Primary graft dysfunction after liver transplantation
2014-05-04XiaoBoChenandMingQingXu
Xiao-Bo Chen and Ming-Qing Xu
Chengdu, China
Primary graft dysfunction after liver transplantation
Xiao-Bo Chen and Ming-Qing Xu
Chengdu, China
BACKGROUND:Primary graft dysfunction (PGD) causes complications in liver transplantation, which result in poor prognosis. Recipients who develop PGD usually experience a longer intensive care unit and hospital stay and have higher mortality and graft loss rates compared with those without graft dysfunction. However, because of the lack of universally accepted definition, early diagnosis of graft dysfunction is difficult. Additionally, numerous factors affect the allograft function after transplantation, making the prediction of PGD more difficult. The present review was to analyze the literature available on PGD and to propose a definition.
DATA SOURCE:A search of PubMed (up to the end of 2012) for English-language articles relevant to PGD was performed to clarify the characteristics, risk factors, and possible treatments or interventions for PGD.
RESULTS:There is no pathological diagnostic standard; many documented definitions of PGD are different. Many factors, such as donor status, procurement and transplant process and recipient illness may affect the function of graft, and ischemiareperfusion injury is considered the direct cause. Potential managements which are helpful to improve graft function were investigated. Some of them are promising.
CONCLUSIONS:Our analyses suggested that the definition of PGD should include one or more of the following variables: (1) bilirubin ≥10 mg/dL on postoperative day 7; (2) international normalized ratio ≥1.6 on postoperative day 7; and (3) alanine aminotransferase or aspartate aminotransferase >2000 IU/L within 7 postoperative days. Reducing risk factors may decrease the incidence of PGD. A majority of the recipients could recover from PGD; however, when the graft progresses intoprimary non-function, the patients need to be treated with retransplantation.
(Hepatobiliary Pancreat Dis Int 2014;13:125-137)
graft function;
primary graft dysfunction;
initial poor function;
primary non-function;
liver transplantation
Introduction
Liver transplantation (LT) has evolved from a risky procedure associated with a high mortality and morbidity to a standard and predominantly effective treatment for patients with end-stage liver diseases, and one-year graft survival averages more than 80% at the majority of treatment centers.[1,2]Because of the increased gap between liver resources and its requirements, marginal organs/donors are used routinely for the sickest transplantation recipients. Severe complications, such as primary graft dysfunction (PGD), can develop in this situation. Recipients with graft dysfunction usually experience a longer intensive care unit (ICU) and hospital stay, increased mortality and higher graft loss than those without graft dysfunction. Numerous conditions can affect the initial function of the allograft after transplantation. Therefore, understanding and detecting these conditions earlier and predicting early graft dysfunction are very important in decreasing the mortality and morbidity caused by PGD after LT. Unfortunately, because there is no uniform definition of PGD, the various definitions (supported by different transplant centers and involving many factors associated with PGD) impede or confuse the recognition of PGD as a complication of LT. Therefore, our aims are, by reviewing the relevant literature, to propose a definition, to identify risk factors, to summarize clinical features, and to recommend the management of PGD.
There is no consensus on the definitions of PGD,initial poor function (IPF), and primary non-function (PNF). However, it is universally accepted that PGD of the liver consists of IPF and PNF, which exhibit different degrees of severity; IPF and PNF are different stages of PGD. IPF is a borderline syndrome and directly influences the survival of the liver allograft. The majority of grafts at IPF are reversible because of their considerable regeneration potential; however, once grafts progress to PNF, the grafts will ultimately progress to graft loss. PNF is characterized by hepatic cytolysis, rapidly rising levels of transaminases, the absence of bile production, severe liver-related coagulation deficiency, high lactate levels, hepatic hemodynamic instability, hypoglycemia and acute renal and respiratory failure.[3-5]
IPF
Currently, there is no universal definition of IPF; different studies use different endpoints and scoring systems (Table 1). Most studies assess IPF based on time intervals during the first postoperative days or weeks and use liver-related laboratory parameters such as alanine aminotransferase (ALT) and asparate aminotransferase (AST) and prothrombin activity.[6-11]Ploeg et al[6]defined IPF as an AST of more than 2000 IU/L, a prothrombin time greater than 16 seconds, and an ammonia level greater than 50 µmol/L between postoperative days 2 and 7. This definition is widely used because it includes AST (indicating hepatocyte injury) and prolonged prothrombin time (indicating reduced synthetic ability). Nanashima and colleagues[7]recommended that an ALT and/or AST is greater than 1500 IU/L for 2 consecutive measurements within the first 72 hours after LT, whereas Dhillon et al[8]suggested that an average level of transaminase greater than 986 IU/L on postoperative day 2. Pokorny et al[3]used AST plus clotting factor support and bile production to evaluate IPF. Broering et al[9]defined primary poor function as ALT or AST>2000 IU/L or fresh frozen plasma being substituted for more than 5 days postoperatively. Nemes et al[12]selected the quotient of serum bilirubin (µmol/L) and prothrombin (percent) at postoperative day 5 to define IPF, González et al[13]used peak serum ALT values, mean bile output and lowest prothrombin activity to score early postoperative graft function. But in these studies the cutoff levels for the parameters were chosen arbitrarily based on the experiences of different centers. Statistically, the Nanashima criteria demonstrate a high concordance with the González criteria for the definition of early postoperative graft function and for predicting graft and patient survival.[14]However, similar tests for predicting graft function can have unequal predictive efficacy for IPF defined by González et al compared with the prediction of IPF defined by Ploeg et al.[15]Moreover, in the study conducted by Heise et al,[10]the incidence of IPF varied according to the scoring systems.
Although a number of the criteria described above demonstrated a high consistency in defining early postoperative graft function and predicting graft andpatient survival,[14]they failed to predict graft function at an earlier stage and failed to predict the dynamic transformation of graft function over a longer period. Moreover, these definitions lagged behind any real change in graft function and were only established when all the clinical signs pointed to IPF. Olthoff et al[16]proposed a simple definition of IPF, stating that IPF is present when one or more of the following variables are observed: (1) bilirubin ≥10 mg/dL on postoperative day 7; (2) international normalized ratio (INR) ≥1.6 on postoperative day 7; and (3) ALT or AST >2000 IU/L within 7 postoperative days. This definition was tested for association with graft and patient survival, validating previously published criteria. Heise et al[10]also developed a new scoring system based on the statistical significance for long-term survival calculated using ALT, AST, bile production, and prothrombin activity on days 1, 3, 7, and 14 after transplantation. This scoring system allows the diagnosis of IPF easily after postoperative day 3 because the levels required for diagnosis are dynamical according to postoperative time points and significantly lower than other criteria at the onset of IPF, and the relocation of patients between individual groups can be detected during the postoperative days. Moreover, patients who meet the criteria of IPF over 7 days after LT can be included in this analysis. Lock et al[17,18]used the maximal liver function capacity (LiMAx) test within 24 hours of LT to classify liver function. This test reflects graft performance in real-time and evaluates graft function from the very beginning. Because initial graft function is a major factor influencing the pharmacokinetics of the drug tacrolimus, the LiMAx test may also provide a guide adjusting the dosage of tacrolimus before toxic or insufficient levels of the drug appear within the first week after LT.[17]Predicting IPF via the detection of gene associations may also provide information before the organ is transplanted.[19]These new scoring systems appear more reliable and accurate at predicting IPF than previous systems. However, doctors may find that the time-consuming techniques and challenging equipment needed for these criteria are not feasible for routine clinical use.
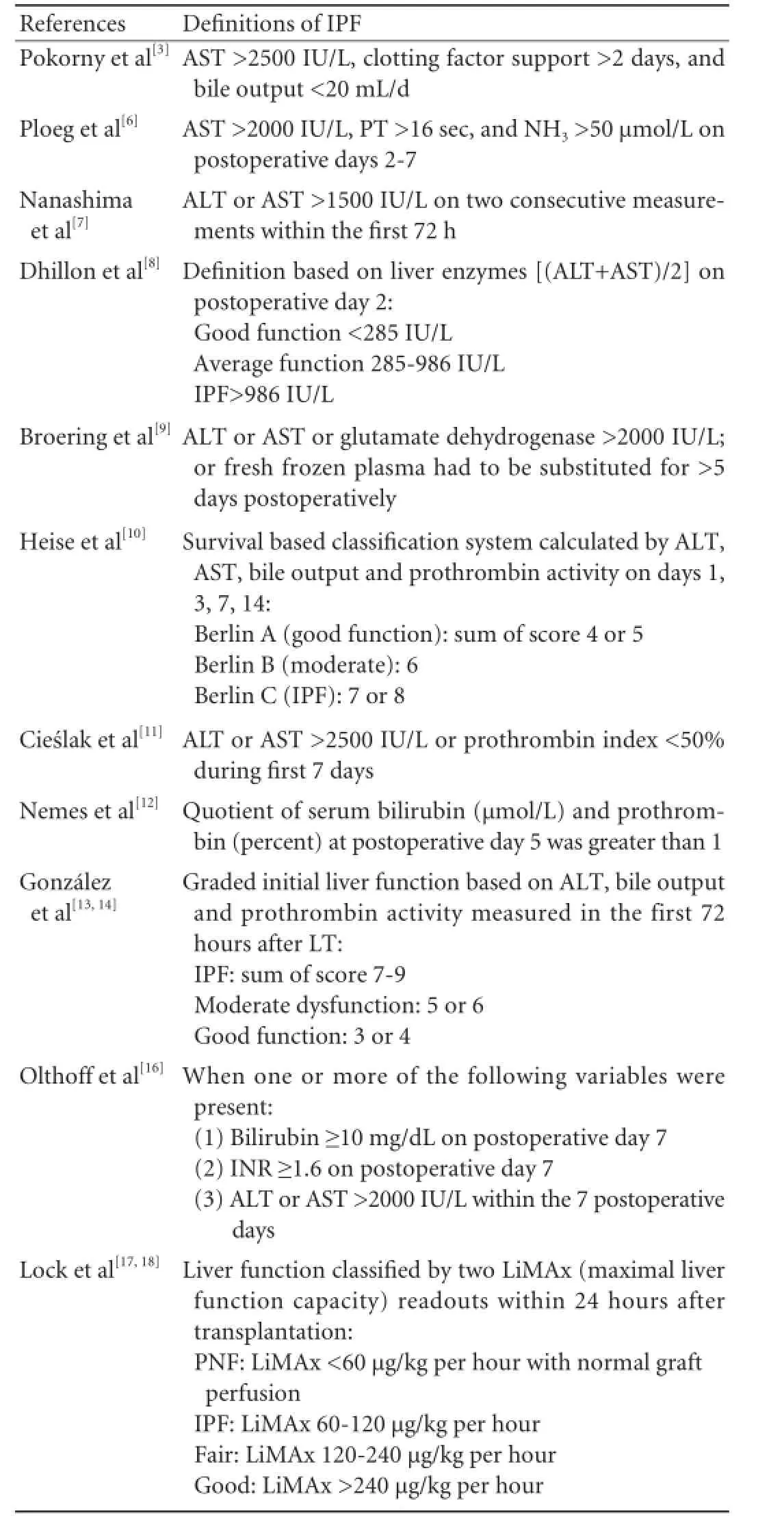
Table 1. Definitions of IPF
PNF
Although a uniform definition of PNF has not been established (Table 2), it is generally accepted that without immediate re-transplantation, PNF leads to graft loss. A progressive increase in the serum transaminase level is detected within the first 24 to 48 hours in transplant recipients who develop PNF. Bile and urine output decreases, serum bilirubin increases, and the synthetic function of the allograft decreases or fails during the same period. Furthermore, hepatic encephalopathy, uncorrectable coagulopathy, and hypoglycemia are observed, resulting in hyperkalemia, metabolic acidosis, and oliguric renal failure. Most investigators use IPF to define PNF after LT,[7,8,20]and this definition is in accordance with the concept of PGD. A number of investigators define PNF using the vague terms "failure" or "non-life sustaining function",[6,21,22]whereas others use aggressive clinical features or recipient status, such as encephalopathy, metabolic acidosis, etc., to explain PNF.[23]
Notably, most definitions of PNF are proposed retrospectively; these definitions exclude other factors that lead to graft loss within a specific period. Kremers et al[24]defined PNF explicitly, including definite cutoffs for transaminase levels, bile production, and coagulopathy. An exact definition was also proposed by the United Network for Organ Sharing (UNOS), which facilitates re-transplantation scheduling.

Table 2.Definitions of PNF
Incidence of PGD
The incidence of IPF and PNF varies between studies because of the different criteria chosen. Table 3 shows the incidence of PGD in the studies reviewed, regardless of the definitions chosen for IPF or PNF, the organ allocation system, the inclusion and exclusion criteria for the patients, etc. The incidence of IPF ranged from 5.2% to 36.3%, whereas the incidence of PNF from 0.9% to 7.2%.
Risk factors for PGD
Donor, procurement, transplantation procedure and recipient status all affect the initial graft function after LT.[20,25,26]Donor-related factors, such as age, nutritional status, the severity of fatty infiltration in the liver, hemodynamic stability during harvesting, liver allograft injury, and ischemia time during procurement, as well as recipient-related factors, such as recipient status and transplantation type, can affect allograft function (Table 4).
Donor-related factors for PGD
Donor age
It is inconclusive whether donor age is a risk factor or not,[2,20]older donors might be complicated with fatty liver, diabetes, celiac vessel arteriosclerosis, etc., and these risk factors increase significantly the risk of PGD. Advanced age impairs the regenerative capacity of the liver;[20]an older liver is more susceptible to hepatocyte injury, which may contribute to poor allograft function after transplantation. In an Scientific Registry of Transplant Recipients analysis, donors older than 50 or 60 years were associated with an increased risk for PNF compared with those younger than 40, demonstrating the significant role of donor age in the development of PNF.[25]The most controversial factor associated with donor age is the designation of a cutoff age. A number of reports suggest that a donor age of over 49 years[6,27]is a risk factor for PGD. However, Corradini et al[14]and Rull and colleagues[28]set this age at 65 years. Nevertheless, livers from advanced age donors for preferred recipients result in similar graft and patient survival rates compared with those from younger donors.[20]
Liver steatosis
The incidence of PNF after LT is 1.8% in normal grafts and 5.1% in those exhibiting greater than 30% steatosis. Therefore, steatosis greater than 30% in a donor liver is considered unacceptable.[29]However, other studies demonstrated that steatosis moderateto severe is acceptable when other risk factors are excluded.[30]The explanations that fatty liver causes PNF might be 1) the sinusoids disrupted by fat globules released from ruptured hepatocytes; 2) increased hepatocyte damage caused by fat solidification during cold preservation; 3) abnormal cell activation (especially Kupffer cell activation[31]) in the donor liver; and 4) the disturbance of hepatic microcirculation. These disturbances are characterized by narrow and irregular sinusoids, vascular congestion, and blood cell adhesion to the sinusoidal walls.[31]Lipid metabolism disturbance is prominent in hepatocytes exhibiting macrovesicular steatosis. Moreover, increased endothelial cells and hepatocyte oxidative injury could increase the vulnerability to secondary insults including warm/cold ischemia and cytokine surge after brain death.[32]These anomalies may eventually cause hepatocyte death and PNF after transplantation.
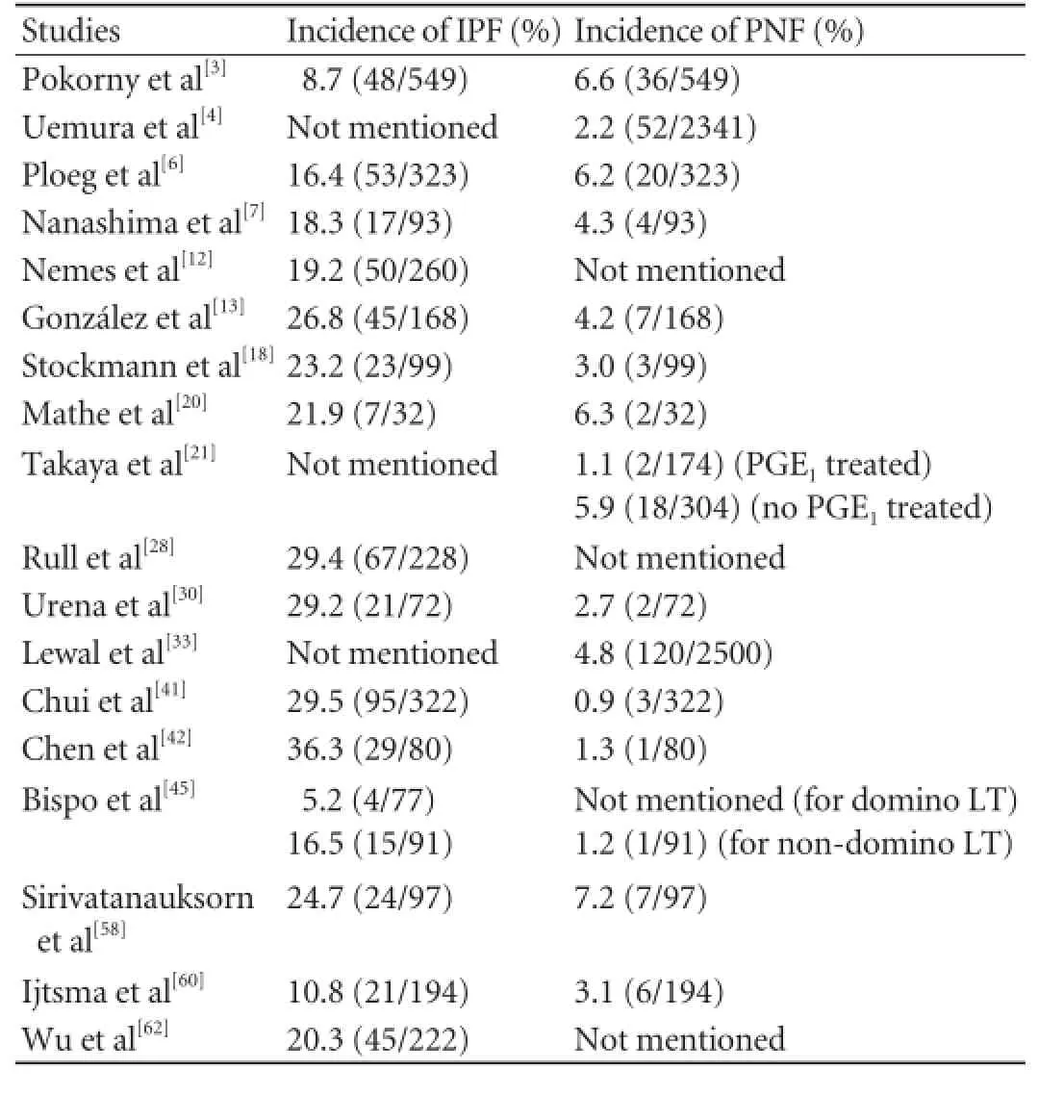
Table 3. Incidence of IPF and PNF in studies we reviewed (basing on different criteria)
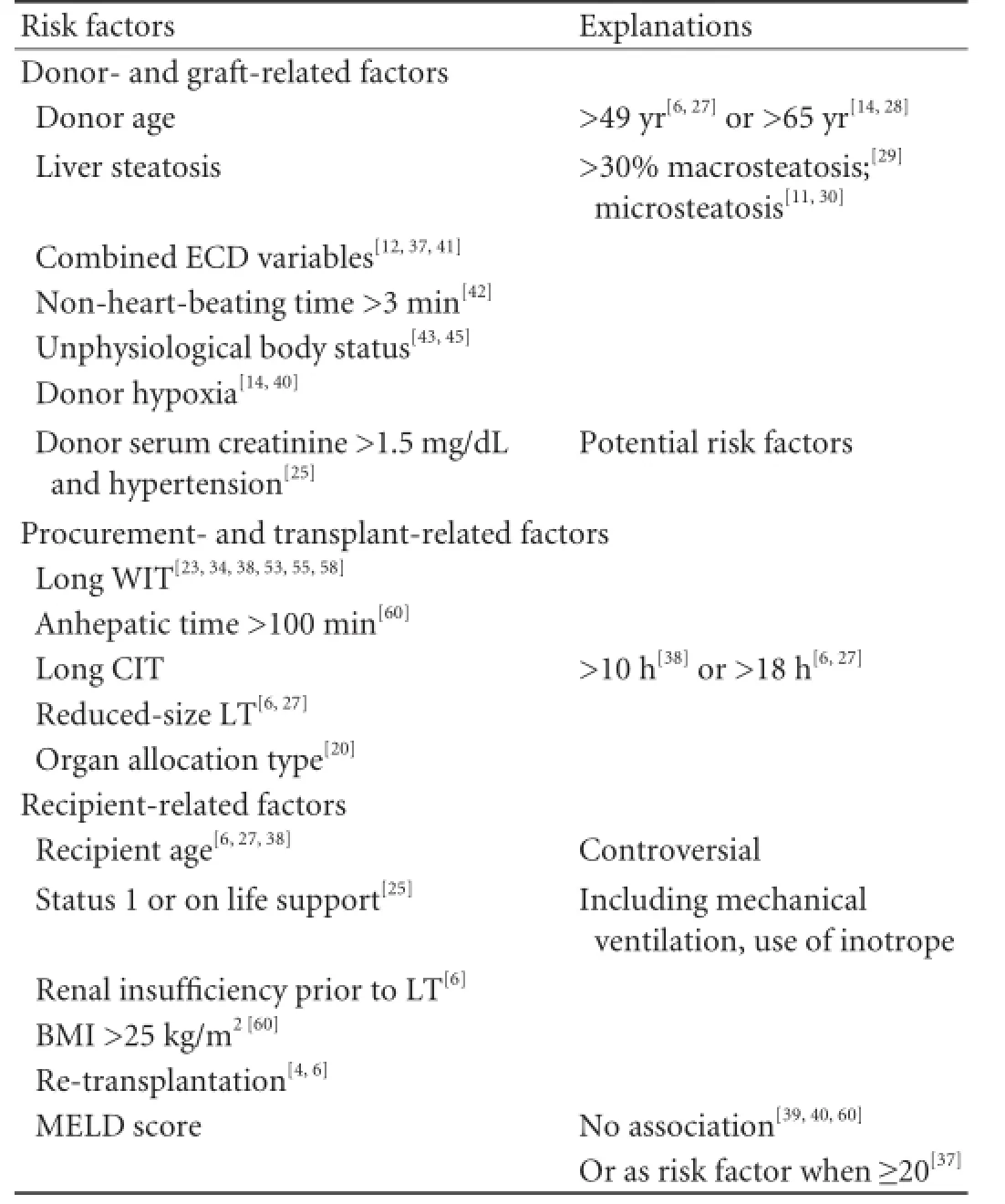
Table 4. Risk factors for PGD
Because microvesicular steatosis is frequently regarded as a mild, reversible condition, this is usually disregarded as a risk factor for IPF.[11]Microvesicular steatosis may develop because of severe and prolonged inhibition of mitochondrial β-oxidation of fatty acids during preservation-reperfusion injury.[33]Microvesicular steatosis increases progressively and evolves in the liver during cold storage and worsens significantly before reperfusion in the recipient, whereas the degree of macrovesicular steatosis remains constant.[34]It has been established that microvesicular steatosis in grafts is an independent factor influencing early graft function. Cieslak et al[11]observed that a 12% increase in microvesicular steatosis was equivalent to a 50% increased risk for IPF. Urena et al[30]reported that 50% of livers exhibiting a microvesicular change of greater than 30% resulted in IPF. Despite the IPF risk, the use of livers exhibiting microsteatosis does not decrease graft or patient survival rates.[30]
Expanded/extended criteria donor (ECD) livers
Because of the shortage of donor organs, the following methods have been developed to augment the donor pool: living donor LT, split LT, domino LT, the reuse of a transplanted liver, and the use of ECD/ marginal livers.[1,2,20,35,36]These "expanded liver donor criteria" have not been clearly established. The expanded criteria generally refer to donor factors that predispose recipients to poor initial graft function and/or increased long-term risk.[14,20,32,37-39]These factors include a donor age ≥60 years (or >50 years), obesity [body mass index (BMI) >27-30 kg/m2], macrovesicular steatosis>30%-50%, ICU stay >4-5 days, hypotensive episodes>1 hour with a mean or systolic blood pressure <60 mmHg, high vasopressor requirement (dopamine dose>10 µg/kg per minute or the use of other catecholamines at any dose), cardiac arrest, cold ischemia time >8 hours or 12-14 hours, warm ischemia time >40-45 minutes, peak serum sodium >150-155 mmol/L, sepsis, donor serum creatinine >1.2 mg/dL, hepatitis, alcoholism, bilirubin level >2.0 mg/dL, ALT >170 IU/L, and AST>150 IU/L. The use of ECD grafts exhibits an increased risk of PGD relative to the severity of the ischemiareperfusion (I/R) injury in the liver graft. This ECD includes nearly all donor-related factors for PGD (most of which are controversial, for example, elevated serum sodium,[2,3,13,38]longer stay in the hospital or ICU,[6,27,28]and noradrenaline usage[14,40]), although different cutoff levels for these variables have been proposed. The ECD criteria may provide an opportunity to analyze the combined efficacy of these potential risk factors. Many previously known risk factors are not clinically significant when evaluated independently; however, when these factors coexist, their influence becomes important.[41]The increased number of ECD variables indicates a higher incidence of PGD. The combination of an ECD ≥3 variables (or ≥2 variables[12]) and a model for end-stage liver diseases (MELD) score ≥9 (or >17[12]or a deteriorating Δ-MELD[39]) produce the worst scenario for graft outcome and PGD after LT.[37]Therefore, an impaired donor graft should not be used in a recipient with a high MELD score.[38]
Donors after cardiac death (DCD) and donors after brain death (DBD)
Prior to the establishment of brain death criteria in 1968, DCD (or non-heart-beating donors) was the only source of grafts and recognized as the only real and effective donors that can increase both adult and pediatric graft pools.[35]Donors with a non-heartbeating time >3 minutes are recognized as exhibiting independent risk factors for PGD.[42]
Although recognized as ideal donors outside the criteria for marginal donor organs, DBD may produce deleterious effects in donor organs because of brain death. Brain death is a catastrophic physiological event accompanied by an unphysiological body status. This status is associated with extensive physiological, immunological, and hormonal alterations that can lead to preservation injury and an increased rate of PNF.[43]The activation of hemostasis and dysregulated fibrinolysis in allografts from DBD have been recognized.[44]This prothrombotic state may lead to the formation of microthrombi in the graft, which may result in diminished organ function or an increased chance of graft dysfunction. Brain death exertsadditional detrimental effects on the graft, causing an autonomic storm and the rapid disintegration of the hypothalamic-hypophyseal axis, including endocrine changes, diffuse cellular mitochondrial injury, and lactic acidosis.[45]
Other donor-related factors
Donor hyperoxia is associated with good early graft function and longer graft and patient survival; however, a lower preharvest donor arterial partial pressure of oxygen (PaO2) is observed more frequently in IPF patients.[14,40]A hyperoxia status in donors could induce good early postoperative liver function because of an increased hepatic ATP content, enhanced protein synthesis, and a reduction in the proteolytic processes in the liver or a reduced sublethal burst of oxygen radicals such as that involved in the protection of ischemia preconditioning against liver cold ischemia injury.[14]A donor serum creatinine level >1.5 mg/dL, hypertension, and cerebrovascular accident appear to be possible risk factors for PNF.[25]
Donor risk index
The donor risk index provides a quantitative evaluation of the effect of the combined characteristics of the donor on LT outcomes. Feng et al[46]identified 7 donor and graft characteristics, which are significantly and independently associated with increased failure in deceased donor liver transplants, to facilitate the decision whether to proceed with transplantation; these characteristics are based on the quantitative assessment of the relative risk at the time of the organ offer. However, a high donor risk index does not mean that a liver is not transplantable; indeed, a high donor risk index could be used as an allocation strategy and in the search for an optimal donor-recipient combination to obtain the highest survival benefit.[47]
Procurement- and transplant-related factors for PGD
The risk factors for PGD during organ harvest and implantation are complex. Most factors are associated with I/R procedure and are technical in nature. I/R injury is recognized as the culprit of IPF and PNF of the organ in transplanted livers.[37,48-50]Hepatic I/R injury causes the infiltration of polymorphonuclear and T cells, activation of Kupffer and endothelial cells, and formation of reactive oxygen species/reactive nitrogen species (ROS/RNS), all of these lead to hepatocyte injury via cytotoxicity and inflammation.[48]The decrease in prostacyclin (PGI2) and thromboxane (TxA2) after I/R injury promotes the local adhesion of leukocytes and platelet aggregation.[51]Impaired sinusoidal cells and a disturbed liver microcirculatory system (both of which are mediated by activated oxygen radicals) are the primary causes of I/R injury.[33]Warm ischemia time (WIT) and cold ischemia time (CIT) are also included in the expanded donor criteria.
WIT
Sinusoidal endothelial cells are the cells in the liver most susceptible to cold ischemia, whereas hepatocytes are injured more readily by warm ischemia.[34]Damage to the hepatocytes is caused primarily by warm ischemia, which is exaggerated by cold preservation and reperfusion.[52]A WIT of 30 minutes plus 4-5 hours of cold preservation causes PNF in pig liver;[53]the longer the WIT, the greater the cumulative release of ALT, AST, and lactate dehydrogenase (LDH) in the perfusion solution.[54]However, a shorter WIT increases the graft tolerance to cold storage. Pig liver subjected to WIT for 20 minutes can endure 12 hours cold preservation in University of Wisconsin (UW) solution, and the time limit for this cold storage is less than 16 hours.[55]When the WIT is reduced to 10 minutes, a graft cold preservation time can be prolonged to 16 hours without early biliary necrosis (the limit for this prolongation is fewer than 20 hours).[56]Human graft livers without WIT can be preserved for more than 30 hours in UW solution, whereas a canine liver has been preserved for up to 48 hours in this solution.[57]Hepatocyte vacuolation, sinusoidal congestion, and the appearance and aggravation of focal hepatocyte dropout accompany increasing WITs.[23]Of these 3 features, the extent of vacuolation after warm ischemia (which reflects the degree of hepatocyte damage) correlates highly with PNF and may predict pig liver viability before LT. Prolonged WIT (>40 minutes[38]or >45 minutes[58]) is an independent risk factor for IPF and PNF. Nanashima et al[7]suggest that to reduce the incidence of IPF and PNF, the WIT should be less than 60 minutes. The minimization of WIT may improve graft and patient survival rates.[59]During the anhepatic period, rewarming ischemia injury occurs because of the increase in the allograft temperature. When this period persists for more than 100 minutes, IPF or PGD can occur.[60]Furthermore, the level of ALT or AST increases along with the re-warming ischemia. The recipient suffers simultaneously from acute hemodynamic changes and an eliminated hepatic metabolism, as well as cytokine, metabolite, and other toxin accumulation in the splanchnic system.[60]
CIT
Cold ischemia or cold storage is another factor thatinterferes with the incidence of PGD. The cutoff for CIT is not uniform; however, Johnson et al[25]and Cameron et al[38]reported that a CIT >10 hours is associated with poor outcomes after LT, and a number of studies have reported that CITs can be longer than 18 hours.[6,27]Decreasing temperatures can induce cell injury through the release of proteases, leading to alterations in calcium homeostasis, modifications of the cytoskeleton, and local tissue destruction.[19]Cold preservation also induces several changes in the hepatocytes, such as cell swelling, intracellular acidosis, loss of mitochondrial function, and decreased ATP. These changes may lead to PGD after LT.
Other factors, such as a shared transplant, rescue allocation organs, the use of a venovenous bypass, coagulopathy during the surgery, high platelet transfusion, and ATP depletion in the liver tissue, are associated with PGD. Longer operative time and blood loss are also potential risk factors.[58]Donor organs "shipped from other centers" or "from rescue allocation" appear to be associated with a higher incidence of IPF or PNF.[20]This may be attributed in part to longer CITs and unknown preservation injury during shipping. In LT, the severity of the endothelial cell damage is likely related to the degree of platelet consumption,[13]explaining why platelet transfusion can be a predictor of initial graft function.
Recipient-related factors for PGD
Many factors associated with recipients have been confirmed as risk factors for PGD. However, the contribution of the recipient age is controversial.[3,58]Cameron et al[38]asserted that a younger recipient and non-urgent recipient status minimize the risks of PNF. Other studies suggest the opposite, asserting that a younger recipient is associated with a higher PGD rate[6,27]because a reduced-size LT is performed increasingly in young recipients, which may influence the incidence of PGD. A high IPF rate could be explained by the reduction of the liver mass, a subsequent elevation in hepatocyte enzymes, and a slow recovering of synthetic function.[27]
Recipient-related factors (especially the severity of the recipient's illness) play a dominant role in the occurrence of PNF. This phenomenon is partially reflected by perioperative red blood cell transfusion,[60]elevated serum bilirubin and creatinine levels,[25]and reduced prothrombin activity. The MELD score is used as a predictor of mortality in patients awaiting LT.[12]This score prioritizes the more dire graft cases and can result in poorer patient survival.[39]However, a consistent incidence of PNF is found in livers allocated using the MELD score system.[25]A relationship has not been identified between the final MELD score of the recipients and the incidence of PGD,[39,40,60]with the exception of one report that an MELD score is a risk factor when it is ≥20.[37]
Other recipient-related factors, such as initial status, life support, mechanical ventilation, the use of inotrope, renal insufficiency prior to LT, hemodialysis, BMI >25 kg/m2, and re-transplantation, can lead to PGD after LT.[4, 6, 25, 60]
Diagnosis
Clinical features
Because IPF and PNF represent the 2 sequential stages of PGD, the manifestations of IPF and PNF overlap to some extent. Elevated serum transaminases, coagulopathy, and reduced bile output are the primary features of IPF, and PNF is the result of IPF. All of these clinical features described exacerbated in PNF. Additionally, hepatic encephalopathy, uncorrectable coagulopathy, and hypoglycemia are observed, causing hyperkalemia, metabolic acidosis, and oliguric renal failure in the patient. Patients at this stage either die or undergo re-transplantation.
Tests for predicting IPF or PNF
Improved technology has provided laboratory methods to predict early graft function pre- or posttransplantation. The LiMAx test can evaluate graft function immediately after LT.[17]Patients receiving massive blood transfusions develop acidosis followed by metabolic alkalosis early in the postoperative period, and this implies the recovery of liver allograft function[61]because the transformation of sodium citrate into sodium bicarbonate in banked blood is highly dependent on adequate hepatocyte function. An early lactate clearance rate below 24.8% with a high sensitivity of 95.5% and a specificity of 88.9% indicates an early prediction (within 6 hours) of IPF, as classified using the Nanashima definition.[62]High preoperative recipient plasma 7β-hydroxycholesterol,[40]insulinlike growth factor 1 (IGF-1) levels in recipients,[63]liver fatty acid-binding protein (L-FABP),[52]complement fragment 4d deposition,[34]and arterial ketone body ratio (AKBR)[21]may be indicators of IPF. The detection of (1) the genes that are highly expressed in the IPF liver tissue[19]and (2) the expression of the TLR4 loss-offunction allele[8]may provide new predictive methods at the gene or molecular level. However, unfortunately, the majority of these tests cannot be widely used in practice.Indocyanine green (ICG) clearance has also been used as a prognostic indicator of graft function after LT.[22]However, this indicator fails to provide information relevant to predicting individual patient outcomes in the early postoperative phase because the uptake and excretion of ICG are influenced by many factors, such as cholestasis or hyperbilirubinemia.[64]
Pathological clues
由此可见,经过40年的改革与创新,我国新闻出版业循着构建新体制、释放新动能、展现新活力、满足新需求的发展路径,建立起了事业与产业并行发展的社会主义新闻出版体制,实现了从单一事业体制向事业与产业并重的华丽转身,践行了“为人民服务、为社会主义服务”的根本宗旨。
Histological findings can identify pre-existing damage that may compromise the outcome of LT. I/R injury-related problems can also be detected before perfusion and early after engraftment. However, it appears that no distinctive histological changes are found in the allografts exhibiting PGD. However, biopsies of kidney allografts with PNF demonstrate acute tubular injury, antibody-mediated rejection, or thrombotic microangiopathy.[65]These pathological changes have also been observed in recipients without PNF but with delayed graft function, a phenomenon also observed in LT.
Biopsies of liver allografts with PNF taken in "backtable" and a few hours after transplantation usually demonstrate morphological changes caused by I/R injury. These changes include centrilobular hepatocyte swelling, hepatocanalicular cholestasis, periportal and perivenular congestion, hemorrhage, necrosis, and neutrophilic inflammation. Biopsies taken within 2 to 3 days after transplantation demonstrate ductular proliferation in the periportal region, acute cholangiolitis, hepatocyte swelling, and hepatocanalicular and cholangiolar cholestasis. These changes can also be observed in patients with sepsis.[66]Takaya et al[21]defined specific histopathological changes associated with PNF, namely, small infarcts and/or zonal hepatocyte coagulative necrosis (centrilobular or periportal) or severe cholestasis without evidence of rejection; however, these changes are not specific. Wisecaver et al[67]reported 2 cases of liver allograft PNF from donors with longstanding hypertension. Marked luminal narrowing of the medium and large intrahepatic arteries along with extensive hepatocyte necrosis were detected in these failed grafts. Endothelial lining morphologies could also be the surrogates of liver graft function after cold preservation and reperfusion because the sinusoidal endothelium is the most susceptible to cold ischemia damage.[34,68]Subcapsular wedge biopsies after reperfusion were performed by Koçbiyik et al[50]and suggested that morphologic features in deeper regions of the parenchyma, such as neutrophilic infiltration of the liver parenchyma (not subcapsular) and hepatocyte necrosis, reflect preservation injury and are indicative of an association with IPF. However, neutrophilic infiltration has also been detected in non-PNF patients.[33]The degree of liver dysfunction after LT can correlate strongly with histological changes, such as calcification and vacuole formation.[69]Light microscopy and electron microscopy analyses have demonstrated that patients who develop PNF demonstrate obvious calcification as well as severe vacuolization as a substitute for cell necrosis. Vacuolization and sinusoidal dilation persist in PNF grafts but are reversed in functioning livers after reperfusion.[23]Therefore, calcification, persisting vacuolization, and sinusoidal dilation could be pathological indicators of PNF; however, repeated biopsies will be required to confirm this hypothesis. Abnormal hepatocyte ultra-structure was observed in a small sample-size study of patients with PNF liver allografts.[33]Intra-mitochondrial crystalline inclusions were observed before and after perfusion using electron microscopy, although statistical significance was not demonstrated.
In summary, there is no established pathological diagnosis for IPF or PNF. Histological characteristics found in patients with PGD can also be found in organs suffering from I/R injury. Moreover, a pathological definition of either IPF or PNF should exclude other syndromes, such as sepsis, rejection, and delayed graft function.
Treatments of interventions for PGD
Although patients can recover from IPF without specific therapy, the recovery usually involves high postoperative costs for medications, laboratory or radiology tests, and blood products, as well as respiratory, physical, and supportive therapy. The normalization of graft function needs 28 days after LT, and the serum bilirubin and albumin may reach to control levels in 28 days.[18]The presentation of PNF is the most serious condition leading to allograft loss and recipient death without retransplantation.[58]There is no effective therapy for PNF except re-transplantation;[3]indeed, because of the risk factors associated with IPF and PNF, all interventions are prophylactic. Because I/R injury is considered the direct cause of IPF and further, PNF, many different methods for alleviating I/R injury have been investigated. The most obvious approach to minimize I/ R injury is to reduce the WIT and to limit the CIT; other possibilities include novel technical or pharmacological interventions (Table 5).[70]
Prostaglandin E1(PGE1)
PGE1, a biologically active polyunsaturated fattyacid derived from arachidonic acid, is used to treat PNF. PGE1prevents fulminant liver failure; therefore, PGE1reverses acute liver failure in freshly transplanted allografts.[21]PGE1reduces ischemia injury in the liver by stabilizing cellular integrity, enhancing tissue repair, and increasing arterial blood flow to the liver. PGE1infusion improves immediate hepatic allograft function, reduces blood product requirements, inhibits platelet aggregation, and prevents a drop in platelet count during LT. Foley and coworkers[1]administered PGE1(0.2-0.8 mg/kg per hour), vitamin E (1000 U), and N-acetylcysteine (6 g) to the recipients during liver transplantation and found that these remedies prevented PNF and improved the recipients' outcomes. Takaya et al[21]used PGE1perioperatively as a prophylactic for PNF; the initial dose was 0.2 µg/kg per hour, gradually increasing this dose to 0.6 µg/kg per hour and maintaining the dosage for the next 5 to 7 days. The incidence of PNF (1.1%) was significantly lower than that of the control (5.9%). However, a high incidence of PNF and postoperative deaths have also been reported despite the use of PGE1.[7]A meta-analysis produced no evidence that the administration of PGE1to LT patients reduces the risk of death, allograft PNF, or the need for liver re-transplantation.[51]Therefore, the effect of PGE1on PNF merits further investigation.
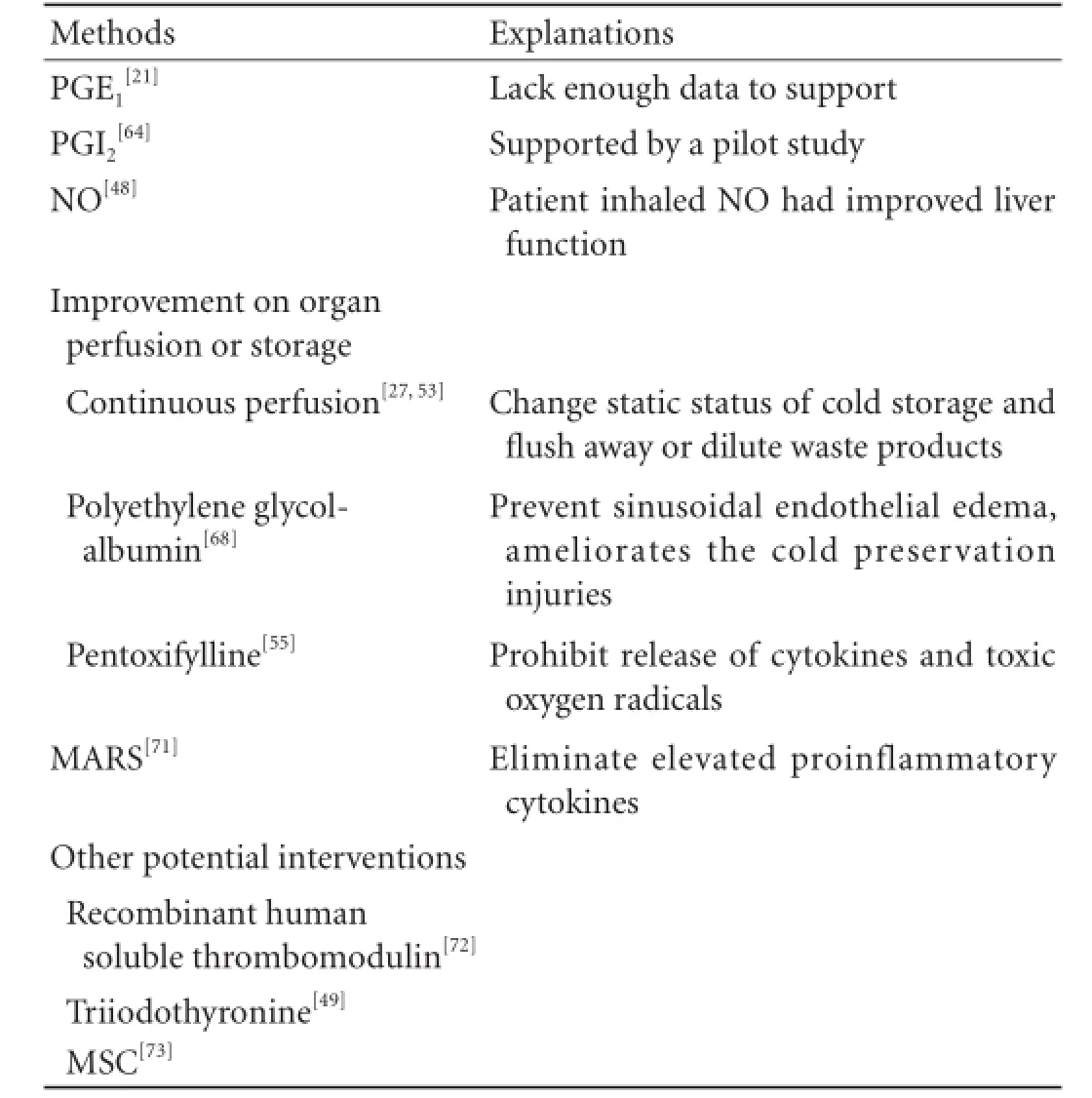
Table 5.Treatment or interventions for PGD
PGI2
PGI2is believed to play a superior role to PGE1with respect to the inhibition of platelet aggregation, and this fatty acid also inhibits the production of inflammatory cytokines.[64]When the PGI2analog iloprost was administered via continuous intravenous infusion for 7 days after LT, a lower incidence of PGD with improved synthetic function and increased excretory function was observed.
NO protects I/R injury via anti-inflammation, cytoprotection, the modulation of mitochondrial respiration, anti-oxidation, and the maintenance of vasomotor tone at the presinusoidal site within the hepatic sinusoid.[48]Patients inhaled NO (80 µg/mL) exhibit improved liver function (larger decreases in prothrombin time and partial thromboplastin time, as well as significantly decreased ALT and AST levels within 24 hours) after LT, which has been associated with the inhibition of hepatocyte death and early discharge from the hospital.[48]The inhalation of NO also decreases platelet usage (a risk factor of PGD) during surgery.
Improvements in organ perfusion and storage
A novel mechanical perfusion system was developed to preserve DCD liver grafts using the continuous perfusion of UW-gluconate at 4 ℃-6 ℃ for 3 hours after 2 hours of cold storage.[53]Toxic substrates and free radicals produced during cold storage can be eliminated using a continuous controlled perfusion flow of the portal vein and hepatic artery. The graft function before implantation can be evaluated simultaneously via the biochemistry examination of the effluent perfusion solution. Monitoring the pressure drop rate of the hepatic artery during machine perfusion may also be useful for evaluating liver graft viability.[54]This continuous perfusion can change the static status of cold storage, preventing time-dependent metabolic depression of the liver by flushing away or diluting waste products.[27]
When added to a UW solution, polyethylene glycolalbumin (PEG-Alb) prevents sinusoidal endothelial edema and ameliorates the cold preservation injuries of liver grafts.[68]It also could stable liver graft weight, reduce disturbance of the endothelial morphology, improve portal vein blood flow, and increase bile production in experimental rats. Pentoxifylline, a methylxanthine phosphodiesterase inhibitor, can inhibit the release of cytokines and toxic oxygen radicals from activated Kupffer cells and improve thehepatic microcirculation damaged during preservation and reperfusion.[55]When added to UW solution, pentoxifylline prolongs the cold preservation limits of pig liver grafts; the livers demonstrate a wellpreserved hepatic architecture and alleviate changes after reperfusion, such as hepatocyte swelling, sinusoid dilatation, hepatocyte apoptosis or necrosis, or severe damage of the sinusoids.
Molecular adsorbent recirculating system (MARS)
MARS utilizes albumin as a molecular adsorbent to remove albumin-bound liver toxins from patient's blood.[71]MARS has been used to treat acute liver failure and IPF after LT. MARS provides effective detoxification by eliminating elevated proinflammatory cytokines involved in hemodynamic and neurologic physiopathologies and improves Glasgow coma score. MARS can enhance a spontaneous recovery or act as a bridge to transplantation.[5,71]
Other potential interventions
Recombinant human soluble thrombomodulin (rTM) demonstrated promising results, it improves the viability of liver grafts in non-heart-beating rats by preventing warm I/R injury.[72]rTM improves allograft function including increased bile production and portal flow volume, lower ALT levels, and less histological changes. Triiodothyronine (T3), a known hepatic mitogen, can attenuate hepatic I/R injury in rats undergoing partial hepatectomy through the inhibition of proinflammatory cytokines, transcription factors, and adhesion molecules.[49]Bone marrow mesenchymal stem cells (MSCs) represent an alternative treatment.[73]The systemic infusion of MSCs via the tail in a rat model of 70% hepatic I/R injury led to the amelioration of hepatic injury. The prevention of liver enzyme release and improvement in the histology of acutely injured livers were observed.[74]
In addition to prophylactic therapy, biopsy and organ matching before transplantation is very important.[28,37]Pre-perfusion biopsies can reflect preexisting liver disease, including steatosis, steatohepatitis, and portal inflammation, whereas post-perfusion biopsies can exhibit fatty change, hepatocyte necrosis, and cholestasis. Biopsies can provide additional information for deciding whether the donor organ should be discarded; this information is crucial whether a marginal organ is suitable or not. The combination of risk factors should be carefully considered before a marginal allograft is transplanted because the use of marginal organs with more than 3 marginal criteria can have deleterious effects on initial graft function.[75]Surgically challenging recipients should not receive a marginal liver because the probability of survival is significantly lower.[28]
Re-transplantation
Early re-transplantation is the only effective therapy for PNF. The removal of the failing graft (rescue hepatectomy) before a liver becomes available can produce a dramatic temporary clinical improvement.[4]Successful re-transplantation for PNF can be performed; however, a longer ICU stay and a higher hemodialysis rate are observed, and the long-term patient and graft survival rates are similar to those observed for retransplantation for other reasons.
Conclusions
PGD consists of IPF and PNF. Both conditions imply a high mortality, a high graft failure rate, and a high retransplantation rate. Many reports have attempted to clarify the mechanism and risk factors for IPF and PNF, and a large number of risk factors, such as severe hepatic steatosis, long WIT or CIT, etc., have been confirmed. Several coexisting potential risk factors also influence the incidence of IPF or PNF, and various definitions for PGD coexist. In our opinion, a diagnosis of PGD should be made when one or more of the following variables are present: (1) bilirubin ≥10 mg/dL on postoperative day 7; (2) INR ≥1.6 on postoperative day 7; and (3) ALT or AST>2000 IU/L within 7 postoperative days. This definition has been validated for patient and graft survival. Interventions alleviating the risk factors of PNF have been investigated but there is no definitive benefit. Retransplantation is the only effective way to treat PNF.
Contributors:CXB wrote the main body of the article under the supervision of XMQ. XMQ is the guarantor.
Funding:None.
Ethical approval:Not needed.
Competing interest:No benefits in any form have been received or will be received from a commercial party related directly or indirectly to the subject of this article.
1 Foley DP, Fernandez LA, Leverson G, Chin LT, Krieger N, Cooper JT, et al. Donation after cardiac death: the University of Wisconsin experience with liver transplantation. Ann Surg 2005;242:724-731.
2 Sirivatanauksorn Y, Taweerutchana V, Limsrichamrern S, Kositamongkol P, Mahawithitwong P, Asavakarn S, et al. Analysis of donor risk factors associated with graft outcomes in orthotopic liver transplantation. Transplant Proc 2012;44:320-323.
3 Pokorny H, Gruenberger T, Soliman T, Rockenschaub S, Längle F, Steininger R. Organ survival after primary dysfunction of liver grafts in clinical orthotopic liver transplantation. Transpl Int 2000;13:S154-157.
4 Uemura T, Randall HB, Sanchez EQ, Ikegami T, Narasimhan G, McKenna GJ, et al. Liver retransplantation for primary nonfunction: analysis of a 20-year single-center experience. Liver Transpl 2007;13:227-233.
5 Novelli G, Morabito V, Lai Q, Levi Sandri GB, Melandro F, Pugliese F, et al. Glasgow coma score and tumor necrosis factor α as predictive criteria for initial poor graft function. Transplant Proc 2012;44:1820-1825.
6 Ploeg RJ, D'Alessandro AM, Knechtle SJ, Stegall MD, Pirsch JD, Hoffmann RM, et al. Risk factors for primary dysfunction after liver transplantation--a multivariate analysis. Transplantation 1993;55:807-813.
7 Nanashima A, Pillay P, Verran DJ, Painter D, Nakasuji M, Crawford M, et al. Analysis of initial poor graft function after orthotopic liver transplantation: experience of an australian single liver transplantation center. Transplant Proc 2002;34:1231-1235.
8 Dhillon N, Walsh L, Krüger B, Ward SC, Godbold JH, Radwan M, et al. A single nucleotide polymorphism of Tolllike receptor 4 identifies the risk of developing graft failure after liver transplantation. J Hepatol 2010;53:67-72.
9 Broering DC, Topp S, Schaefer U, Fischer L, Gundlach M, Sterneck M, et al. Split liver transplantation and risk to the adult recipient: analysis using matched pairs. J Am Coll Surg 2002;195:648-657.
10 Heise M, Settmacher U, Pfitzmann R, Wünscher U, Müller AR, Jonas S, et al. A survival-based scoring-system for initial graft function following orthotopic liver transplantation. Transpl Int 2003;16:794-800.
11 Cieślak B, Lewandowski Z, Urban M, Ziarkiewicz-Wróblewska B, Krawczyk M. Microvesicular liver graft steatosis as a risk factor of initial poor function in relation to suboptimal donor parameters. Transplant Proc 2009;41:2985-2988.
12 Nemes B, Gelley F, Zádori G, Piros L, Perneczky J, Kóbori L, et al. Outcome of liver transplantation based on donor graft quality and recipient status. Transplant Proc 2010;42:2327-2330.
13 González FX, Rimola A, Grande L, Antolin M, Garcia-Valdecasas JC, Fuster J, et al. Predictive factors of early postoperative graft function in human liver transplantation. Hepatology 1994;20:565-573.
14 Corradini SG, Elisei W, De Marco R, Siciliano M, Iappelli M, Pugliese F, et al. Preharvest donor hyperoxia predicts good early graft function and longer graft survival after liver transplantation. Liver Transpl 2005;11:140-151.
15 Olinga P, Maring JK, Groothuis GM, Kranenburg K, Merema M, Hof IH, et al. Value of the in vitro or in vivo monoethylglycinexylidide test for predicting liver graft function. Transplantation 1997;64:60-65.
16 Olthoff KM, Kulik L, Samstein B, Kaminski M, Abecassis M, Emond J, et al. Validation of a current definition of early allograft dysfunction in liver transplant recipients and analysis of risk factors. Liver Transpl 2010;16:943-949.
17 Lock JF, Malinowski M, Schwabauer E, Martus P, Pratschke J, Seehofer D, et al. Initial liver graft function is a reliable predictor of tacrolimus trough levels during the first posttransplant week. Clin Transplant 2011;25:436-443.
18 Stockmann M, Lock JF, Malinowski M, Seehofer D, Puhl G, Pratschke J, et al. How to define initial poor graft function after liver transplantation? - a new functional definition by the LiMAx test. Transpl Int 2010;23:1023-1032.
19 Defamie V, Cursio R, Le Brigand K, Moreilhon C, Saint-Paul MC, Laurens M, et al. Gene expression profiling of human liver transplants identifies an early transcriptional signature associated with initial poor graft function. Am J Transplant 2008;8:1221-1236.
20 Máthé Z, Paul A, Molmenti EP, Vernadakis S, Klein CG, Beckebaum S, et al. Liver transplantation with donors over the expected lifespan in the model for end-staged liver disease era: is Mother Nature punishing us? Liver Int 2011;31: 1054-1061.
21 Takaya S, Doyle H, Todo S, Irish W, Fung JJ, Starzl TE. Reduction of primary nonfunction with prostaglandin E1after clinical liver transplantation. Transplant Proc 1995;27: 1862-1867.
22 Escorsell À, Mas A, Fernández J, García-Valdecasas JC. Limitations of use of the noninvasive clearance of indocyanine green as a prognostic indicator of graft function in liver transplantation. Transplant Proc 2012;44:1539-1541.
23 Monbaliu D, Libbrecht L, De Vos R, Vekemans K, Walter H, Liu Q, et al. The extent of vacuolation in non-heart-beating porcine donor liver grafts prior to transplantation predicts their viability. Liver Transpl 2008;14:1256-1265.
24 Kremers WK, van IJperen M, Kim WR, Freeman RB, Harper AM, Kamath PS, et al. MELD score as a predictor of pretransplant and posttransplant survival in OPTN/UNOS status 1 patients. Hepatology 2004;39:764-769.
25 Johnson SR, Alexopoulos S, Curry M, Hanto DW. Primary nonfunction (PNF) in the MELD Era: An SRTR database analysis. Am J Transplant 2007;7:1003-1009.
26 D'Alessandro AM, Fernandez LA, Chin LT, Shames BD, Turgeon NA, Scott DL, et al. Donation after cardiac death: the University of Wisconsin experience. Ann Transplant 2004;9:68-71.
27 Brokelman W, Stel AL, Ploeg RJ. Risk factors for primary dysfunction after liver transplantation in the University of Wisconsin solution era. Transplant Proc 1999;31:2087-2090.
28 Rull R, Vidal O, Momblan D, González FX, López-Boado MA, Fuster J, et al. Evaluation of potential liver donors: limits imposed by donor variables in liver transplantation. Liver Transpl 2003;9:389-393.
29 Uzun MA, Koksal N, Kadioglu H, Gunerhan Y, Aktas S, Dursun N, et al. Effects of N-acetylcysteine on regeneration following partial hepatectomy in rats with nonalcoholic fatty liver disease. Surg Today 2009;39:592-597.
30 Ureña MA, Ruiz-Delgado FC, González EM, Segurola CL, Romero CJ, García IG, et al. Assessing risk of the use of livers with macro and microsteatosis in a liver transplant program. Transplant Proc 1998;30:3288-3291.
31 Teramoto K, Bowers JL, Kruskal JB, Clouse ME. Hepatic microcirculatory changes after reperfusion in fatty and normal liver transplantation in the rat. Transplantation 1993;56:1076-1082.
32 Gordon Burroughs S, Busuttil RW. Optimal utilization of extended hepatic grafts. Surg Today 2009;39:746-751.
33 Lawal A, Florman S, Fiel MI, Gordon R, Bromberg J, SchianoTD. Identification of ultrastructural changes in liver allografts of patients experiencing primary nonfunction. Transplant Proc 2005;37:4339-4342.
34 Silva MA, Mirza DF, Murphy N, Richards DA, Reynolds GM, Wigmore SJ, et al. Intrahepatic complement activation, sinusoidal endothelial injury, and lactic acidosis are associated with initial poor function of the liver after transplantation. Transplantation 2008;85:718-725.
35 Ciria R, Briceno J, Rufian S, Luque A, Lopez-Cillero P. Donation after cardiac death: where, when, and how? Transplant Proc 2012;44:1470-1474.
36 Nafidi O, Letourneau R, Willems BE, Lapointe RW. Reuse of liver graft from a brain dead recipient. Clin Transplant 2007;21:773-776.
37 Briceño J, Ciria R, de la Mata M, Rufián S, López-Cillero P. Prediction of graft dysfunction based on extended criteria donors in the model for end-stage liver disease score era. Transplantation 2010;90:530-539.
38 Cameron AM, Ghobrial RM, Yersiz H, Farmer DG, Lipshutz GS, Gordon SA, et al. Optimal utilization of donor grafts with extended criteria: a single-center experience in over 1000 liver transplants. Ann Surg 2006;243:748-755.
39 Silberhumer GR, Pokorny H, Hetz H, Herkner H, Rasoul-Rockenschaub S, Soliman T, et al. Combination of extended donor criteria and changes in the Model for End-Stage Liver Disease score predict patient survival and primary dysfunction in liver transplantation: a retrospective analysis. Transplantation 2007;83:588-592.
40 Corradini SG, Micheletta F, Natoli S, Iappelli M, Di Angelantonio E, De Marco R, et al. High preoperative recipient plasma 7beta-hydroxycholesterol is associated with initial poor graft function after liver transplantation. Liver Transpl 2005;11:1494-1504.
41 Chui AK, Shi LW, Rao AR, Anasuya A, Hagl C, Pillay P, et al. Primary graft dysfunction after liver transplantation. Transplant Proc 2000;32:2219-2220.
42 Chen H, Peng CH, Shen BY, Deng XX, Shen C, Xie JJ, et al. Multi-factor analysis of initial poor graft function after orthotopic liver transplantation. Hepatobiliary Pancreat Dis Int 2007;6:141-146.
43 Weiss S, Kotsch K, Francuski M, Reutzel-Selke A, Mantouvalou L, Klemz R, et al. Brain death activates donor organs and is associated with a worse I/R injury after liver transplantation. Am J Transplant 2007;7:1584-1593.
44 Lisman T, Leuvenink HG, Porte RJ, Ploeg RJ. Activation of hemostasis in brain dead organ donors: an observational study. J Thromb Haemost 2011;9:1959-1965.
45 Bispo M, Marcelino P, Marques HP, Martins A, Perdigoto R, Aguiar MJ, et al. Domino versus deceased donor liver transplantation: association with early graft function and perioperative bleeding. Liver Transpl 2011;17:270-278.
46 Feng S, Goodrich NP, Bragg-Gresham JL, Dykstra DM, Punch JD, DebRoy MA, et al. Characteristics associated with liver graft failure: the concept of a donor risk index. Am J Transplant 2006;6:783-790.
47 Braat AE, Blok JJ, Putter H, Adam R, Burroughs AK, Rahmel AO, et al. The Eurotransplant donor risk index in liver transplantation: ET-DRI. Am J Transplant 2012;12:2789-2796.
48 Lang JD Jr, Teng X, Chumley P, Crawford JH, Isbell TS, Chacko BK, et al. Inhaled NO accelerates restoration of liver function in adults following orthotopic liver transplantation. J Clin Invest 2007;117:2583-2591.
49 Taki-Eldin A, Zhou L, Xie HY, Chen KJ, Yu D, He Y, et al. Triiodothyronine attenuates hepatic ischemia/reperfusion injury in a partial hepatectomy model through inhibition of proinflammatory cytokines, transcription factors, and adhesion molecules. J Surg Res 2012;178:646-656.
50 Koçbiyik A, Demirhan B, Sevmis S, Budakoglu I, Karakayali H, Haberal M. Role of postreperfusion subcapsular wedge biopsies in predicting initially poor graft function after liver transplantation. Transplant Proc 2009;41:2747-2748.
51 Cavalcanti AB, De Vasconcelos CP, Perroni de Oliveira M, Rother ET, Ferraz L Jr. Prostaglandins for adult liver transplanted patients. Cochrane Database Syst Rev 2011;9: CD006006.
52 Monbaliu D, de Vries B, Crabbé T, van Heurn E, Verwaest C, Roskams T, et al. Liver fatty acid-binding protein: an early and sensitive plasma marker of hepatocellular damage and a reliable predictor of graft viability after liver transplantation from non-heart-beating donors. Transplant Proc 2005;37:413-416.
53 Shigeta T, Matsuno N, Obara H, Mizunuma H, Kanazawa H, Tanaka H, et al. Functional recovery of donation after cardiac death liver graft by continuous machine perfusion preservation in pigs. Transplant Proc 2012;44:946-947.
54 Obara H, Matsuno N, Enosawa S, Shigeta T, Huai-Che H, Hirano T, et al. Pretransplant screening and evaluation of liver graft viability using machine perfusion preservation in porcine transplantation. Transplant Proc 2012;44:959-961.
55 Qing DK, Dong JH, Han BL, Chen XR. Cold preservation of pig liver grafts with warm ischemia and pentoxifylline-UW solution. Arch Med Res 2006;37:449-455.
56 Zheng SG, Feng XB, He ZP, Qing DK, Leng JJ, Dong JH. Experimental study on tolerance time limits from warm ischemia to cold preservation of liver grafts. Zhonghua Gan Zang Bing Za Zhi 2006;14:250-254.
57 Jamieson NV, Sundberg R, Lindell S, Claesson K, Moen J, Vreugdenhil PK, et al. Preservation of the canine liver for 24-48 hours using simple cold storage with UW solution. Transplantation 1988;46:517-522.
58 Sirivatanauksorn Y, Taweerutchana V, Limsrichamrern S, Kositamongkol P, Mahawithitwong P, Asavakarn S, et al. Recipient and perioperative risk factors associated with liver transplant graft outcomes. Transplant Proc 2012;44:505-508.
59 Lai Q, Molinaro A, Mennini G, Nudo F, Morabito V, Corradini SG, et al. Preoperative donor scores and postoperative early measures of graft function: relevance to the outcome of liver transplantation. Transplant Proc 2010;42:1209-1211.
60 Ijtsma AJ, van der Hilst CS, de Boer MT, de Jong KP, Peeters PM, Porte RJ, et al. The clinical relevance of the anhepatic phase during liver transplantation. Liver Transpl 2009;15: 1050-1055.
61 Driscoll DF, Bistrian BR, Jenkins RL, Randall S, Dzik WH, Gerson B, et al. Development of metabolic alkalosis after massive transfusion during orthotopic liver transplantation. Crit Care Med 1987;15:905-908.
62 Wu JF, Wu RY, Chen J, Ou-Yang B, Chen MY, Guan XD. Early lactate clearance as a reliable predictor of initial poor graft function after orthotopic liver transplantation. Hepatobiliary Pancreat Dis Int 2011;10:587-592.
63 Bassanello M, De Palo EF, Lancerin F, Vitale A, Gatti R, Montin U, et al. Growth hormone/insulin-like growth factor1 axis recovery after liver transplantation: a preliminary prospective study. Liver Transpl 2004;10:692-698.
64 Bärthel E, Rauchfuss F, Hoyer H, Habrecht O, Jandt K, Götz M, et al. Impact of stable PGI2analog iloprost on early graft viability after liver transplantation: a pilot study. Clin Transplant 2012;26:E38-47.
65 Webber A, Hambleton J, Chami A, Bang H, Seshan S, Sharma A, et al. Mean arterial blood pressure while awaiting kidney transplantation is associated with the risk of primary nonfunction. Transplantation 2012;93:54-60.
66 Gao ZH. Seeking beyond rejection: an update on the differential diagnosis and a practical approach to liver allograft biopsy interpretation. Adv Anat Pathol 2009;16:97-117.
67 Wisecaver JL, Radio SJ, Shaw BW Jr, Langnas AN, Markin RS. Intrahepatic arteriopathy associated with primary nonfunction of liver allografts. Hum Pathol 1994;25:960-963.
68 Abbas R, Kombu RS, Dignam D, Gunning W, Stulberg JJ, Brunengraber H, et al. Polyethylene glycol modified-albumin enhances the cold preservation properties of University of Wisconsin solution in rat liver and a hepatocyte cell line. J Surg Res 2010;164:95-104.
69 Tzimas GN, Afshar M, Emadali A, Chevet E, Vali H, Metrakos PP. Correlation of cell necrosis and tissue calcification with ischemia/reperfusion injury after liver transplantation. Transplant Proc 2004;36:1766-1768.
70 Aydin Z, Mallat MJ, Schaapherder AF, van Zonneveld AJ, van Kooten C, Rabelink TJ, et al. Randomized trial of shortcourse high-dose erythropoietin in donation after cardiac death kidney transplant recipients. Am J Transplant 2012;12: 1793-1800.
71 Novelli G, Annesini MC, Morabito V, Cinti P, Pugliese F, Novelli S, et al. Cytokine level modifications: molecular adsorbent recirculating system versus standard medical therapy. Transplant Proc 2009;41:1243-1248.
72 Kashiwadate T, Miyagi S, Hara Y, Akamatsu Y, Kawagishi N, Sekiguchi S, et al. Recombinant human soluble thrombomodulin (ART-123) prevents warm ischemiareperfusion injury in liver grafts from non-heart-beating donors. Transplant Proc 2012;44:369-372.
73 Zaim M, Karaman S, Cetin G, Isik S. Donor age and longterm culture affect differentiation and proliferation of human bone marrow mesenchymal stem cells. Ann Hematol 2012;91:1175-1186.
74 Pan GZ, Yang Y, Zhang J, Liu W, Wang GY, Zhang YC, et al. Bone marrow mesenchymal stem cells ameliorate hepatic ischemia/reperfusion injuries via inactivation of the MEK/ ERK signaling pathway in rats. J Surg Res 2012;178:935-948.
75 Pokorny H, Langer F, Herkner H, Schernberger R, Plöchl W, Soliman T, et al. Influence of cumulative number of marginal donor criteria on primary organ dysfunction in liver recipients. Clin Transplant 2005;19:532-536.
Received December 13, 2012
Accepted after revision August 9, 2013
Author Affiliations: Department of Liver and Vascular Surgery, West China Hospital, Sichuan University, Chengdu 610041, China (Chen XB and Xu MQ)
Ming-Qing Xu, MD, PhD, Department of Liver and Vascular Surgery, West China Hospital, Sichuan University, Chengdu 610041, China (Tel: 86-28-85422870; Fax: 86-28-85422867; Email: xumingqing0018@163.com)
© 2014, Hepatobiliary Pancreat Dis Int. All rights reserved.
10.1016/S1499-3872(14)60023-0
猜你喜欢
杂志排行
Hepatobiliary & Pancreatic Diseases International的其它文章
- Pancreatic fistula after central pancreatectomy: case series and review of the literature
- FBW7 increases chemosensitivity in hepatocellular carcinoma cells through suppression of epithelialmesenchymal transition
- Pancreatic head cancer in patients with chronic pancreatitis
- Multi-visceral resection of locally advanced extra-pancreatic carcinoma
- Instrumental detection of cystic duct stones during laparoscopic cholecystectomy
- Improved anterior hepatic transection for isolated hepatocellular carcinoma in the caudate
