Angiographic embolization in the treatment of intrahepatic arterial bleeding in patients with blunt abdominal trauma
2014-05-04YaLinKongHongYiZhangXiaoJunHeGangZhaoChengLiLiuMeiXiaoandYuYingZhen
Ya-Lin Kong, Hong-Yi Zhang, Xiao-Jun He, Gang Zhao, Cheng-Li Liu, Mei Xiao and Yu-Ying Zhen
Beijing, China
Angiographic embolization in the treatment of intrahepatic arterial bleeding in patients with blunt abdominal trauma
Ya-Lin Kong, Hong-Yi Zhang, Xiao-Jun He, Gang Zhao, Cheng-Li Liu, Mei Xiao and Yu-Ying Zhen
Beijing, China
BACKGROUND:Angiographic embolization (AE) as an adjunct non-operative treatment of intrahepatic arterial bleeding has been widely used. The present study aimed to evaluate the efficacy of selective AE in patients with hepatic trauma.
METHODS:Seventy patients with intrahepatic arterial bleeding after blunt abdominal trauma who had undergone selective AE in 10 years at this institution were retrospectively reviewed. The criteria for selective AE included active extravasation on contrast-enhanced CT, an episode of hypotension or a decrease in hemoglobin level during the non-operative treatment. The data of the patients included demographics, grade of liver injuries, mechanism of blunt abdominal trauma, associated intra-abdominal injuries, indications for AE, angiographic findings, type of AE, and AE-related hepatobiliary complications.
RESULTS:In the 70 patients, 32 (45.71%) had high-grade liver injuries. Extravazation during the early arterial phase mainly involved the right hepatic segments. Thirteen (18.57%) patients underwent embolization of intrahepatic branches and the extrahepatic trunk and these patients all developed AE-related hepatobiliary complications. In 19 patients with AE-related complications, 14 received minimally invasive treatment and recovered without severe sequelae.
CONCLUSIONS:AE is an adjunct treatment for liver injuries. Selective and/or super-selective AE should be advocated to decrease the incidence and severity of AE-related hepatobiliary complications.
(Hepatobiliary Pancreat Dis Int 2014;13:173-178)
angiography;
selective embolization;
liver injury;
hepatic arterial bleeding;
complication
Introduction
Intrahepatic arterial bleeding has been considered as an indication of laparotomy for patients with blunt abdominal trauma complicated with liver injury, and accounted for 20%-35% of the patients who failed in non-operative treatment.[1]Over the past 20 years, significant changes have been made in the treatment of blunt liver injury. Non-operative treatment has become the standard therapy for hemodynamically stable patients with low-grade liver injuries (I-II).[2,3]With angiographic embolization (AE) as an adjunct non-operative treatment, patients with high-grade liver injuries (IV-V) have also been successfully treated.[4]Although the potential of AE to expand the scope of non-operative management and to increase its success rate has been recognized, the actual benefit of AE is still unclear, and controversy remains over the efficacy of AE for patients with suspected intrahepatic bleeding after blunt abdominal trauma.[5]
Over the past decade, we have performed selective AE for the patients with active intrahepatic arterial bleeding after blunt abdominal trauma and have achieved some experience in the non-operative treatment of patients with liver injury. This study was undertaken to analyze the clinical characteristics of such patients, and to systematically evaluate the efficacy of selective AE.
Methods
The patients with blunt liver injuries who had beenadmitted to our hospital from January 1, 2002 to December 31, 2011 were retrospectively studied. This study was conducted in compliance with the Declaration of Helsinki (revised in 2000) and approved by the Ethics Committee of the Chinese PLA Air Force General Hospital (Trial Registration Number: KZ2012024). Since the study was retrospective, the Ethics Committee waived the requirement for informed consent from the patients.
Inclusion criteria included: (1) patients who were hemodynamically stable on admission or stabilized by initial resuscitation; (2) patients with blunt liver injuries associated with injuries of solid organs such as the kidney, pancreas and spleen, which were within the scope of non-operative management; (3) patients with no symptoms and signs of peritonitis; (4) patients with no signs and signs of gastric or intestinal rupture; and (5) patients who underwent selective AE during the non-operative treatment because of high-risk intrahepatic arterial bleeding. Exclusion criteria included: (1) patients with abdominal trauma caused by penetrating injuries; (2) patients who were hemodynamically unstable after resuscitation in the Emergency Department and transported directly to the operating room for abdominal exploration; (3) patients with temporary stable hemodynamics who developed peritonitis and/or unstable hemodynamics during the non-operative management and were subjected to abdominal exploration in the operation room.
Selective AE was performed under digital subtractive angiography (DSA) by the right-sided femoral approach after local anesthesia. With fluoroscopic guidance, a 5-F reverse curve Mickelson (Cook, Bloomington, IN, USA) catheter was introduced, and the celiac and hepatic arteries were selectively catheterized. After identification of the extravasation of the contrast medium from the hepatic arterial branches, selective embolization was performed using the microcatheter system to deploy multiple Tornado coils (Cook) of various sizes into the segmental or main branches of the hepatic artery. Follow-up imaging confirmed the position of the coils. Specific procedure was performed for each patient at the discretion of the attending interventional radiologist. Follow-up imaging was not routinely performed unless new symptoms or signs appeared. Successful selective AE was defined if there was no active bleeding shown angiographically after embolization.
Demographics, grading of liver injury, mechanism of blunt abdominal trauma, associated intra-abdominal injury, indications for AE, angiographic findings, type of AE, and AE-related hepatobiliary complications of the patients were all reviewed. Liver injuries were graded according to Trauma Classification (revised in 1994) of the American Association for Surgery.[6]AE-related hepatobiliary complications included liver abscess, hepatic necrosis, gallbladder infarction, bile peritonitis, bile leak, and biloma formation.[7]
Results
Seventy patients with blunt liver injury underwent selective AE because of active bleeding of the intrahepatic artery. These patients comprised 52 men and 18 women, with a mean age of 36.3 years (range: 16-62). Trauma mechanism included motor vehicle collision in 32 (45.71%) patients, motorcycle crash in 11 (15.71%), pedestrian vs auto in 4 (5.71%), falling injury in 15 (21.43%), sports injury in 2 (2.86%), and explosive blast injury in 6 (8.57%). According to Trauma Classification of the American Association for Surgery, 13 patients (18.57%) had liver injuries of grade II, 25 (35.71%) grade III, 23 (32.86%) grade IV, and 9 (12.86%) grade V (Table 1).
Associated injuries of intra-abdominal organs werefound in 16 (22.86%) patients, including 10 splenic injuries, 3 renal injuries, and 3 pancreatic injuries. Indications for AE included active extravasation on contrast-enhanced CT in 27 (38.57%) patients, an episode of hypotension or decreased hemoglobin (Hb) level during the non-operative treatment in 29 (41.43%), high-grade liver injury demonstrated by CT in 5 (7.14%), and required angiogram for other injuries (injury of the spleen or aorta) in 9 (12.86%). Angiography revealed multiple extravasations during the early arterial phase involving segment I in 2 (2.17%) patients, segment II in 7 (7.61%), segment III in 10 (10.87%), segment IV in 11 (11.96%), segment V in 12 (13.04%), segment VI in 14 (15.22%), segment VII in 17 (18.48%), and segment VIII in 19 (20.65%). But no patient had active extravasation from the hepatic trunk in the early arterial phase. The late arterial phase depicted active extravasation from the proximal left hepatic artery in 4 patients, and from the proximal right hepatic artery in 9 patients. Neither bleeding from the juxtahepatic veins nor supplementary contrast pooling was found during the portal phase. Simple selective embolization involving the arterial branches was done in 57 (81.43%) patients using a coaxial microcatheter, and 31 of them underwent superselective embolization (embolization of the terminalbranches of the bleeding intrahepatic artery). Combined embolization involving the intrahepatic branches and extrahepatic trunk was performed in 13 (18.57%) patients using metal and coaxial microcoils. Nineteen patients (27.14%) developed AE-related hepatobiliary complications after embolization, including liver abscess (9 patients), hepatic necrosis (11), gallbladder infarction (5), bile peritonitis (2), bile leak (3), and biloma formation (3). CT and selective AE images of patients with blunt liver injuries are shown in Figs. 1-3. AE-related hepatobiliary complications occurred in 6 patients after selective embolization (including 2 patients after super-selective embolization) and in 13 patients after intrahepatic and extrahepatic embolization. Laparoscopic cholecystectomy was performed in 5 patients with gallbladder infarction. Percutaneous aspiration and catheter drainage guided by ultrasound were performed in 7 patients with liver abscess and/or biloma formation. Laparoscopic peritoneal lavage and drainage was performed in 3 patients with bile leak and bile peritonitis. Eight patients were treated conservatively. The 16 patients with AE-related hepatobiliary complications recovered uneventfully. The clinical results of the 70 patients are shown in Table 2.
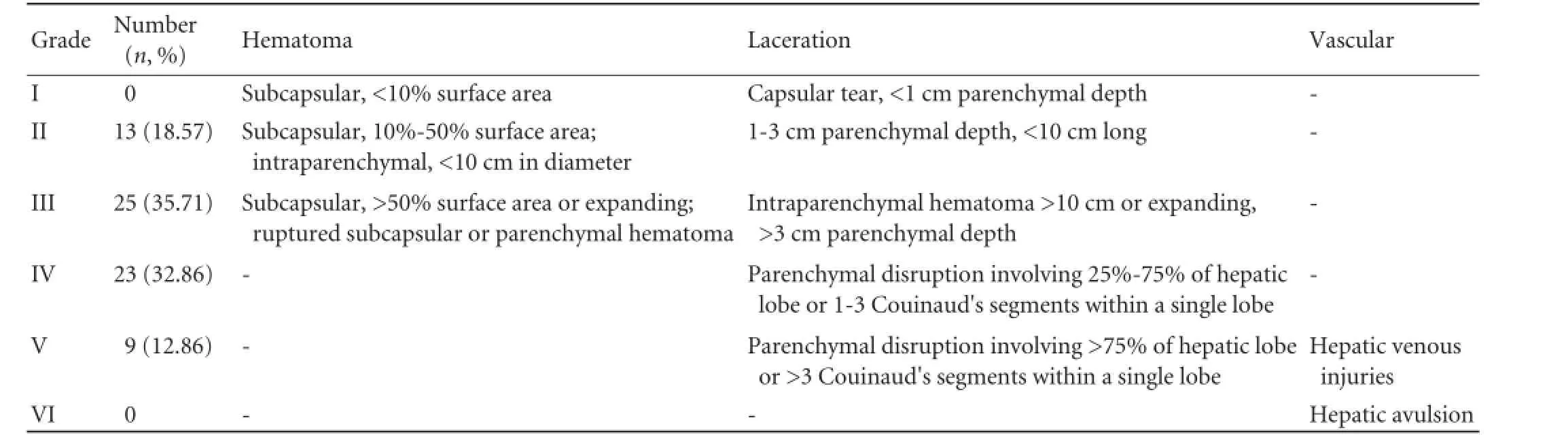
Table 1. Liver injuries and severity of the 70 patients

Fig. 1.A 33-year-old female with liver injury of grade III after a motor vehicle collision.A: CT scan showing intraperitoneal exudation around liver (arrow).B: Coronal CT showing hepatic laceration (white arrow) and intraparenchymal hematoma in segment IV and V (black arrows).C: Hepatic angiography before arterial embolizaiton: active intrahepatic arterial bleeding from parenchymal laceration (black arrow) and segment IV (white arrow) in late arterial phase under DSA.D: Hepatic angiography after selective and super-selective embolization and effective control of the intrahepatic arterial bleeding.
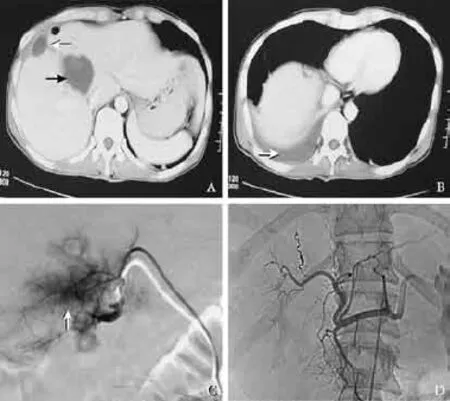
Fig. 2.A 25-year-old male with liver injury of grade IV after a falling accident.A: Enhanced CT scan, arterial phase: subcapsular hematoma (white arrow) and active bleeding (black arrow) within right hepatic lobe;B: Enhanced CT scan, delayed phase: active extravasation around right liver lobe;C: Hepatic angiography before arterial embolizaiton: active intrahepatic arterial bleeding in segment V and VIII (white arrow) in late arterial phase under DSA;D: Hepatic angiography after selective coil embolization: disappearance of contrast extravastion.
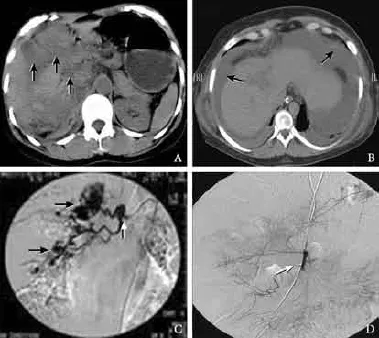
Fig. 3.A 23-year-old male with liver injury of grade V after a military training accident.A: CT scan of 2 hours after injury: multiple parenchymal lacerations (arrows);B: CT scan of 15 hours after injury: active exudation in large amount around the liver (arrows);C: Hepatic angiography before arterial embolizaiton: active intrahepatic arterial bleeding from the lacerations of segment V and VI (black arrows) and the right hepatic artery (white arrow) in late arterial phase under DSA;D: Hepatic angiography after combined embolization: combined occlusion of the right hepatic artery (white arrow) and disappearance of contrast extravastion.

Table 2.Clinical results of the 70 patients
Discussion
Non-operative management of blunt liver injury as the standard of care whenever possible reflects the enormous progress in the field of abdominal trauma. AE helps to diagnose and treat hepatic arterial bleeding in early stage, and is responsible for the significant improvements in patient outcome after non-operative management. In this study, we used AE in three situations. First, when there is no proof of active and massive bleeding. For patients whose blood pressure is unstable after vigorous fluid resuscitation, laparotomy should be performed without hesitation, and as an adjunct to non-operative treatment, AE can only stop arterial bleeding who are hemodynamically stable.[8-10]Second, when there is no severe associated solid organ injury and no gastric or intestinal rupture. In fact, the decision-making of non-operative therapy for blunt liver injury should be dependent on the overall evaluation for all associated injuries rather than on liver injury only. Third, when there is an evidence of inadequate hemostasis. Arterial contrast extravasation on CT, liver injury above grade IV, and fluctuation of hemodynamic parameters during non-operative treatment should all be considered as indications for AE because of the high risk of intrahepatic arterial bleeding.[11]
In this study, 32 (45.71%) patients undertook AE because of indications confirmed by CT. From our experience, successful non-operative treatment depends on early and timely imaging examination in order to perform AE to control arterial bleeding, and we suggest CT as the first choice if condition permits. Initially, we used sonography and conventional dual-phase CT for hemodynamically stable patients in our department to evaluate liver injury and rule out associated intraabdominal injuries. However, the limitations in image quality of conventional dual-phase CT made it often difficult to grade the liver injury, although the grading is extremely valuable for identifying associated injuries that might require immediate operation. We noticed that in this study, 9 (12.86%) patients were subjected to AE because of spleen or aorta injuries, whereas initial conventional dual-phase CT revealed no obvious signs of intrahepatic arterial bleeding. In the recent 5 years, Dual-source CT (DSCT) enhanced with intravenous contrast has become a new method for hemodynamically stable patients with suspected liver injuries in ourdepartment. DSCT is superior in detecting small quantities of blood, and allows for rapid and accurate grading of hepatic injuries in predicting the need of subsequent interventions.[12]In the 27 patients who were subjected to AE for active extravasation and the 5 patients who underwent AE for high-grade liver injury, 18 (66.67%, 18/27) and 3 (60.00%, 3/5) were detected by DSCT respectively. Thus DSCT plays a significant role in detecting patients who are only temporarily stable and require AE to control intrahepatic arterial bleeding during the non-operative treatment.
Consensus on operative exploration is conclusive for hemodynamically unstable patients with suspected high-grade liver injury, but for hemodynamically stable patients with high-grade liver injury, there is still controversy over the efficacy of non-operative treatment.[13]From our experience, hepatic arterial bleeding in the deep liver parenchyma is difficult to control even by operative packing, and postoperative or preoperative angiography/embolization may be useful for patients with deep liver parenchyma injury. Letoublon et al found that 52% of patients with IV and V liver injuries who had undergone staged laparotomy showed postoperative intrahepatic bleeding on angiography and required embolization. He suggested that AE should be performed for patients with active extravasation regardless of the grading of liver injury.[14]In our series, AE and non-operative treatment were effective in 32 patients with high-grade liver injuries (IV-V). Fourteen patients showed intrahepatic arterial bleeding in segment VI and 17 in segment VII. The bleeding in these patients was hard to control by operation because of its deep location. We suggest that for patients with high-grade liver injuries, if their general condition allows, AE should be considered as an important therapeutic method. Non-operative treatment is now commonly used for patients with low-grade liver injuries; however, intrahepatic arterial bleeding is not rare, and in such patients, AE can avoid the potential risk of surgical intervention.[15]In our series, over 50% of the patients (38/70) who received AE to control intrahepatic arterial bleeding had only grade II or III liver injuries. Another factor that needs special attention is the mechanism of trauma. Direct impact on the body surface where the liver locates caused by vehicle collision or falling to obstacles on ground, accounts for most cases of intrahepatic arterial bleeding with low-grade liver injuries, and this often causes failure of non-operative treatment.[16]In our series, 47 patients (67.14%) received AE because of the mechanisms of trauma mentioned above. We suggest that the risk of intrahepatic bleeding should be ruled out for patients even with low-grade liver injuries.
Nineteen patients (27.14%) in this study had various AE-related hepatobiliary complications mostly caused by combined embolization involving the intrahepatic branches and the extrahepatic trunk (13/19, 68.42%). The hepatobiliary complications should be considered as the clinical evolution of AE, and with the wide use of AE, there will be an increase in the incidence of such complications.[17]Although it is unavoidable, the incidence and severity of hepatobiliary complications can be lowered by selective AE. No laparotomy or lobectomy was performed in these patients because of hepatic necrosis, especially in those with grade IV and V liver injuries. The incidence of gallbladder infarction could be reduced, if not avoided, by embolization beyond the level of the cystic artery in the right hepatic artery. Liver abscess was also delayed after superselective AE by avoiding occlusion of lobar arterial branches, especially in patients with grade IV or V liver injuries. In our series, minimally invasive treatments, including laparoscopic cholecystectomy, percutaneous aspirate and catheter drainage, and laparoscopic peritoneal lavage/drainage, were given to 14 patients with gallbladder infarction, liver abscess or biloma formation, and bile leak due to selective AE. These complications mostly happened 6-8 weeks after liver injury and there was no severe side effect. Embolization of the extrahepatic arterial trunk was done in 13 patients because of their active extravasation in late arterial phase. During the embolization, complete occlusion of the extrahepatic trunk was not considered as a target, but used to control active extravasation and keep hemodynamics stable. Combined selective AE was also performed to stop the intrahepatic arterial bleeding. Selective AE can decrease the risk of hepatic ischemia, and avoid the rare complication of abdominal compartment syndrome.[18]
In conclusion, AE is an adjunct treatment for liver injuries. It is effective in controlling intrahepatic arterial bleeding in hemodynamically stable patients with high-grade liver injuries. Indications for AE should be considered with the hemodynamic condition of patients, trauma mechanism, and associated intra-abdominal injuries. Selective and/or super-selective AE should be advocated in order to decrease the incidence and severity of AE-related hepatobiliary complications.
Acknowledgements:We thank Dr. Zi-Ming Huang of Chinese PLA Air Force General Hospital for help with the study design and data collection.
Contributors:ZHY proposed the study. KYL performed research and wrote the first draft. HXJ, ZG and LCL collected the data. XM and ZYY analyzed the data. All authors contributed to the designand interpretation of the study and to further drafts. ZHY is the guarantor.
Funding:This study was supported by grants from the National Science and Technology Support program of China (2012BAI15B08) and the Chinese PLA Air Force Logistics Department Science Support program (BKJ02J001).
Ethical approval:This study was approved by the Ethics Committee of Chinese PLA Air Force General Hospital.
Competing interest:No benefits in any form have been received or will be received from a commercial party related directly or indirectly to the subject of this article.
1 Huang YC, Wu SC, Fu CY, Chen YF, Chen RJ, Hsieh CH, et al. Tomographic findings are not always predictive of failed nonoperative management in blunt hepatic injury. Am J Surg 2012;203:448-453.
2 van der Vlies CH, Olthof DC, Gaakeer M, Ponsen KJ, van Delden OM, Goslings JC. Changing patterns in diagnostic strategies and the treatment of blunt injury to solid abdominal organs. Int J Emerg Med 2011;4:47.
3 Yi IK, Miao FL, Wong J, Narasimhan KL, Lo RH, Yee L, et al. Prophylactic embolization of hepatic artery pseudoaneurysm after blunt abdominal trauma in a child. J Pediatr Surg 2010;45:837-839.
4 Wang YC, Fu CY, Chen YF, Hsieh CH, Wu SC, Yeh CC. Role of arterial embolization on blunt hepatic trauma patients with type I contrast extravasation. Am J Emerg Med 2011;29: 1147-1151.
5 Ochiai T, Igari K, Yagi M, Ito H, Kumagai Y, Iida M, et al. Treatment strategy for blunt hepatic trauma: analysis of 183 consecutive cases. Hepatogastroenterology 2011;58:1312-1315.
6 Moore EE, Cogbill TH, Jurkovich GJ, Shackford SR, Malangoni MA, Champion HR. Organ injury scaling: spleen and liver (1994 revision). J Trauma 1995;38:323-324.
7 Misselbeck TS, Teicher EJ, Cipolle MD, Pasquale MD, Shah KT, Dangleben DA, et al. Hepatic angioembolization in trauma patients: indications and complications. J Trauma 2009;67:769-773.
8 Kozar RA, Moore FA, Moore EE, West M, Cocanour CS, Davis J, et al. Western Trauma Association critical decisions in trauma: nonoperative management of adult blunt hepatic trauma. J Trauma 2009;67:1144-1149.
9 Velmahos GC, Toutouzas K, Radin R, Chan L, Rhee P, Tillou A, et al. High success with nonoperative management of blunt hepatic trauma: the liver is a sturdy organ. Arch Surg 2003;138:475-481.
10 Yanar H, Ertekin C, Taviloglu K, Kabay B, Bakkaloglu H, Guloglu R. Nonoperative treatment of multiple intraabdominal solid organ injury after blunt abdominal trauma. J Trauma 2008;64:943-948.
11 Hashemzadeh SH, Hashemzadeh KH, Dehdilani M, Rezaei S. Non-operative management of blunt trauma in abdominal solid organ injuries: a prospective study to evaluate the success rate and predictive factors of failure. Minerva Chir 2010;65:267-274.
12 Richardson JD. Changes in the management of injuries to the liver and spleen. J Am Coll Surg 2005;200:648-669.
13 Jiang H, Wang J. Emergency strategies and trends in the management of liver trauma. Front Med 2012;6:225-233.
14 Letoublon C, Morra I, Chen Y, Monnin V, Voirin D, Arvieux C. Hepatic arterial embolization in the management of blunt hepatic trauma: indications and complications. J Trauma 2011;70:1032-1037.
15 Bhullar IS, Frykberg ER, Siragusa D, Chesire D, Paul J, Tepas JJ 3rd, et al. Selective angiographic embolization of blunt splenic traumatic injuries in adults decreases failure rate of nonoperative management. J Trauma Acute Care Surg 2012;72:1127-1134.
16 Letoublon C, Chen Y, Arvieux C, Voirin D, Morra I, Broux C, et al. Delayed celiotomy or laparoscopy as part of the nonoperative management of blunt hepatic trauma. World J Surg 2008;32:1189-1193.
17 Kozar RA, Moore JB, Niles SE, Holcomb JB, Moore EE, Cothren CC, et al. Complications of nonoperative management of highgrade blunt hepatic injuries. J Trauma 2005;59:1066-1071.
18 Chen RJ, Fang JF, Lin BC, Kao JL. Laparoscopic decompression of abdominal compartment syndrome after blunt hepatic trauma. Surg Endosc 2000;14:966.
Received October 6, 2012
Accepted after revision July 22, 2013
Author Affiliations: Hepatobiliary Surgery Department, Chinese PLA Air Force General Hospital, Beijing 100142, China (Kong YL, Zhang HY, He XJ, Zhao G, Liu CL, Xiao M and Zhen YY)
Hong-Yi Zhang, MD, Hepatobiliary Surgery Department, Chinese PLA Air Force General Hospital, Beijing 100142, China (Tel: 86-10-66928312; Fax: 86-10-66927612; Email: kjzygdwk@163. com)
© 2014, Hepatobiliary Pancreat Dis Int. All rights reserved.
10.1016/S1499-3872(14)60027-8
杂志排行
Hepatobiliary & Pancreatic Diseases International的其它文章
- Pancreatic fistula after central pancreatectomy: case series and review of the literature
- FBW7 increases chemosensitivity in hepatocellular carcinoma cells through suppression of epithelialmesenchymal transition
- Pancreatic head cancer in patients with chronic pancreatitis
- Multi-visceral resection of locally advanced extra-pancreatic carcinoma
- Instrumental detection of cystic duct stones during laparoscopic cholecystectomy
- Improved anterior hepatic transection for isolated hepatocellular carcinoma in the caudate
