Effects of plasma exchange combined with continuous renal replacement therapy on acute fatty liver of pregnancy
2014-05-04ChengBoYuJiaJiaChenWeiBoDuPingChenJianRongHuangYueMeiChenHongCuiCaoandLanJuanLi
Cheng-Bo Yu, Jia-Jia Chen, Wei-Bo Du, Ping Chen, Jian-Rong Huang, Yue-Mei Chen, Hong-Cui Cao and Lan-Juan Li
Hangzhou, China
Effects of plasma exchange combined with continuous renal replacement therapy on acute fatty liver of pregnancy
Cheng-Bo Yu, Jia-Jia Chen, Wei-Bo Du, Ping Chen, Jian-Rong Huang, Yue-Mei Chen, Hong-Cui Cao and Lan-Juan Li
Hangzhou, China
BACKGROUND:Acute fatty liver of pregnancy (AFLP) in the third trimester or early postpartum period can lead to fatal liver damage. Its traditional therapy is not very effective in facilitating hepatic recovery. The safety and effect of plasma exchange (PE) in combination with continuous renal replacement therapy (CRRT) (PE+CRRT) for AFLP still needs evaluation.
METHODS:Five AFLP patients with hepatic encephalopathy and renal failure were subjected to PE+CRRT in our department from 2007 to 2012. Their symptoms, physical signs and results were observed, and all relevant laboratory tests were compared before and after PE+CRRT.
RESULTS:All the 5 patients were well tolerated to the therapy. Four of them responded to the treatment and showed improvement in clinical symptoms/signs and laboratory results, and they were cured and discharged home after the treatment. One patient succeeded in bridging to transplantation for slowing down hepatic failure and its complications process after 2 treatment sessions. Intensive care unit stay and hospital stay were 9.4 (range 5-18) and 25.0 days (range 11-42), respectively.CONCLUSION:PE+CRRT is safe and effective and should be used immediately at the onset of hepatic encephalopathy and/or renal failure in patients with AFLP.
(Hepatobiliary Pancreat Dis Int 2014;13:179-183)
plasma exchange; continuous renal replacement therapy;
acute fatty liver;
pregnancy;
liver failure
Introduction
Acute fatty liver of pregnancy (AFLP) is an uncommon but potentially lethal and elusive complication that occurs in the third trimester or early postpartum period. Multiple organ dysfunction syndrome (MODS) and associated death is common in such cases. Mother-infant mortality rate is as high as 18%-25%. However, the cause of AFLP is not fully clear at present. Researchers[1,2]suggested that AFLP may be related to increased estrogen, metabolism disturbance of fatty acid (i.e., long-chain 3-hydroxyacyl coenzyme A dehydrogenase) or mitochondrial dysfunction in the third trimester or early postpartum period.
Once insulted, microvesicular fatty infiltration results in encephalopathy and hepatic failure. Other clinical manifestations include disseminated intravascular coagulation (DIC), coagulation disturbance, metabolic disorders, and the accumulation of toxic substances (e.g., endotoxins and fatty acids). Treatments should focus on the removal of toxicants and the maintenance of internal homeostasis. Several therapies such as rapid termination of pregnancy and early comprehensive treatment are thought to effectively improve the prognosis of AFLP.[3,4]In addition, liver transplantation is required in some cases. Nevertheless, traditional managements are not sufficiently effective for hepatic recovery.[5]
Meanwhile, artificial liver has been used for AFLP patients on several occasions.[6-8]Plasma exchange in combination with continuous renal replacementtherapy (PE+CRRT) is a novel treatment for AFLP patients. Presently, PE+CRRT technologies still lack systematic evaluation. Although few studies reported the effectiveness and safety of PE+CRRT, they have not been widely accepted in clinical practice. PE+CRRT in the treatment of AFLP[9]demonstrated that it is capable of eliminating many toxins and replenishing nutrients, thus shortening the recovery time. The introduction of PE+CRRT in our center maximized the treatment effectiveness over the last 5 years. Thus, the present study aimed to determine the effect of PE+CRRT in the treatment of AFLP patients including those with serious complications.
Methods
Patients
This study was approved by the Ethics Committee of our hospital. Five patients who had been diagnosed with AFLP and managed with PE+CRRT in our artificial liver treatment center between 2007 and 2012 were reviewed. The diagnosis of AFLP was confirmed according to the Swansea criteria after viral hepatitis and hemolysis, elevated liver enzymes and low platelet (HELLP) syndrome were excluded.[10]None of these patients was reported previously. The five patients were admitted to the medical intensive care unit (ICU) for overall management and received PE+CRRT until they were at the recovery phase.
PE+CRRT procedures
PE+CRRT was given to the five patients who had been evaluated before PE+CRRT. PE+CRRT was initiated within 24-72 hours after the termination of pregnancy. At first, a double-lumen catheter was inserted into the femoral vein of the patient. During the treatment, blood flow was maintained at 80-120 mL per minute and the plasma separation rate was set at 20 mL/min.[11]The total volume of PE was calculated as described previously.[12]According to the conditions of the patient, PE+CRRT was performed for 1-3 times. AFLP patients with hepatic encephalopathy or hepatorenal syndrome were treated with a combination of PE and continuous venovenous hemofiltration (CVVHF), venovenous hemodiafiltration (CVVHDF), or venovenous hemoperfusion (CVVHP) once a day or every other day. Combined treatment can regulate electrolyte imbalance and improve renal function and hepatic encephalopathy.[9,13,14]
Blood samples (10-20 mL) were taken to assess blood biochemical parameters and liver function reserve. The exchanged fluid was collected at the beginning and the end of each PE+CRRT session to calculate the clearance rate.
Statistical analysis
Data were analyzed using SPSS 17.0 (SPSS Inc., Chicago, IL, USA) and expressed as mean±standard deviation (SD). Median values were compared using the Mann-WhitneyUtest. Abnormal cases were also expressed proportionately. The rates in the study were compared by the Chi-square test. APvalue <0.05 was considered statistically significant.
Results
Demographic characteristics
The five AFLP patients complicated with MODS received PE+CRRT (Table 1). Their mean age was 29 ±6 years (range 23-36). Of the five patients, 2 were primiparous and 3 multiparous. The mean fetal age on admission was 35 weeks (range 29-39). Three women were diagnosed with AFLP before the delivery, 1 on the day after delivery, and 1 on the second day after delivery. Cesarean delivery was performed in 4 patients, and vaginal delivery in 1. All of the 5 patients were given antenatal care at the nearest hospital before referral and none received preferential treatment. The liver function of the patients was normal until the onset of AFLP. There was no stillbirth.
PE+CRRT
In the 5 patients with renal insufficiency (mean serum creatinine level: 269.2±97.3 mmol/L), 2 presented with oliguria. Their total levels of bilirubin, aminotransferases and serum lactic dehydrogenase were significantly elevated. The levels of albumin and blood glucose were decreased, and the prothrombintime was prolonged. Moreover, of the patients with thrombocytopenia, 2 had obvious thrombocytopenia (platelet count <40×109/L). PE+CRRT treatment significantly improved the liver and renal function of the patients and corrected coagulopathy and blood glucose (Table 2).
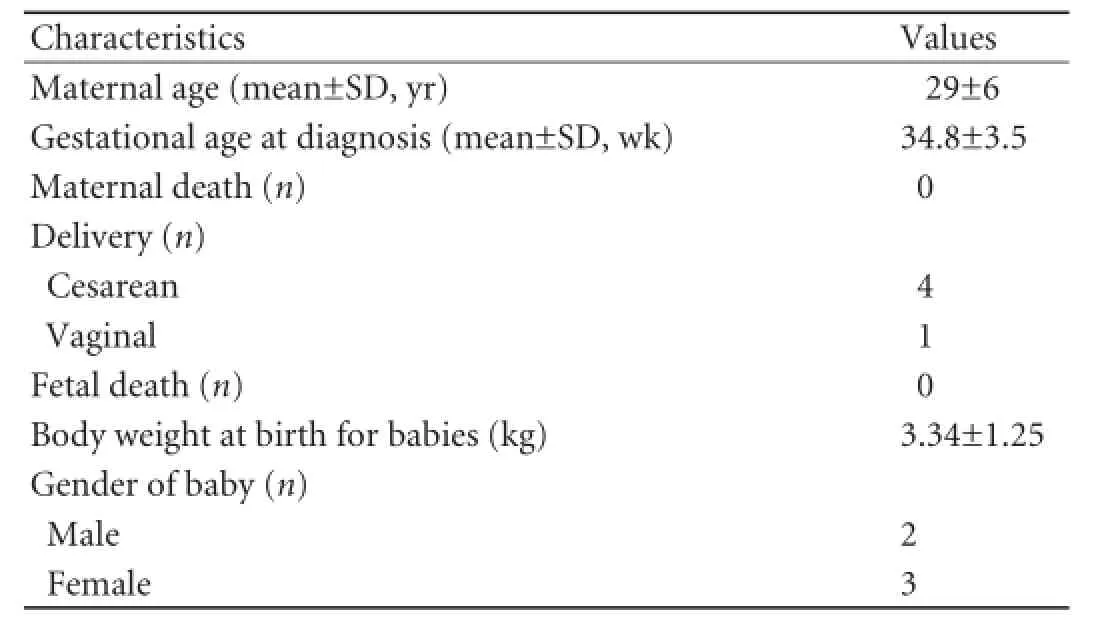
Table 1.Clinical features of patients (n=5) and babies (n=5)
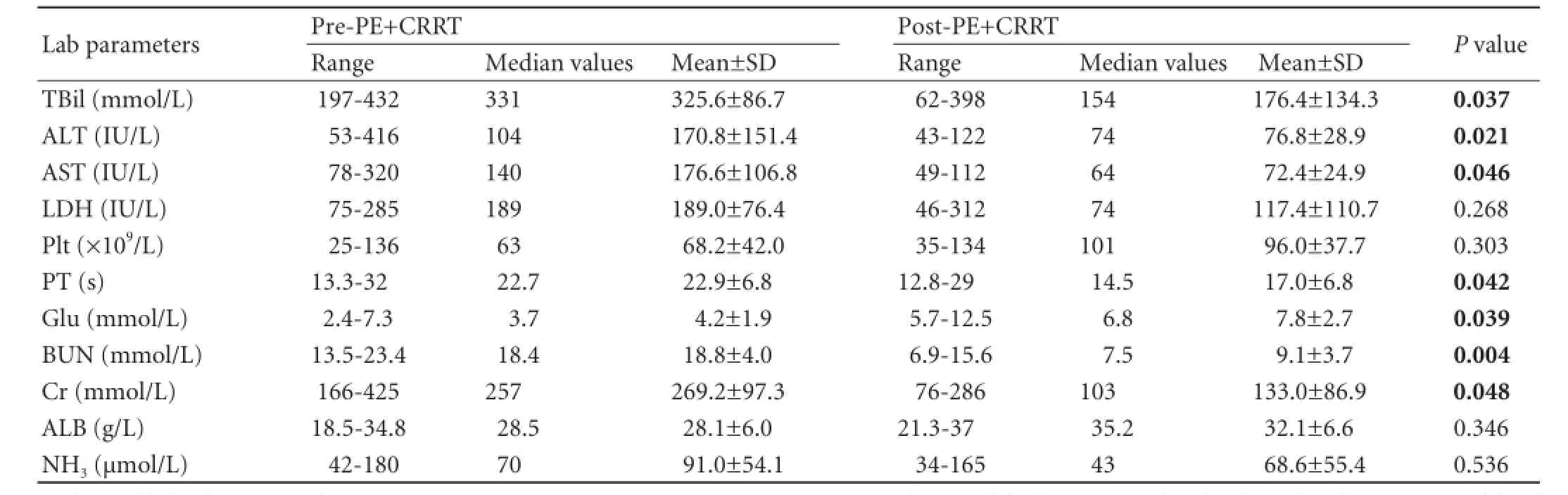
Table 2.Lab parameters of AFLP preceding first PE+CRRT and after final PE+CRRT
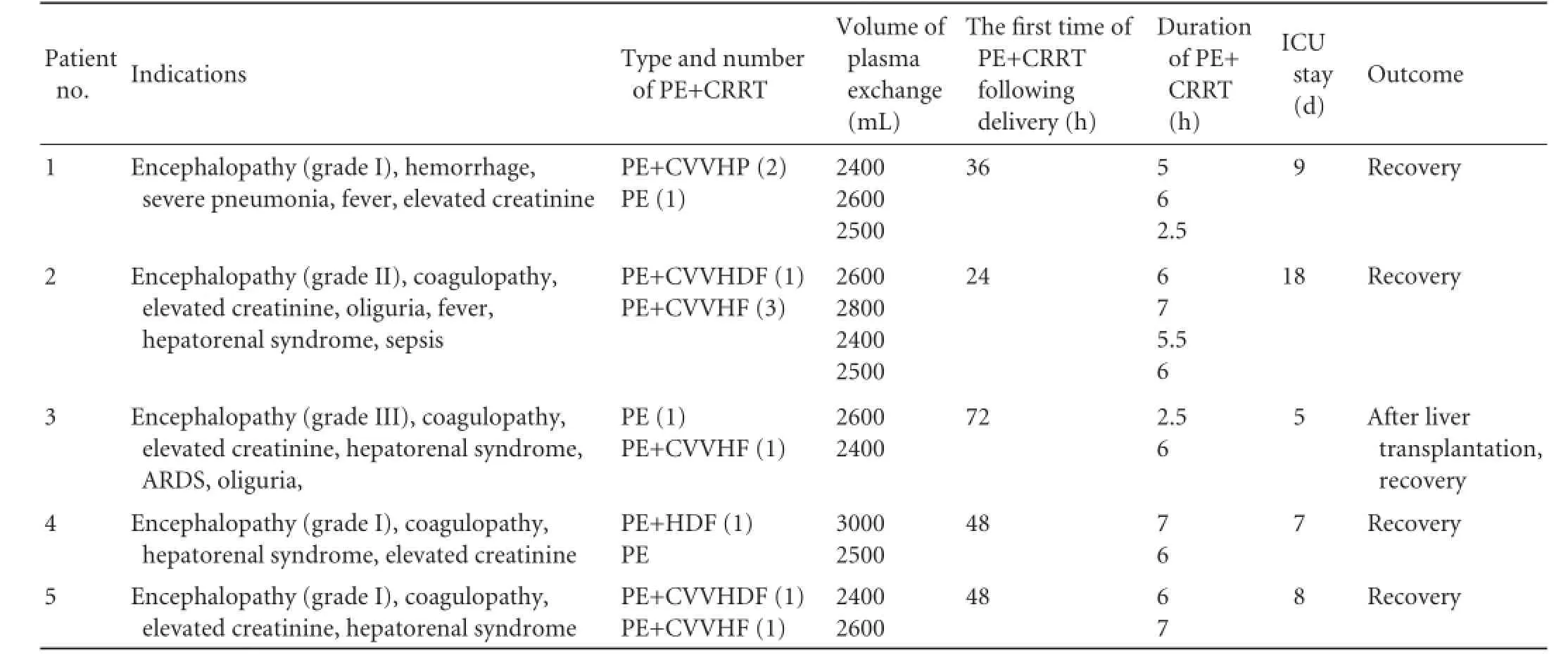
Table 3.Clinical course of the patients with AFLP complicated with multiple organ dysfunction
Patient outcomes
At the time of deterioration in the first 24-108 hours postpartum, the 5 patients were referred to our hospital for urgent treatment. In these patients, AFLP was complicated by significant renal insufficiency with increased serum ammonia. They had mental disorder or encephalopathy, and only one required mechanical ventilation because of adult respiratory distress syndrome. A total of 13 PE+CRRT sessions were given to the 5 patients. PE combined with CVVHP, CVVHDF, or CVVHF was performed 2 days postpartum on average (range 1-3). PE+CRRT was well tolerated in 5 patients. ICU stay was 9.4 days (range 5-18) and hospital stay 25.0 days (range 11-42). In this series, 4 patients were cured and discharged home, whereas the remaining one was sent to the liver transplantation unit of our hospital and was cured. The data of the 5 AFLP patients are shown in Table 3.
Discussion
AFLP is a rare but severe maternal illness that occurs inthe third trimester or early postpartum period. Early diagnosis, rapid termination of pregnancy, and advances in critical care medicine have improved the prognosis of this disease. However, no clinical trials have ever compared the efficacy of therapeutic methods for AFLP. Therefore, no data are available for demonstrating the feasibility of PE+CRRT. Clinical data on AFLP were largely based on a few cases treated with conventional supportive medicine.[6,15]Clinical and fundamental investigations of PE+CRRT on non-pregnant women with acute hepatic failure reported satisfactory results.[16-19]Nevertheless, PE+CRRT for AFLP is a novel treatment option. The cases in the present study were among the first to be published, introducing PE+CRRT as an important method and even as a rescue measure for the treatment of AFLP. Of the 5 patients treated with PE+CRRT including PE and CVVHDF, CVVHF, or CVVHP, 4 survived, and one was transferred to the liver transplantation unit after 2 PE+CRRT sessions and cured ultimately.
Early PE+CRRT may effectively remove a vast quantity of endotoxins, supply blood coagulation factors and albumin, and ameliorate coagulopathy. More importantly, PE+CRRT can maintain hemodynamic stability as well as water-electrolyte and acid-base balance, which may be conducive to MODS.[20]Furthermore, PE+CRRT may be effective for the management of fluids and rapid correction of metabolic disorders. In the present study, the total bilirubin levels of the patients decreased significantly, the prothrombin time decreased, and the levels of blood glucose were significantly increased after PE+CRRT treatment.
All patients suffered from preexisting acute kidney injury. Their levels of serum creatinine were significantly decreased after PE+CRRT. Therefore, early PE+CRRT can promote hepatic and renal rehabilitation and prevent severe complications in AFLP patients with renal insufficiency. During the treatment, no side-effects such as leukopenia, thrombocytopenia, pulmonary edema, and allergy were observed.
One patient underwent liver transplantation at the same hospital. University hospitals such as ours can accept critical patients with AFLP from other institutions, since they can receive combined therapies including PE+CRRT.
All the 5 patients were transferred to our ICU from other hospitals after delivery. These patients, either received PE+CRRT earlier or was subjected to liver transplantation, survived. This indicates that early PE+CRRT is suitable for severe AFLP patients with potentially fatal illness that cannot be controlled by conventional therapy.
Although conventional therapy is the preferred for AFLP, PE+CRRT may benefit patients with refractory and critical diseases who do not exhibit a curative effect but a deterioration. In conclusion, we consider that PE+CRRT is effective in the treatment of patients with advanced AFLP complicated by renal failure and encephalopathy.
Contributors:LLJ proposed the study. YCB and LLJ performed research and wrote the first draft. CJJ, DWB, CP, HJR, CYM and CHC collected and analyzed the data. All authors contributed to the design and interpretation of the study and to further drafts. LLJ is the guarantor.
Funding:The work was supported by grants from the National Scientific and Technological Major Project of China (2011ZX10004-901 and 2013ZX10004904), the National Science and Technology Major Project (2012ZX10002006), the Scientific Research Fundation of the Education Department, Zhejiang Province (N20120081).
Ethical approval:This study was approved by the Ethics Committee of the First Affiliated Hospital, Zhejiang University School of Medicine.
Competing interest:No benefits in any form have been received or will be received from a commercial party related directly or indirectly to the subject of this article.
1 Wilcken B, Leung KC, Hammond J, Kamath R, Leonard JV. Pregnancy and fetal long-chain 3-hydroxyacyl coenzyme A dehydrogenase deficiency. Lancet 1993;341:407-408.
2 Treem WR, Rinaldo P, Hale DE, Stanley CA, Millington DS, Hyams JS, et al. Acute fatty liver of pregnancy and longchain 3-hydroxyacyl-coenzyme A dehydrogenase deficiency. Hepatology 1994;19:339-345.
3 Moldenhauer JS, O'brien JM, Barton JR, Sibai B. Acute fatty liver of pregnancy associated with pancreatitis: a lifethreatening complication. Am J Obstet Gynecol 2004;190:502-505.
4 Ibdah JA. Acute fatty liver of pregnancy: an update on pathogenesis and clinical implications. World J Gastroenterol 2006;12:7397-7404.
5 Rajasri AG, Srestha R, Mitchell J. Acute fatty liver of pregnancy (AFLP)--an overview. J Obstet Gynaecol 2007;27:237-240.
6 Martin JN Jr, Briery CM, Rose CH, Owens MT, Bofill JA, Files JC. Postpartum plasma exchange as adjunctive therapy for severe acute fatty liver of pregnancy. J Clin Apher 2008;23:138-143.
7 Won TJ, Lin YH, Huang LW. Successful clinical application of the molecular adsorbent recirculating system in a patient with acute fatty liver of pregnancy. Taiwan J Obstet Gynecol 2008;47:113-115.
8 Vora KS, Shah VR, Parikh GP. Acute fatty liver of pregnancy: a case report of an uncommon disease. Indian J Crit Care Med 2009;13:34-36.
9 Li LJ. Artificial liver, 2nd ed. Zhejiang: Zhejiang University Press; 2012:1-8.
10 Ch'ng CL, Morgan M, Hainsworth I, Kingham JG.Prospective study of liver dysfunction in pregnancy in Southwest Wales. Gut 2002;51:876-880.
11 Bramlage CP, Schröder K, Bramlage P, Ahrens K, Zapf A, Müller GA, et al. Predictors of complications in therapeutic plasma exchange. J Clin Apher 2009;24:225-231.
12 Li LJ, Zhang YM, Liu XL, Du WB, Huang JR, Yang Q, et al. Artificial liver support system in China: a review over the last 30 years. Ther Apher Dial 2006;10:160-167.
13 Artificial Liver Group Chinese Association of Infectious and Parasitic Diseases. Operating guide for artificial liver support system. Zhonghua Gan Zang Bing Za Zhi 2002;10:329-332.
14 Tang WX, Huang ZY, Chen ZJ, Cui TL, Zhang L, Fu P. Combined blood purification for treating acute fatty liver of pregnancy complicated by acute kidney injury: a case series. J Artif Organs 2012;15:176-184.
15 Sibai BM. Imitators of severe pre-eclampsia/eclampsia. Clin Perinatol 2004;31:835-852.
16 Yonekawa C, Nakae H, Tajimi K, Asanuma Y. Effectiveness of combining plasma exchange and continuous hemodiafiltration in patients with postoperative liver failure. Artif Organs 2005;29:324-328.
17 Ling Q, Xu X, Wei Q, Liu X, Guo H, Zhuang L, et al. Downgrading MELD improves the outcomes after liver transplantation in patients with acute-on-chronic hepatitis B liver failure. PLoS One 2012;7:e30322.
18 Chen YS, Wu ZW, He JQ, Yu J, Yang SG, Zhang YM, et al. The curative effect of ALSS on 1-month mortality in AoCLF patients after 72 to 120 hours. Int J Artif Organs 2007;30:906-914.
19 Du WB, Li LJ, Huang JR, Yang Q, Liu XL, Li J, et al. Effects of artificial liver support system on patients with acute or chronic liver failure. Transplant Proc 2005;37:4359-4364.
20 Augustine JJ, Sandy D, Seifert TH, Paganini EP. A randomized controlled trial comparing intermittent with continuous dialysis in patients with ARF. Am J Kidney Dis 2004;44:1000-1007.
Received August 5, 2013
Accepted after revision January 29, 2014
Author Affiliations: State Key Laboratory for Diagnosis and Treatment of Infectious Diseases, the First Affiliated Hospital, Zhejiang University School of Medicine (Yu CB, Chen JJ, Du WB, Chen P, Huang JR, Chen YM, Cao HC and Li LJ); Collaborative Innovation Center for Diagnosis and Treatment of Infectious Diseases (Du WB, Huang JR, Cao HC and Li LJ), Hangzhou 310003, China
Lan-Juan Li, MD, State Key Laboratory for Diagnosis and Treatment of Infectious Disease, the First Affiliated Hospital, Zhejiang University School of Medicine, 79 Qingchun Road, Hangzhou 310003, China (Tel: 86-571-87236458; Fax: 86-571-87236459; Email: ljli@ zju.edu.cn)
© 2014, Hepatobiliary Pancreat Dis Int. All rights reserved.
10.1016/S1499-3872(14)60028-X
杂志排行
Hepatobiliary & Pancreatic Diseases International的其它文章
- Pancreatic fistula after central pancreatectomy: case series and review of the literature
- FBW7 increases chemosensitivity in hepatocellular carcinoma cells through suppression of epithelialmesenchymal transition
- Pancreatic head cancer in patients with chronic pancreatitis
- Multi-visceral resection of locally advanced extra-pancreatic carcinoma
- Instrumental detection of cystic duct stones during laparoscopic cholecystectomy
- Improved anterior hepatic transection for isolated hepatocellular carcinoma in the caudate
