锁定钢板与交锁髓内钉治疗肱骨近端骨折的疗效分析
2014-07-05徐小东张殿英付中国王天兵陈建海杨明芦浩
徐小东 张殿英 付中国 王天兵 陈建海 杨明 芦浩
锁定钢板与交锁髓内钉治疗肱骨近端骨折的疗效分析
徐小东 张殿英 付中国 王天兵 陈建海 杨明 芦浩
目的分析比较锁定钢板与交锁髓内钉治疗肱骨近端骨折的治疗结果。方法对2012年1月至2013年5月的38例肱骨近端骨折患者进行回顾性分析。根据治疗方法分为锁定钢板组(24例)与交锁髓内钉组(14例)。结果所有患者均获得随访,时间为9~23个月(平均16.1个月)。两组患者在切口长度、手术时间和并发症发生率方面差异有统计学意义(t=8.857、5.323、2.460,P均<0.05),锁定钢板组患者并发症发生率低,交锁髓内钉组患者切口小、手术时间短;两组患者在颈干角、骨折愈合时间方面差异无统计学意义(t=0.548、0.459,P均>0.05);锁定钢板组患者的前举范围、Constant-Murley肩关节功能评分、优良率均高于交锁髓内钉组,但差异无统计学意义(t=1.470、0.905、0.133,P均>0.05)。结论锁定钢板和交锁髓内钉治疗肱骨近端骨折各有优势,如适应证合适,经过规范的手术治疗均可取得良好的治疗结果。
肱骨骨折,近端;交锁髓内钉;锁定钢板;治疗结果
肱骨近端骨折常见于老年骨质疏松患者,年轻人骨折多见于高能量损伤。对于不稳定或者明显移位骨折常采用手术治疗。切开复位锁定钢板固定和闭合复位交锁髓内钉固定是治疗肱骨近端骨折两种常见的治疗方法[1-3]。本文对采用锁定钢板与交锁髓内钉治疗肱骨近端骨折的病例进行回顾性分析。
资料与方法
一、一般资料
随机选取我科2012年1月至2013年5月有完整资料的应用锁定钢板或交锁髓内钉治疗的肱骨近端骨折患者38例,其中男性13例,女性25例。年龄20~86岁,平均(66.5±16.9)岁。所有患者均为单侧闭合性骨折,左侧21例,右侧17例。低能量损伤28例,滑雪、车祸等高能量损伤10例。锁定钢板组24例,交锁髓内钉组14例。按Neer分型:锁定钢板组中2部分骨折7例,3部分骨折11例,4部分骨折6例;交锁髓内钉组中2部分骨折8例,3部分骨折5例,4部分骨折1例;按AO分型:锁定钢板组中11-A型4例,11-B型14例,11-C型6例;交锁髓内钉组中11-A型7例,11-B型6例,11-C型1例(表1,2)。术中使用Synthes公司的PHILOS钢板和Smith&Nephew公司的TRIGEN髓内钉。

表1 两组患者的一般情况统计

表2 两组患者的骨折分型及术中情况
二、手术方法
患者麻醉后取沙滩椅位。锁定钢板组:采用三角肌 胸大肌间隙入路,暴露骨折端后,清理关节囊积血,将骨折块复位,克氏针临时固定,C臂X线机辅助复位满意后放置钢板固定,对于3部分和4部分骨折,缝合固定大小结节并注意植骨。交锁髓内钉组:行肩峰前外侧切口,纵行劈开肩袖,保护肩袖后显露肱骨头。在透视引导下行手法及克氏针撬拨复位,选择结节间沟后方肱骨头和大结节交界处为进针点,置入合适髓内钉,并尽量使尾端没入骨质内,近端和远端锁定,安装尾帽,仔细缝合肩袖,缝合包扎伤口[4]。
三、功能锻炼
术后吊带支具固定患肢,根据全身状况、骨折类型及手术固定情况指导术后康复锻炼。术后第2天或拔除引流管后即开始被动活动锻炼,包括钟摆样运动和被动前屈、外旋锻炼,并逐渐被动内旋、内收和外展活动。术后复查X线片如见骨痂或骨折愈合后主动活动锻炼,可加强伸屈、旋转及收展活动锻炼,约3个月后开始肩部力量锻炼并加强活动范围练习[5]。
四、随访及评估
内容包括:(1)定期复查并行Constant-Murley肩关节功能评分;(2)影像学检查:标准X线片(肩胛骨正侧位、腋位);(3)采用Constant-Murley肩关节功能评分评定优良率,总分100分,90分以上为优,80~89分为良,70~79分为可,70分以下为差。优良率=优良例数/总例数×100%。内翻畸形愈合标准:肱骨颈干角<120°[6-7]。
五、统计学分析
计量资料以x-±s表示,应用SPSS 13.0统计软件,两组比较采用独立样本t检验,计数资料采用χ2检验,P<0.05为差异有统计学意义。
结 果
所有患者均获随访,随访时间为9~23个月,平均16.1个月。锁定钢板组与交锁髓内钉组的平均手术时间(小时)分别为89.4±14.8与65.7±10.3(t=5.323,P<0.05),平均切口长度(mm)分别为10.3±3.1与2.7±1.1(t=8.857,P<0.05),差异有统计学意义。
根据术后X线片和Constant-Murley肩关节功能评分:锁定钢板组与交锁髓内钉组患者的初次颈干角分别为(139.2±6.40)°与(137.9±7.04)°(t=0.644,P>0.05);末次颈干角分别为(134.7±8.0)°与(133.3±6.42)°(t=0.548,P>0.05),平均下降度数分别为4.5°与4.6°,两组间差异无统计学意义;锁定钢板组与交锁髓内钉组的前举范围为(146.2±25.3)°与(135.7±36.3)°(t=1.470,P>0.05);肩关节评分为(82.9±16.7)分与(77.6±19.2)分(t=0.905,P>0.05);优良率为83.3%与78.6%,前者优于后者,但差异无统计学意义(χ2=0.133,P>0.05)(表3)。
表3 两组患者预后情况统计(±s)
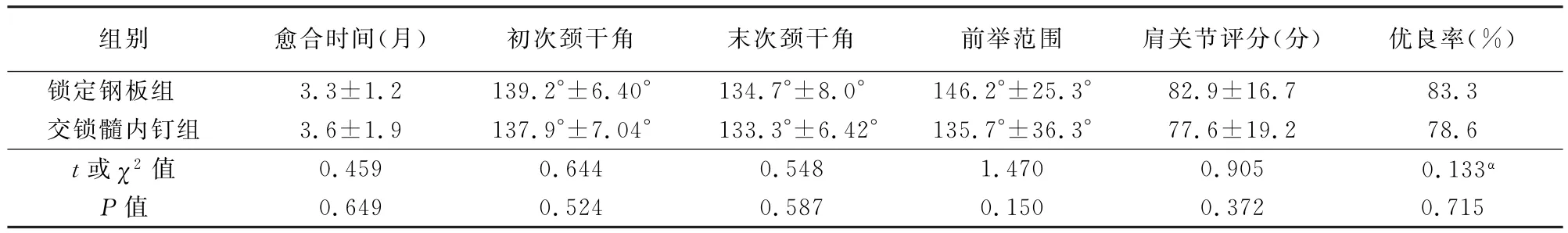
表3 两组患者预后情况统计(±s)
注:α为χ2值
组别 愈合时间(月) 初次颈干角 末次颈干角 前举范围 肩关节评分(分) 优良率(%)锁定钢板组 3.3±1.2 139.2°±6.40° 134.7°±8.0° 146.2°±25.3° 82.9±16.7 83.3交锁髓内钉组 3.6±1.9 137.9°±7.04° 133.3°±6.42° 135.7°±36.3° 77.6±19.2 78.6t或χ2值 0.459 0.644 0.548 1.470 0.905 0.133α0.649 0.524 0.587 0.150 0.372 0.715P值
锁定钢板组并发症:内翻畸形愈合2例,螺钉切出1例,退钉1例,肩峰撞击综合征1例;交锁髓内钉组的并发症:内翻畸形愈合2例,延迟愈合1例,肩峰撞击综合征2例;锁定钢板组并发症发生率为20.8%,交锁髓内钉组并发症发生率为35.7%,差异有统计学意义(χ2=2.46,P<0.05),见表4。其中交锁髓内钉组有1例2部分骨折患者在每月复查过程中出现颈干角降低后再升高的变化,初次、再次和末次颈干角分别为142.7°、122.8°和130.9°。经过吊带固定后于术后7个月畸形愈合。
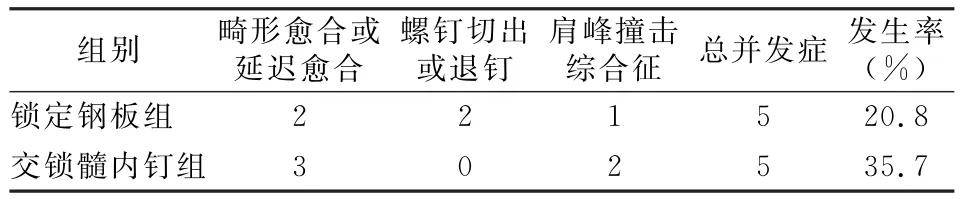
表4 两组患者并发症统计
讨 论
肱骨近端骨折的常见手术治疗方法包括锁定钢板内固定和交锁髓内钉内固定[8]。锁定钢板的螺钉为锁定设计,可提供角稳定性;螺钉较多,固定体积相对大而全面;螺钉相互成角,把持力强,抗拔出阻力大;锁定钢板有限接触骨膜组织,一定程度上保护骨折断端及周围血运。但锁定钢板为髓外偏心固定,固定力臂大,抗内收力量差,对某些内侧皮质粉碎、缺损或复位不良的患者,术后可出现内翻畸形、螺钉切割甚至穿出肱骨头的情况[9-10]。
交锁髓内钉为髓内中心性固定,固定力臂小,初始稳定性强,有良好的抗屈曲和抗旋转特性;闭合复位,剥离软组织少,骨折断端血运破坏小;交锁髓内钉近端可平行或垂直多向锁定,可避免在固定失败时螺钉穿入关节腔[11-12]。但是交锁髓内钉近端螺钉数量相对较少,单位体积螺钉数量少,骨块把持力下降;进针点处的医源性骨折、肩袖撕裂、神经血管损伤等也是其缺陷。
交锁髓内钉组患者在切口大小和手术时间方面具有明显优势,手术操作快,皮肤切口小更易被患者接受。任世祥等[13]研究发现,锁定钢板和交锁髓内钉治疗肱骨近端骨折均可取得较好的效果,并且后者具有切口小、操作简单的优点。
锁定钢板组患者平均前臂上举范围比交锁髓内钉组大,但差异无统计学意义,这与交锁髓内钉损伤肩袖有一定关系,但不起决定性作用。目前采用的交锁髓内钉更直、更细,入钉点对肩袖的损伤明显减小,如入钉点近内侧,经冈上肌肌腹入针,肩袖损伤减少。同时肩关节功能与规范的术后康复功能锻炼密切相关[11]。Lekic等[3]研究发现,锁定钢板和交锁髓内钉治疗的患者术后6个月的上举范围平均达到141°与134°,锁定钢板组患者的活动范围比交锁髓内钉组好,但是两者之间比较差异无统计学意义。
锁定钢板组患者和交锁髓内钉组在优良率和肩关节评分方面差异无统计学意义。影响预后的因素很多,如年龄、一般状况、骨折类型、内固定方式、术者熟练程度、康复功能锻炼等。Konrad等[1]研究发现,锁定钢板和交锁髓内钉的临床治疗效果类似,手术技巧和经验是手术成功的关键。von Rüden等[2]研究发现,不同的骨折类型、年龄和内固定物在长期临床和影像学随访中没有发现明显差异,交锁髓内钉和锁定钢板都是较好的肱骨近端骨折治疗方法。
颈干角<120°即内翻畸形和内固定丢失之间有密切联系,见于各种内固定的肱骨近端骨折术后[6-7]。本研究中两组患者初次颈干角均比末次颈干角有一定程度的下降,颈干角大小及随访过程中的下降程度差异无统计学意义。交锁髓内钉组有1例患者:女性,80岁,3部分骨折,出现颈干角波动性变化,可能与交锁髓内钉固定单位面积的螺钉数量相对少、骨质疏松等导致螺钉把持能力下降,固定不牢固,导致复位丢失有关,此种情况应该慎重选择交锁髓内钉固定。
锁定钢板组患者肱骨近端内侧皮质粉碎,骨块难以复位固定,内侧皮质支撑失败,造成肱骨头进行性内翻并最终出现内翻畸形和螺钉切出[4,14-15],术中对于肱骨头内翻的复位和维持内侧皮质支撑作用是避免术后内翻畸形发生的关键[6]。交锁髓内钉虽然是髓内固定、力臂短、抗屈曲能力强,但是如果患者的骨质疏松严重,肱骨头内骨质空虚,植骨困难,难以维持内侧皮质支撑;而交锁髓内钉螺钉数量相对少,对部分骨折块的把持作用有限,尤其对老年骨质疏松性3或4部分骨折,不易稳定固定肱骨头。本次研究中交锁髓内钉组并发症的发生率明显高于锁定钢板组,与这些因素有密切关系。
肱骨近端骨折为关节周围骨折,应该解剖复位,平整关节面,恢复关节及内侧皮质力线,并坚强固定,以维持肱骨近端的形态并保护血运,以利于早期功能锻炼和骨折愈合[6,16]。锁定钢板和交锁髓内钉治疗都是可行的治疗方法,把握各自的适应证,是提高手术疗效的重要因素。对于2部分或3部分骨折且无骨质疏松的年轻患者,可采用锁定钢板或交锁髓内钉固定[17]。对于2部分外科颈和肱骨干骨折,可采用交锁髓内钉固定[18],对于交锁螺钉难以把持的结节骨折以及4部分骨折谨慎采用[19],但最新交锁髓内钉的设计和性能越来越完善,交锁髓内钉固定的适应证也将进一步扩展。对骨质情况良好的3部分或部分4部分老年骨折患者,可以采取锁定钢板固定[18]。对于部分3部分或4部分骨折,尤其是伴有严重骨质疏松的老年患者,血运破坏非常严重,肱骨头中心骨量很少,螺钉难以把持而且容易出现不稳定现象,尤其是内侧皮质缺损或者复位困难的患者应该选择肩关节置换治疗[4,17,20]。总之,应该综合患者年龄、骨量、骨折类型、粉碎程度、碎片数量与位置等因素,选择合适的手术适应证,制定个体化的治疗方案,并不断提高手术技术和熟练程度,规范康复功能锻炼,才能不断提高预后。
本研究的缺点:分组病例较少,没有对肱骨近端骨折各个分型的预后及并发症等对比分析。
[1] Konrad G,AudigéL,Lambert S,et al.Similar outcomes for nail versus plate fixation of three-part proximal humeral fractures[J].Clin Orthop Relat Res,2012,470(2):602-609.
[2] von Rüden C,Trapp O,Hierholzer C,et al.Intramedullary nailing vs.locking plate osteosynthesis in proximal humeral fractures:Long-term outcome[J].Unfallchirurg,2014,In gress.
[3] Lekic N,Montero NM,Takemoto RC,et al.Treatment of two-part proximal humerus fractures:intramedullary nail compared to locked plating[J].HSS J,2012,8(2):86-91.
[4] 姜保国,白露,张培训,等.肱骨近端骨折的手术治疗[J].中华创伤骨科杂志,2009,11(5):404-407.
[5] 姜保国,付中国,张殿英,等.肱骨近端骨折的外科治疗及术后康复[J].中华创伤杂志,2002,18(3):133-135.
[6] 付中国,徐春归,芦浩,等.累及干骺端及肱骨干的肱骨近端骨折的手术治疗[J].北京大学学报:医学版,2012,44(6):887-890.
[7] Agudelo J,Schürmann M,Stahel P,et al.Analysis of efficacy and failure in proximal humerus fractures treated with locking plates[J].J Orthop Trauma,2007,21(10):676-681.
[8] Jo MJ,Gardner MJ.Proximal humerus fractures[J].Curr Rev Musculoskelet Med,2012,5(3):192-198.
[9] 张亮,陈统一.肱骨近端三或四部分骨折治疗方式选择[J].国际骨科学杂志,2010,31(2):83-85.
[10] Haidukewych GJ.Innovations in locking plate technology[J].J Am Acad Orthop Surg,2004,12(4):205-212.
[11] 俞银贤,吴晓明,王秋根.交锁髓内钉治疗肱骨近端骨折[J].中华创伤骨科杂志,2012,14(12):1092-1094.
[12] Hessmann MH,Hansen WS,Krummenauer F,et al.Locked plate fixation and intramedullary nailing for proximal humerus fractures:a biomechanical evaluation[J].J Trauma,2005,58(6):1194-1201.
[13] 任世祥,林源,曲铁兵,等.交锁髓内钉与锁定钢板治疗肱骨近端骨折的疗效研究[J].中华创伤骨科杂志,2011,13(10):937-939.
[14] Gardner MJ,Weil Y,Barker JU,et al.The importance of medial support in locked plating of proximal humerus fractures[J].J Orthop Trauma,2007,21(3):185-191.
[15] Osterhoff G,Baumgartner D,Favre P,et al.Medial support by fibula bone graft in angular stable plate fixation of proximal humeral fractures:an in vitro study with synthetic bone[J].J Shoulder Elbow Surg,2011,20(5):740-746.
[16] Helmy N,Hintermann B.New trends in the treatment of proximal humerus fractures[J].Clin Orthop Relat Res,2006,442:100-108.
[17] 金晨,陆雄伟,朱彤,等.肱骨近端骨折的手术策略[J].医学临床研究,2008,25(9):1610-1613.
[18] 张睿,陈云丰.肱骨近端骨折的手术治疗进展[J].实用骨科杂志,2010,16(1):41-44.
[19] Füchtmeier B,Bröckner S,Hente R,et al.The treatment of dislocated humeral head fractures with a new proximal intramedullary nail system[J].Int Orthop,2008,32(6):759-765.
[20] Hertel R,Fandridis E.(iii)post-traumatic Reconstruction for sequelae of fractures of the proximal humerus[J].Curr Orthop,2007,21(6):422-431.
Treatment of proximal humeral fractures with interlocking intramedullary nail versus locking plate
Xu Xiaodong,Zhang Dianying,Fu Zhongguo,Wang Tianbing,Chen Jianhai,Yang Ming,Lu Hao.Department of Trauma and Orthopedics,Peking University People’s Hospital,Peking University Traffic Medicine Center,Beijing 100044,China
BackgroundProximal humeral fracture is usually seen in elder citizens with osteoporosis,and such a fracture in younger patients mainly results from high-energy injury.Surgical procedure is often adopted for patients with unstable or obviously displaced fracture.Open reduction and locking plate fixation or closed reduction and interlocking intramedullary nail fixation are two common treatment methods for proximal humeral fracture.In this paper,retrospective analysis was conducted to compare the clinical curative effects between locking plate and intramedullary nail in the treatment of proximal humeral fracture.MethodsGeneral data:From January 2012 to May 2013,38 patients with full information in our department were randomly selected in the retrospective analysis,including 13 male and 25 female,aged from 20 to 86,and the mean age was 66.5±16.9 years.According to the different treatment methods,the patients were divided into the locking plate group(24 cases)and the interlocking intramedullary nail group(14 cases).All patients had unilateral closed fractures treated with locking plate or interlocking intramedullary nail,including 22 cases on the left side and 17 cases on the right side.28 patients were injured from low energy falls and 10 cases were from high energy trauma like skiing,motor accidents,etc.According to Neer classification,7 cases of two-part fracture,11 cases of three-part fracture and 6 cases of four-part fracture were in the locking plate group,and 8 cases of two-part fracture,5 cases of three-part fracture and 1 case of four-part fracture were in the interlocking intramedullary nail group.In the meanwhile,on the basis of AO classification,4 type 11-A cases,14 type 11-B cases and 6 type 11-C cases were in the locking plate group,and 7 type 11-A cases,6 type 11-B cases and 1 type 11-C case were in the interlockingintramedullary group.PHILOS plate of Synthes,Inc.and TRIGEN intramedullary nail of Smith&Nephew,Inc.were used in the operation.Operation methods:After successful anesthesia,the patient was placed in beach chair position.Locking plate group:Deltoid pectoralis major muscle gap approach was applied to expose the fracture end.Clean up the hematocele in the joint capsule,reduce the bone fragments and use Kirschner wire for temporary fixation.Plate fixation was done after successful C-arm fluoroscopy assisted reduction.The greater and lesser tubercles of humerus were sutured with bone graft for three and four-part fracture.Interlocking intramedullary nail group:Anterolateral incision on the acromion was made to split the rotator cuff longitudinally,and then protect the acromion and expose the humeral head.Manual or Kirschner wire poking reduction was done under fluoroscopic guidance.Choose the junction of humeral head behind intertubercular sulcus and the greater tubercles of humerus as the entry point,insert the proper nail and make sure that the nail tail was in the bone before locking the proximal and distal screws.After installing the tail cap,closely suture the rotator cuff and then stitch and bind up the wound.Functional training:The affected limb was fixed with forearm sling brace after operation.Postoperative functional training is guided on the basis of general condition,fracture type and state of surgical fixation.With the drainage tube extracted,passive movement is initiated on the second day after surgery,including pendular movement,passive anteflexion and external rotation,and then gradual passive internal rotation,adduction and abduction.With signs of callus or fracture healing seen on postoperative X-ray films,we should encourage active movement and enhance the exercises of flexion and extension,rotation,adduction and abduction,etc.The training of shoulder strength starts 3 months later,with the intensified exercises for range of motion.Follow-ups and evaluation:The content includes:(1)Regular return visit and evaluation of shoulder function with Constant-Murley score;(2)Imaging examinations:standard X-ray films(anteroposterior view of scapula,axillary view);(3)Excellent rate of shoulder function is assessed with Constant-Murley score.The total score is 100 points,regarding 90 points and above as better,80-89 as good,70-79 as normal and 70 points below as poor.The excellent rate=excellent case number/total case number*100%.The standard of varus malunion:humeral neck shaft angle is smaller than 120°.Statistical analysis Measurement data is expressed asx-±swith SPSS 13.0 statistical software,using independent samples t test.Theχ2 test is adopted for enumeration data.P<0.05 is considered as statistical difference.Results(1)All the patients were followed up for 9-23 months with an average of 16.1 months.The mean operation time(minute)of plate group and intramedullary nail group were 89.4±14.8 and 65.7±10.3(t=5.323,P<0.05).The average length of incisions(mm)were 10.3±3.1 and 2.7±1.1(t=8.857,P<0.05).The two indices above had statistically significant difference.(2)Assessment was based on post-operative X-ray film and Constant-Murley scoring system of shoulder joint function:The initial neck shaft angles in plate group and intramedullary nail group were 139.2°±6.40°and 137.9°±7.04°(t=0.644,P>0.05);the last neck shaft angles in plate group and intramedullary nail group were 134.7°±8°and 133.3°±6.42°(t=0.548,P>0.05)with the average decline degrees respectively 4.5°and 4.6°,and there was no statistical difference between the two groups.The ranges of forward elevation in locking plate group and intramedullary nail group were respectively 146.2°±25.3°and 135.7°±36.3°(t=1.470,P>0.05);the shoulder scores were 82.9±16.7 and 77.6±19.2(t=0.905,P>0.05);the excellent rates were 83.3%and 78.6%with the former better than the latter,but no statistical difference was found(χ2=0.133,P>0.05).(3)Complications of plate group:2 cases of varus malunion,1 case of screw cut-out,1 case of screw withdrawal and 1 case of subacromial impingement syndrome;Complications of intramedullary nail group:2 cases of varus malunion,1 case of delayed union and 2 cases of acromion impingement syndrome;The incidence rate of complications in plate group was 20.8%and that in intramedullary nail group was 35.7%(χ2=2.46,P<0.05)with statistical difference.Details are seen in table 4.In a two-part fracture case of intramedullary nail group,the changes of neck shaft angle appeared as increase after decline during monthly review,and the initial-second-last neck shaft angles were 142.7°,-122.8°,-130.9°.This patient had malunion with the affected arm fixed in a sling for 7months after surgery.ConclusionsBoth the interlocking intramedullary nail fixation and the locking plate fixation have the merits in treatment of proximal humeral fractures.Choosing proper indications,we can get excellent curative outcomes after operation and rehabilitation.
Humeral fractures,proximal;Nail;Plate;Treatment outcome
Zhang Dianying,Email:zdy8016@163.com
2014-03-10)
(本文编辑:李静)
10.3877/cma.j.issn.2095-5790.2014.04.005
卫生公益性行业科研专项(201002014);教育部创新团队(IRT1201)
100044 北京大学人民医院创伤骨科 北京大学交通医学中心
张殿英,Email:zdy8016@163.com
徐小东,张殿英,付中国,等.锁定钢板与交锁髓内钉治疗肱骨近端骨折的疗效分析[J/CD].中华肩肘外科电子杂志,2014,2(4):230-234.