早期负荷剂量阿托伐他汀治疗血脂正常的急性非ST段抬高型心肌梗死疗效观察
2014-07-18贾新未王艳飞
张 晶,贾新未,王艳飞
早期负荷剂量阿托伐他汀治疗血脂正常的急性非ST段抬高型心肌梗死疗效观察
张 晶,贾新未,王艳飞
目的探讨早期应用负荷剂量阿托伐他汀对血脂正常的急性非ST段抬高型心肌梗死(non-ST-segment elevation acut myocardial infarction,NSTEMI)患者的临床疗效及安全性。方法将血脂正常的NSTEMI患者65例,随机分为阿托伐他汀负荷剂量组(A组)33例及常规剂量组(B组)32例,A组给予阿托伐他汀钙片40 mg/d,口服;B组给予阿托伐他汀钙片20 mg/d,口服。分别于治疗前及治疗2周后测定血脂、高敏C-反应蛋白(high-sensitivity C-reactive protein,hs-CRP)、血清脂联素(adiponectin,APN)、肝功能,并且随访6个月,统计严重心血管不良事件(major adverse cardiovascular events,MACE)发生情况。结果与常规剂量组比较,负荷剂量组的总胆固醇(total cholesterol,TCH)、低密度脂蛋白胆固醇(low density lipoprotein cholesterol,LDL-C)、hs-CRP下降更明显,APN较高,且两组肝功能无明显损害。6个月随访,负荷剂量组的MACE发生率少于常规剂量组。结论血脂正常的NSTEMI患者早期应用负荷剂量阿托伐他汀钙片可使炎性反应明显减轻,稳定粥样斑块,并且改善预后。
急性非ST段抬高型心肌梗死;阿托伐他汀钙片;高敏C反应蛋白;血清脂联素
急性冠脉综合征(acute coronary syndrome,ACS)是冠状动脉粥样硬化性心脏病最严重的一种类型,目前认为ACS发病的病理生理基础为易损斑块破裂、血小板聚集和血栓形成。炎性反应在冠状动脉粥样硬化的发生、发展中起着重要作用,冠心病患者早期即出现内皮功能损害[1]。近来研究发现,他汀类药物具有独立于调脂作用以外的多效性作用[2],如抗炎、抗血小板聚集、抑制细胞增殖、改善血管内皮功能等。本研究通过早期应用负荷剂量阿托伐他汀治疗血脂正常的NSTEMI患者,观察治疗前后血脂、hs-CRP、APN水平的变化,探讨负荷剂量阿托伐他汀对稳定斑块、抗炎及改善预后的效果及安全性。
1 对象与方法
1.1 对象 选择2012-01至2013-01在河北大学附属医院心内一科住院的血脂正常NSTEMI患者65例,所有病例均符合《不稳定性心绞痛和非ST段抬高心肌梗死诊断标准》。男48例,女17例,年龄45~65岁,平均(58.6±6.2)岁。随机分为阿托伐他汀负荷剂量组(A组)33例,常规剂量组(B组)32例,两组在年龄、性别、血脂、吸烟比例、血压水平、血糖水平方面比较,差异无统计学意义(P>0.05),具有可比性。
1.2 排除标准 急性感染患者,严重心力衰竭患者,肝肾功能不全者,近3个月有脑卒中病史者,有肌病者,有恶性肿瘤患者,自身免疫性疾病患者,服用非甾体类抗炎药物、糖皮质激素,以及入院4周内服调脂药物患者。
1.3 用药方法 两组均给予NSTEMI常规治疗,A组给予阿托伐他汀钙片40 mg,1次/d,口服;B组给予阿托伐他汀钙片20 mg,1次/d,口服。两组均服药6个月。
1.4 观察指标 两组均于治疗前测定血脂、hs-CRP、APN、肝功能、心肌酶水平,并于治疗2周后复查;随访6个月,统计MACE发生率(包括再发心肌梗死、恶性心律失常、症状性心力衰竭、死亡)。测定血脂、心肌酶、hs-CRP,使用放射免疫分析法(RIA)测定APN。

2 结 果
2.1 治疗前后血脂、hs-CRP、APN比较 两组治疗前血脂、hs-CRP、APN水平无差异,治疗后TCH、LDL-C、hs-CRP水平均较治疗前下降(P<0.05);A组较B组治疗后TCH、LDL-C、hs-CRP水平下降明显,APN升高更明显,差异有统计学意义(P<0.05,表1)。
2.2 不良反应比较 两组患者服药期间反应良好,肝功能无明显损害,未出现肌痛、肌炎及横纹肌溶解现象。随访6个月,A组MACE发生率为15.1%,明显低于B组34.4%,差异有统计学意义(P<0.05,表2)。
3 讨 论
冠状动脉粥样硬化斑块是脂质代谢紊乱、炎性反应、血管内皮损伤共同作用的结果[3]。此类斑块的特点是纤维帽较薄,平滑肌细胞及胶原含量少,核心脂质含量高,以及炎性反应细胞浸润多。他汀类药物通过竞争性抑制肝脏三羟基-三甲基-戊二酰辅酶A还原酶阻断TCH的合成,降低具有致动脉粥样硬化作用的LDL-C。本研究表明,负荷剂量组能更好地降低血TCH、LDL-C,起到调脂、稳定斑块作用。


组别A组(n=33)B组(n=32)TCH(mmol/L) 治疗前4.78±0.334.76±0.36 治疗后4.15±0.36①②4.46±0.26①LDL⁃C(mmol/L) 治疗前3.15±0.203.18±0.15 治疗后2.16±0.29①②2.53±0.30①hs⁃CRP(mg/L) 治疗前19.65±1.3319.32±2.59 治疗后3.05±0.86①②6.18±1.03①APN(mg/L) 治疗前6.866.99 治疗后10.59①②8.36①
注:与治疗前比较,①P<0.05;与B组治疗后比较,②P<0.05
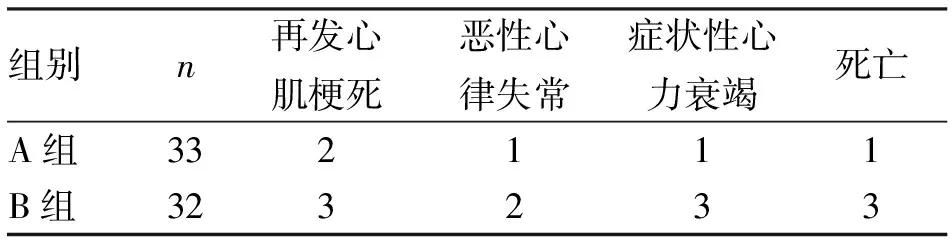
表2 两组NSTEMI患者治疗后发生MACE比较
hs-CRP是肝脏合成的一种非特异性的急性时相反应蛋白,其水平增高是体内存在炎性反应的标志[4],可以由此来推测炎性反应的严重程度,被认为是心血管风险的独立预测因子[5]。本研究证实,在NSTEMI患者应用负荷量阿托伐他汀,能更有效地降低hs-CRP,减轻炎性反应。
APN是一种由脂肪组织分泌的胶原样蛋白,可能对血脂代谢产生一定的作用,目前国内已有研究表明,APN与游离脂肪酸、空腹血糖、体重指数呈负相关[6]。另有研究发现,健康志愿者血中富含APN[7]。国外有研究发现,APN缺乏会增加血栓的发生和血小板的聚集[8]。本研究观察到口服负荷剂量的他汀类药物组较常规剂量组患者APN的水平更高,证明负荷剂量阿托伐他汀可增强其抗动脉粥样、抗炎、促进脂肪代谢等作用。通过对65例NSTEMI患者6个月的随访,笔者发现,早期服用负荷剂量他汀类药物的患者,MACE的发生率明显减少,这得益于他汀类药物降脂、抗炎、改善内皮功能、抗血小板聚集的多效性,与许多实验结果一致[9,10]。
综上所述,无论是否存在血脂异常,在NSTEMI早期应用负荷剂量阿托伐他汀,可明显减低hs-CRP水平,提高APN水平,减少严重心血管事件的发生,改善患者远期预后,且无明显肝功能损害及肌病发生,值得推广应用。
[1] Hsu H Y,Wang P Y,Chen Y T,etal. Changes in flow-mediated dilatation, cytokines and carotid arterial stenosis during aggressive atorvastatin treatment in normocholeste rolemic patients[J].J Chin med Assoc,2005,68(2):53-58.
[2] Lee J M,Choudhury R P.Prospects for atherosclerosis regression through increase in high-density lipoprotein and other emerging therapeutic targets[J].Heart,2007,93(5):559-564.
[3] Rauch U,Osende J I,Chesebro J H.Statins and cardiovascular diseases: the multiple effects lipid-lowing therepy by statins[J].Atheroaclerosis,2000,153(1):181-189.
[4] Kablak Z A,Przewlocki T,Sokolowski A,etal.Carotid intima-media thickness,hs-CRP and TNF-α are independently associated with cardiovascular event risk in patients with atherosclerotic occlusive diease[J].Atherosclerosis,2011,214(1):185-190.
[5] Ridker P M,Refai N,Rose L,etal.Comparison of C-reactive protein and low-density lipoprotein cholesterol levels in the prediction of first cardiovascular events[J].N Engl J Med,2002,347(20):1557-1565.
[6] Gao M,Ding D,Huang J,etal.Association of genetic variants in the adiponectin gene with metabolic syndrome:a case-control study and a systematic meta-analysis in the Chinese population[J].PLoS One,2013,8:e58412.
[7] Dastani Z,Hivert M F,Timpson N,etal.Novel loci for adiponectin levels and their influence on type2 diabetes and metabolic traits:a multi-ethnic mete-analysis of 45,891 individuals[J]. PloS Genet, 2012,8(3):e1002067.
[8] Kato H,Kashiwagi H,Shirage M,etal.Adiponectin acts as an endogenous antithrombotic factor[J].Arterioscler Thromb Vasc Biol,2006,26:224-230.
[9] 刘时武,丁世芳.他汀类药物的非调脂作用[J].华南国防医学杂志,2008,22(2):63-65.
[10] 于 鑫,刘 斌, 魏路清,等.阿托伐他汀对博莱霉素诱导大鼠肺成纤维细胞MMP-9及TIMP-1表达影响[J]. 中国急救复苏与灾害医学杂志, 2012,7(12):1131-1136.
(2014-03-10收稿 2014-06-09修回)
(责任编辑 尤伟杰)
Earlyapplicationofloaddoseofatorvastationtopatientswithnon-ST-segmentelevationacutemyocardialinfarctionwithnornallipids
ZHANG Jing, JIA Xinwei, and WANG Yanfei. Department of cardiovascular medicine one, Affiliated Hospital of Hebei University, Baoding 071000, China
ObjectiveTo ivsetigate the clinical effect and safety of early application of load dose of atorvastation to patients with non-ST-segment elevation acute myocardial infarction with nornal lipids.MethodsA total of 65 patients who were diagnosed as having NSTEMI with nornal lipids were randomly divided into atorvastation load dose group (group A,n=33) and the conventional dose group (group B,n=32).Group A took 40 mg/d atorvastation in addition to routine treatment.Group B took 20 mg/d atorvastation.Blood lipids, high-sensitivity C-reactive protein(hs-CRP)and adiponectin(APN) levels, and liver functions were measured before treatment and after 2 weeks of treatment.Patients were followed up for 6 months. The incidence of major adverse cardiovascular events(MACE) were observed.ResultsThe TCH,LDL-C and hs-CRP levels were decreased more obviously in group A after 2 weeks treatment (P<0.05).while the APN levels were increased more obviously in group A(P<0.05).Obvious liver dysfunctions were not found in both groups. After 6 months,the incidence of MACE was lower in group A than in group B.ConclusionsIn patients with NSTEMI, even with normal blood lipids,taking load dose of atorvastation early can reduce the inflammation response, improve the stabilization of atherosclerotic plaque and improve the prognosis.
non-ST-segment elevation acute myocardial infarction;atorvastation;high-sensitivity C-reactive protein;adiponectin
张 晶,硕士,主治医师,E-mail:zhangjing917@sina.com.cn
071000 保定,河北大学附属医院心内一科
R542.22