Pancreatic fistula after central pancreatectomy: case series and review of the literature
2014-05-04YanMingZhouXiaoFengZhangLuPengWuXuSuBinLiandLeHuaShi
Yan-Ming Zhou, Xiao-Feng Zhang, Lu-Peng Wu, Xu Su, Bin Li and Le-Hua Shi
Xiamen, China
Pancreatic fistula after central pancreatectomy: case series and review of the literature
Yan-Ming Zhou, Xiao-Feng Zhang, Lu-Peng Wu, Xu Su, Bin Li and Le-Hua Shi
Xiamen, China
BACKGROUND:Postoperative pancreatic fistula is one of the most common complications after pancreatectomy. This study aimed to assess the occurrence and severity of pancreatic fistula after central pancreatectomy.
METHODS:The medical records of 13 patients who had undergone central pancreatectomy were retrospectively studied, together with a literature review of studies including at least five cases of central pancreatectomy. Pancreatic fistula was defined and graded according to the recommendations of the International Study Group on Pancreatic Fistula (ISGPF).
RESULTS:No death was observed in the 13 patients. Pancreatic fistula developed in 7 patients and was successfully treated nonoperatively. None of these patients required re-operation. A total of 40 studies involving 867 patients who underwent central pancreatectomy were reviewed. The overall pancreatic fistula rate of the patients was 33.4% (0-100%). Of 279 patients, 250 (89.6%) had grade A or B fistulae of ISGPF and were treated nonoperatively, and the remaining 29 (10.4%) had grade C fistulae of ISGPF. In 194 patients, 15 (7.7%) were re-operated upon. Only one patient with grade C fistula of ISGPF died from multiple organ failure after re-operation.
CONCLUSION:Despite the relatively high occurrence, most pancreatic fistulae after central pancreatectomy are recognized a grade A or B fistula of ISGPF, which can be treated conservatively or by mini-invasive approaches.
(Hepatobiliary Pancreat Dis Int 2014;13:203-208)
pancreas;
central pancreatectomy;
pancreatic fistula
Introduction
Postoperative pancreatic fistula is one of the most common complications after pancreatectomy, often resulting in intra-abdominal abscess and bleeding, wound infection, respiratory complications, sepsis, and prolonged postoperative hospitalization.[1-16]Since the first report of central pancreatectomy (CP) in 1957, it has been increasingly used to remove benign or low-grade malignant tumors located in the neck and body of the pancreas. Unlike other conventional major pancreatic resections, CP has the advantages of preserving the integrity of the gastrointestinal tract and splenic function and sparing maximal pancreatic endocrine and exocrine function by avoiding extended resection of the pancreas.[17-20]However, the high pancreatic fistula rate has been one of the major shortcomings of the procedure.[20-23]The introduction of the International Study Group on Pancreatic Fistula (ISGPF) definition offers a standardized way to document pancreatic fistula related complications.[16]This study aimed to assess the occurrence and severity of pancreatic fistula after CP.
Methods
Patients
The medical records of 13 patients who had undergone CP between January 2006 and July 2011 were retrospectively reviewed. Informed consent was obtained from these patients and the study was approved by the Ethics Committee of our hospital. In this series, 5 were men and 8 women, with a mean age of 42.1 years (27-64). Preoperative computed tomography and ultrasonography were routinely performed in all patients to determine the size and location of the tumors and to determine potential indications for CP.
Surgical procedure
Surgery was performed through a midline incisionat the upper abdomen to open the lesser sac and expose the anterior face of the pancreas by dividing the adhesion between the posterior surface of the stomach and the pancreas. The pancreatic lesion was resected using electrocautery with a margin of at least 1 cm to cut both sides of the pancreas. Specimens taken from surgical margins were frozen and assessed intraoperatively. The proximal pancreatic stump was over-sewed with interrupted non-absorbable 4-0 suture after ligation of the identified main pancreatic duct. The distal pancreatic stump was reconstructed by retrocolic end-to-side dunking Roux-en-Y pancreaticojejunostomy. Before abdominal closure, an intra-abdominal drainage tube was placed around the surgical field.
Literature review
A literature search was performed using PubMed database from 1966 to June 2012. Search terms were "central pancreatectomy", "medial pancreatectomy", "middle segment pancreatectomy", and "median pancreatectomy". Only studies with at least five cases of CP published in the English language were included. Letters, reviews, abstracts, editorials, expert opinions, non-English language papers and animal studies were excluded. In the case of multiple publications of a given cohort of patients, only the most recent one was used.
Two investigators (ZYM and ZXF) independently reviewed all the retrieved studies that met the inclusion and exclusion criteria. Discrepancies between the two reviewers were resolved by discussion and consensus. The two reviewers extracted data on the following categories: first author, year of publication, study design, patient demographic characteristics, incidence and severity of pancreatic fistula. Pancreatic fistula was defined and graded according to the recommendations of the ISGPF.[16]
Results
Our experience
The mean operative time of the 13 patients was 186 minutes (160-280), and the mean intraoperative blood loss was 450 mL (100-1600). Three patients required blood transfusion. The spleen was preserved in all patients.
There was no death. Eight of the 13 patients developed postoperative complications. Pancreatic fistula was the main complication, occurring in 7 patients. According to the ISGPF definition, all the 7 patients with pancreatic fistula belonged to grade B. Of these patients, 5 patients with fistulae were managed by delayed removal of surgical drains. Two fistulae with intra-abdominal fluid collection were managed by percutaneous drainage with total parenteral nutrition. No patient required re-operation. The mean length of hospital stay was 26 days (14-47).
Final pathology revealed 6 patients suffered from serous cystadenoma, 3 from mucinous cystadenoma, 2 from branch-duct intraductal papillomary-mucinous neoplasms, 1 from nonfunctioning islet cell adenoma, and 1 from chronic pancreatitis. All resection margins were microscopically negative. No patient developed new onset diabetes or exocrine pancreatic insufficiency during a median follow-up period of 17 months (6-64). One patient with chronic pancreatitis had preoperative diabetes, which did not worsen after surgery. There was no neoplastic recurrence.
Literature review
Forty studies involving 867 patients (including the present series) met the inclusion criteria and were included for review.[17-55]An overview of these studies is shown in Table. All these studies were observational. The sample size of each study varied from 5 to 100 patients. The overall pancreatic fistula rate of the patients was 33.4% (0-100%). Of them, 89.6% (250/279) had grade A or B fistulae of ISGPF, all of which were managed successfully non-operatively; 10.4% (29/279) had grade C fistulae of ISGPF. The re-operative rate in all patients was 7.7% (15/194). Only one patient with grade C fistula of ISGPF died several days after reoperation from multiple organ failure, resulting in an overall mortality rate of 0.3% (1/290).
The source of fistula was identified in only 19 patients: 7 from the proximal remnant and 12 from the distal pancreatic anastomosis.[17,20,23,30,31,52]All 7 fistulae originating from the proximal remnant were grade A or B fistulae of ISGPF. In contrast, 5 of 12 leakages from the distal pancreatic anastomosis were due to grade C fistulae of ISGPF, and were treated by re-operation. One patient subsequently died from multiple organ failure.
Discussion
Traditionally, enucleation or formal pancreatectomy is the treatment of choice for benign or borderline lesions of the neck and body of the pancreas. However, enucleation is not always applicable because of the lesion size and location. Besides, this surgical procedure runs a high risk of injury to the main pancreatic duct. Formal pancreatectomy, including pancreatoduodenectomy (PD) and distal pancreatectomy, may sacrifice thenormal pancreatic parenchyma and can be associated with the risk of postoperative diabetes mellitus, exocrine and endocrine pancreatic insufficiency. CP represents an organ-preserving operation. This modality has the advantages of preserving the integrity of the gastrointestinal tract and splenic function, and sparing the maximal pancreatic endocrine and exocrine function by avoiding extended resection of the pancreas.[17-20]
However, these benefits may be outweighed by the greater pancreatic fistula rate associated with CP. The overall pancreatic fistula rate was 33.4% in the current collective review of 867 patients who underwent CP. It was reported that the fistula rate after CP was significantly higher than that after PD or distal pancreatectomy,[1-15]because there are two transectedpancreatic surfaces in CP, thus potentially facilitating the formation of pancreatic fistula. On the other hand, indications for CP are generally limited to benign or low-grade malignant neoplasms. The soft remnant pancreas and the small main pancreatic duct become established risk factors associated with the development of pancreatic fistula.[56]
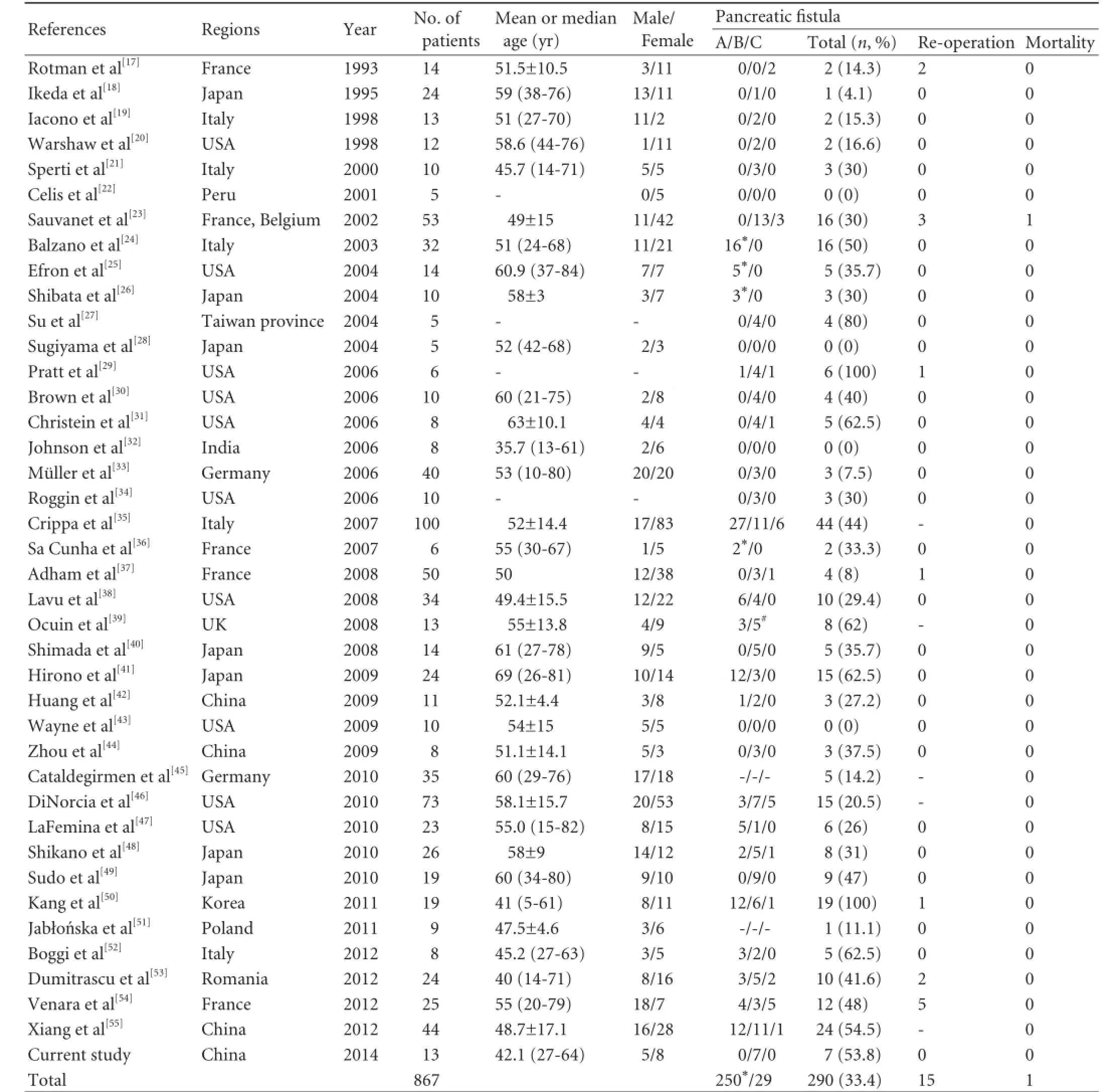
Table.Literature review on the occurrence and severity of pancreatic fistula after central pancreatectomy
According to the ISGPF definition, grade A or B fistulae can be managed successfully by conservative measures or mini-invasive approaches, while grade C fistulae may induce life-threatening complications and often requires re-operation for definitive management.[16]Despite the relatively high occurrence of postoperative pancreatic fistula in our patients, most pancreatic fistulae after CP were grade A or B fistulae of ISGPF, and only 10.4% were grade C fistulae. This figure is lower than that of PD. A recent systematic review of 2706 PD cases reported that grade C pancreatic fistula accounted for 15% of all their 479 cases of pancreatic fistulae.[57]Pratt,[29]Hirono,[41]DiNorcia,[46]Xiang[55]and their colleagues consistently demonstrated that the occurrence of grade C fistulae of ISGPF with CP was similar to that with distal pancreatectomy. These data indicate that CP does not seem to increase the severity of fistula.
According to literature review, the leakage from the distal pancreatic anastomosis is likely to cause more severe clinical consequences. Recently, an Italian group described inframesocolic pancreatojejunostomy after CP, where the cut end of the distal pancreatic stump after CP was brought in the inframesocolic compartment through a small transverse mesocolic window.[52]Pancreatojejunostomy was hence constructed in the intraperitoneal compartment, being divided by the retroperitoneal proximal pancreatic stump by the transverse mesocolon itself. Segregation of the two pancreatic stumps into different body compartments allows for selective identification of the source of a fistula.
Pancreaticojejunostomy and pancreaticogastrostomy are two commonly preferred methods for reconstruction of the distal pancreatic remnant. Sauvanet et al[23]and Brown et al[30]groups found that both techniques had an equivalent fistula rate in CP. Xiang et al[55]reported that pancreaticogastrostomy for the distal pancreatic remnant reduced the occurrence of pancreatic fistula, whereas Venara et al[54]showed a lower anastomotic leakage rate with pancreaticojejunostomy. Therefore, controversies still exist over ideal distal pancreatic anastomosis. Wayne et al[43]reported that there was no pancreatic leakage in a series of 10 patients who underwent CP without pancreatico-enteric anastomosis. However, their conclusion needs to be confirmed by further studies of other centers.
Indications for CP include various benign and borderline tumors (neuroendocrine, serous and mucinous cystadenomas, non-invasive intraductal mucinous producing tumors, solid pseudopapillary tumors) and chronic pancreatitis with segmental stenosis of Wirsung's duct.[51]The technique is contraindicated for malignant lesions owing to limited oncological radicality. In case of invasive malignancy as confirmed by intraoperative histopathological examinations, the operation should be extended as a proximal or distal pancreatic resection.
In conclusion, despite the relatively high occurrence of pancreatic fistula after CP, most cases were grade A or B fistulae of ISGPF that can be managed successfully by conservative measures or mini-invasive approaches. It appears that fistulae originating from distal pancreatic anastomosis have poorer clinical consequences as compared with those originating from the proximal remnant. A recent meta-analysis showed that external pancreatic duct stenting could reduce the occurrence and severity of pancreatic fistula after pancreatic resection.[58]This technical modification has the advantages of diverting away pancreatic juice from the anastomosis and preventing activation of pancreatic enzymes by enterokinase in the small bowel mucosa soon after surgery. In a prospective randomized trial involving 158 patients with a high risk of fistula (soft pancreas and a non-dilated pancreatic duct), Pessaux et al[56]found that external pancreatic duct stenting decreased the pancreatic fistula rate after PD, because the pancreas is soft and the main pancreatic duct is nondilated in most cases of CP. It is expected that external drainage of the pancreatic duct may be particularly helpful in reducing the occurrence of pancreatic fistula in patients undergoing CP, though it needs verification in further study.
Contributors:ZYM and LB participated in the design and coordination of the study, carried out the critical appraisal of studies and wrote the manuscript. ZXF, WLP, SX and SLH developed the literature search, carried out the extraction of data, and assisted in the critical appraisal of included studies. All authors read and approved the final manuscript. LB is the guarantor.
Funding:None.
Ethical approval:This study was approved by the Ethics Committee of our hospital.
Competing interest:No benefits in any form have been received or will be received from a commercial party related directly or indirectly to the subject of this article.
1 van Berge Henegouwen MI, De Wit LT, Van Gulik TM, Obertop H, Gouma DJ. Incidence, risk factors, and treatmentof pancreatic leakage after pancreaticoduodenectomy: drainage versus resection of the pancreatic remnant. J Am Coll Surg 1997;185:18-24.
2 Peng SY, Mou YP, Liu YB, Su Y, Peng CH, Cai XJ, et al. Binding pancreaticojejunostomy: 150 consecutive cases without leakage. J Gastrointest Surg 2003;7:898-900.
3 Dong X, Zhang B, Kang MX, Chen Y, Guo QQ, Wu YL. Analysis of pancreatic fistula according to the International Study Group on Pancreatic Fistula classification scheme for 294 patients who underwent pancreaticoduodenectomy in a single center. Pancreas 2011;40:222-228.
4 Daskalaki D, Butturini G, Molinari E, Crippa S, Pederzoli P, Bassi C. A grading system can predict clinical and economic outcomes of pancreatic fistula after pancreaticoduodenectomy: results in 755 consecutive patients. Langenbecks Arch Surg 2011;396:91-98.
5 Kim WS, Choi DW, Choi SH, Heo JS, Kim MJ, Song SC, et al. Clinical validation of the ISGPF classification and the risk factors of pancreatic fistula formation following duct-tomucosa pancreaticojejunostomy by one surgeon at a single center. J Gastrointest Surg 2011;15:2187-2192.
6 Uemura K, Murakami Y, Sudo T, Hashimoto Y, Nakashima A, Yamaoka E, et al. Elevation of urine trypsinogen 2 is an independent risk factor for pancreatic fistula after pancreaticoduodenectomy. Pancreas 2012;41:876-881.
7 Tranchart H, Gaujoux S, Rebours V, Vullierme MP, Dokmak S, Levy P, et al. Preoperative CT scan helps to predict the occurrence of severe pancreatic fistula after pancreaticoduodenectomy. Ann Surg 2012;256:139-145.
8 Sheehan MK, Beck K, Creech S, Pickleman J, Aranha GV. Distal pancreatectomy: does the method of closure influence fistula formation? Am Surg 2002;68:264-268.
9 Bilimoria MM, Cormier JN, Mun Y, Lee JE, Evans DB, Pisters PW. Pancreatic leak after left pancreatectomy is reduced following main pancreatic duct ligation. Br J Surg 2003;90:190-196.
10 Balzano G, Zerbi A, Cristallo M, Di Carlo V. The unsolved problem of fistula after left pancreatectomy: the benefit of cautious drain management. J Gastrointest Surg 2005;9:837-842.
11 Pannegeon V, Pessaux P, Sauvanet A, Vullierme MP, Kianmanesh R, Belghiti J. Pancreatic fistula after distal pancreatectomy: predictive risk factors and value of conservative treatment. Arch Surg 2006;141:1071-1076.
12 Kleeff J, Diener MK, Z'graggen K, Hinz U, Wagner M, Bachmann J, et al. Distal pancreatectomy: risk factors for surgical failure in 302 consecutive cases. Ann Surg 2007;245: 573-582.
13 Sierzega M, Niekowal B, Kulig J, Popiela T. Nutritional status affects the rate of pancreatic fistula after distal pancreatectomy: a multivariate analysis of 132 patients. J Am Coll Surg 2007;205:52-59.
14 Ferrone CR, Warshaw AL, Rattner DW, Berger D, Zheng H, Rawal B, et al. Pancreatic fistula rates after 462 distal pancreatectomies: staplers do not decrease fistula rates. J Gastrointest Surg 2008;12:1691-1698.
15 Goh BK, Tan YM, Chung YF, Cheow PC, Ong HS, Chan WH, et al. Critical appraisal of 232 consecutive distal pancreatectomies with emphasis on risk factors, outcome, and management of the postoperative pancreatic fistula: a 21-year experience at a single institution. Arch Surg 2008;143: 956-965.
16 Bassi C, Dervenis C, Butturini G, Fingerhut A, Yeo C, Izbicki J, et al. Postoperative pancreatic fistula: an international study group (ISGPF) definition. Surgery 2005;138:8-13.
17 Rotman N, Sastre B, Fagniez PL. Medial pancreatectomy for tumors of the neck of the pancreas. Surgery 1993;113:532-535.
18 Ikeda S, Matsumoto S, Maeshiro K, Miyazaki R, Okamoto K, Yasunami Y. Segmental pancreatectomy for the diagnosis and treatment of small lesions in the neck or body of the pancreas. Hepatogastroenterology 1995;42:730-733.
19 Iacono C, Bortolasi L, Serio G. Is there a place for central pancreatectomy in pancreatic surgery? J Gastrointest Surg 1998;2:509-517.
20 Warshaw AL, Rattner DW, Fernández-del Castillo C, Z'graggen K. Middle segment pancreatectomy: a novel technique for conserving pancreatic tissue. Arch Surg 1998;133:327-331.
21 Sperti C, Pasquali C, Ferronato A, Pedrazzoli S. Median pancreatectomy for tumors of the neck and body of the pancreas. J Am Coll Surg 2000;190:711-716.
22 Celis J, Berrospi F, Ruiz E, Payet E, Luque C. Central pancreatectomy for tumors of the neck and body of the pancreas. J Surg Oncol 2001;77:132-135.
23 Sauvanet A, Partensky C, Sastre B, Gigot JF, Fagniez PL, Tuech JJ, et al. Medial pancreatectomy: a multi-institutional retrospective study of 53 patients by the French Pancreas Club. Surgery 2002;132:836-843.
24 Balzano G, Zerbi A, Veronesi P, Cristallo M, Di Carlo V. Surgical treatment of benign and borderline neoplasms of the pancreatic body. Dig Surg 2003;20:506-510.
25 Efron DT, Lillemoe KD, Cameron JL, Yeo CJ. Central pancreatectomy with pancreaticogastrostomy for benign pancreatic pathology. J Gastrointest Surg 2004;8:532-538.
26 Shibata S, Sato T, Andoh H, Yasui O, Yoshioka M, Kurokawa T, et al. Outcomes and indications of segmental pancreatectomy. Comparison with distal pancreatectomy. Dig Surg 2004;21: 48-53.
27 Su CH, Shyr YM, Lui WY, P'eng FK. Surgical treatment for serous cystadenoma of pancreas--segmental pancreatectomy or conventional resection? Hepatogastroenterology 2004;51: 595-598.
28 Sugiyama M, Abe N, Ueki H, Masaki T, Mori T, Atomi Y. Pancreaticogastrostomy for reconstruction after medial pancreatectomy. J Am Coll Surg 2004;199:163-165.
29 Pratt W, Maithel SK, Vanounou T, Callery MP, Vollmer CM Jr. Postoperative pancreatic fistulas are not equivalent after proximal, distal, and central pancreatectomy. J Gastrointest Surg 2006;10:1264-1279.
30 Brown KM, Shoup M, Abodeely A, Hodul P, Brems JJ, Aranha GV. Central pancreatectomy for benign pancreatic lesions. HPB (Oxford) 2006;8:142-147.
31 Christein JD, Smoot RL, Farnell MB. Central pancreatectomy: a technique for the resection of pancreatic neck lesions. Arch Surg 2006;141:293-299.
32 Johnson MA, Rajendran S, Balachandar TG, Kannan DG, Jeswanth S, Ravichandran P, et al. Central pancreatectomy for benign pancreatic pathology/trauma: is it a reasonable pancreas-preserving conservative surgical strategy alternative to standard major pancreatic resection? ANZ J Surg 2006;76:987-995.
33 Müller MW, Friess H, Kleeff J, Hinz U, Wente MN, Paramythiotis D, et al. Middle segmental pancreaticresection: An option to treat benign pancreatic body lesions. Ann Surg 2006;244:909-920.
34 Roggin KK, Rudloff U, Blumgart LH, Brennan MF. Central pancreatectomy revisited. J Gastrointest Surg 2006;10:804-812.
35 Crippa S, Bassi C, Warshaw AL, Falconi M, Partelli S, Thayer SP, et al. Middle pancreatectomy: indications, short- and long-term operative outcomes. Ann Surg 2007;246:69-76.
36 Sa Cunha A, Rault A, Beau C, Collet D, Masson B. Laparoscopic central pancreatectomy: single institution experience of 6 patients. Surgery 2007;142:405-409.
37 Adham M, Giunippero A, Hervieu V, Courbière M, Partensky C. Central pancreatectomy: single-center experience of 50 cases. Arch Surg 2008;143:175-181.
38 Lavu H, Knuth JL, Baker MS, Shen C, Zyromski NJ, Schmidt M, et al. Middle segment pancreatectomy can be safely incorporated into a pancreatic surgeon's clinical practice. HPB (Oxford) 2008;10:491-497.
39 Ocuin LM, Sarmiento JM, Staley CA, Galloway JR, Johnson CD, Wood WC, et al. Comparison of central and extended left pancreatectomy for lesions of the pancreatic neck. Ann Surg Oncol 2008;15:2096-2103.
40 Shimada K, Sakamoto Y, Esaki M, Kosuge T, Hiraoka N. Role of medial pancreatectomy in the management of intraductal papillary mucinous neoplasms and islet cell tumors of the pancreatic neck and body. Dig Surg 2008;25:46-51.
41 Hirono S, Tani M, Kawai M, Ina S, Nishioka R, Miyazawa M, et al. A central pancreatectomy for benign or low-grade malignant neoplasms. J Gastrointest Surg 2009;13:1659-1665.
42 Huang H, Dong X, Gao SL, Wu YL. Conservative resection for benign tumors of the proximal pancreas. World J Gastroenterol 2009;15:4044-4048.
43 Wayne M, Neragi-Miandoab S, Kasmin F, Brown W, Pahuja A, Cooperman AM. Central pancreatectomy without anastomosis. World J Surg Oncol 2009;7:67.
44 Zhou J, Dong M, Kong F, Li Y, Tian Y. Central pancreatectomy for benign tumors of the neck and body of the pancreas: report of eight cases. J Surg Oncol 2009;100:273-276.
45 Cataldegirmen G, Schneider CG, Bogoevski D, Koenig A, KaifiJT, Bockhorn M, et al. Extended central pancreatic resection as an alternative for extended left or extended right resection for appropriate pancreatic neoplasms. Surgery 2010;147:331-338.
46 DiNorcia J, Ahmed L, Lee MK, Reavey PL, Yakaitis EA, Lee JA, et al. Better preservation of endocrine function after central versus distal pancreatectomy for mid-gland lesions. Surgery 2010;148:1247-1256.
47 LaFemina J, VagefiPA, Warshaw AL, Fernández-del Castillo C. Transgastric pancreaticogastric anastomosis: an alternative operative approach for middle pancreatectomy. Arch Surg 2010;145:476-481.
48 Shikano T, Nakao A, Kodera Y, Yamada S, Fujii T, Sugimoto H, et al. Middle pancreatectomy: safety and long-term results. Surgery 2010;147:21-29.
49 Sudo T, Murakami Y, Uemura K, Hayashidani Y, Hashimoto Y, Ohge H, et al. Middle pancreatectomy with pancreaticogastrostomy: a technique, operative outcomes, and long-term pancreatic function. J Surg Oncol 2010;101:61-65.
50 Kang CM, Lee JM, Kim MW, Yoon DS, Park JS, Lee WJ. Experiences in central pancreatectomy. Dig Surg 2011;28:57-62.
51 Jabłońska B, Żaworonkow D, Dranka-Bojarowska D, Musialski P, Lampe P. Middle pancreatectomy--own experience. Pol Przegl Chir 2011;83:237-243.
52 Boggi U, Amorese G, De Lio N, Perrone V, D'Imporzano S, Croce C, et al. Central pancreatectomy with inframesocolic pancreatojejunostomy. Langenbecks Arch Surg 2012;397:1013-1021.
53 Dumitrascu T, Barbu ST, Purnichescu-Purtan R, Ionescu M, Popescu I. Risk factors for surgical complications after central pancreatectomy. Hepatogastroenterology 2012;59:592-598.
54 Venara A, de Franco V, Mucci S, Frampas E, Lermite E, Regenet N, et al. Central pancreatectomy: comparison of results according to the type of anastomosis. J Visc Surg 2012;149:e153-158.
55 Xiang GM, Tan CL, Zhang H, Ran X, Mai G, Liu XB. Central pancreatectomy for benign or borderline lesions of the pancreatic neck: a single centre experience and literature review. Hepatogastroenterology 2012;59:1286-1289.
56 Pessaux P, Sauvanet A, Mariette C, Paye F, Muscari F, Cunha AS, et al. External pancreatic duct stent decreases pancreatic fistula rate after pancreaticoduodenectomy: prospective multicenter randomized trial. Ann Surg 2011;253:879-885.
57 Denbo JW, Orr WS, Zarzaur BL, Behrman SW. Toward defining grade C pancreatic fistula following pancreaticoduodenectomy: incidence, risk factors, management and outcome. HPB (Oxford) 2012;14:589-593.
58 Zhou Y, Yang C, Wang S, Chen J, Li B. Does external pancreatic duct stent decrease pancreatic fistula rate after pancreatic resection?: a meta-analysis. Pancreatology 2011;11: 362-370.
Received November 26, 2012
Accepted after revision August 15, 2013
Author Affiliations: Department of Hepatobiliary & Pancreatovascular Surgery, First Affiliated Hospital of Xiamen University; Oncologic Center of Xiamen, Xiamen 361003, China (Zhou YM, Wu LP, Su X and Li B); The 4th Department of Hepatic Surgery, Eastern Hepatobiliary Surgery Hospital, Second Military Medical University, Shanghai 200438, China (Zhang XF and Shi LH)
Bin Li, MS, Department of Hepatobiliary & Pancreatovascular Surgery, First Affiliated Hospital of Xiamen University, Xiamen 361003, China (Tel: 86-592-2139708; Fax: 86-592-2139908; Email: Binl1962@sina.cn)
© 2014, Hepatobiliary Pancreat Dis Int. All rights reserved.
10.1016/S1499-3872(14)60032-1
杂志排行
Hepatobiliary & Pancreatic Diseases International的其它文章
- Multi-visceral resection of locally advanced extra-pancreatic carcinoma
- Effects of plasma exchange combined with continuous renal replacement therapy on acute fatty liver of pregnancy
- FBW7 increases chemosensitivity in hepatocellular carcinoma cells through suppression of epithelialmesenchymal transition
- Pancreatic head cancer in patients with chronic pancreatitis
- Instrumental detection of cystic duct stones during laparoscopic cholecystectomy
- Improved anterior hepatic transection for isolated hepatocellular carcinoma in the caudate
