The role of early nephrostomy in the management of patients with hyperkalaemia and renal failure due to ureteric obstruction
2014-03-22BhaskarKumarSomaniHarunGuptaAlastairTodd
Bhaskar Kumar Somani, Harun Gupta, Alastair Todd
1University Hospital Southampton NHS Trust, Southampton, UK.
2Leeds General Hospital, Leeds, UK.
3Raigmore Hospital, Inverness, UK.
The role of early nephrostomy in the management of patients with hyperkalaemia and renal failure due to ureteric obstruction
Bhaskar Kumar Somani1*, Harun Gupta2, Alastair Todd3
1University Hospital Southampton NHS Trust, Southampton, UK.
2Leeds General Hospital, Leeds, UK.
3Raigmore Hospital, Inverness, UK.
Objective: To assess the outcomes of early percutaneous nephrostomy in obstructed hydronephrosis and hyperkalaemia from ureteric obstruction.
Methods: Patients were diagnosed with hyperkalaemia with serum potassium >5.0 mmol/L and hyperkalaemia was graded as mild (5.0-6.0 mmol/L), moderate (6.1-7.0 mmol/L) or severe (>7.1 mmol/L). Data on age, sex, clinical presentation, presence of concurrent disease, creatinine, potassium, haemoglobin concentration, time interval in doing the nephrostomy since their first presentation, any prenephrostomy medical correction of hyperkalaemia and complications were collected.
Results: A total of 61 patients (40 males and 21 females) with mean age of 69.7 years (ranged 35 to 94 years) underwent 69 procedures. Prior to the nephrostomy, the serum potassium was mildly elevated in 42 cases, moderately elevated in 17 cases and severely elevated in 10 cases. The overall mean level of potassium before intervention was 6.1 mmol/L (range: 5.1 mmol/L-9.3 mmol/ L). Forty (58%) had nephrostomy without prior medical treatment of the hyperkalaemia. The mean serum potassium in these patients was 5.6 mmol/L (range: 5.1 mmol/L-7.5 mmol/L). Twentynine (42%) had medical treatment of the hyperkalaemia prior to nephrostomy. The mean potassium level in these patients was reduced from 6.7 mmol/L (range 5.4 mmol/L-9.3 mmol/L) before medical treatment to 5.8 mmol/L (4.0 mmol/L-7.4 mmol/L). Five patients (7%) had complications from percutaneous nephrostomy including temporary atrial fibrillation in 3 patients and transient pyrexia in 2 patients.
Conclusions: Percutaneous nephrostomy as the initial management for hyperkalaemia from ureteric obstruction is a safe procedure with acceptable complication rates.
ARTICLE INFO
Article history:
Received 11 January 2015
Received in revised form 13 January 2015
Accepted 15 January 2015
Available online 16 January 2015
Nephrostomy
1. Introduction
Hyperkalaemia is a common feature of acute kidney injury of any cause. Percutaneous nephrostomy (PCN) under local anaesthesia or retrograde ureteric stenting under general anaesthesia are effective treatments to relieve renal impairment due to ureteric obstruction[1]. Preprocedural hyperkalaemia is often a cause of concern for anaesthetic and radiological staff due to the associated risk of dysrhythmia and sudden death. Decompression of the ureteric obstruction either by PCN or retrograde ureteric stent usually improves renal function or hyperkalaemia with a low morbidity[2,3]. Retrograde ureteric stent insertion in patients with malignant ureteric obstruction carries a higher failure rate compared to PCN; furthermore the majority of patients will need a general anaesthetic which may be challenging when complicated with hyperkalaemia[4].
There are no specific guidelines on management of patients with hyperkalaemia due to ureteric obstruction. Wide variation in management exists in some patients undergoing dialysis, having infusion of dextrose/insulin, inhaling salbutamol or terbutaline and receiving oral/ rectal calcium resonium, and most patients having acombination of the above. Once the potassium is normalised, decompression of the ureter is achieved by either PCN or ureteric stenting. A handful of case reports, however, have suggested that early nephrostomy can help normalise the renal function and correct the potassium. Furthermore, no added morbidity has been reported following early nephrostomy. Whilst, as these case reports suggested, there are no large case series reported in the literature to verify the encouraging outcome. We hypothesised that an early nephrostomy in this group of patients without prior additional medical correction is effective without added morbidity. In order to test this hypothesis, we analysed our results with specific aims: 1. to assess the outcome of early nephrostomy in patients with ureteric obstruction, in particular the morbidity and outcome in terms of renal function and correction of hyperkalaemia; 2. to compare the outcomes of patients with and without medical treatment prior to hyperkalaemia. In some cases, medical management was commenced to prevent further increase in serum potassium whilst waiting nephrostomy and in others because intervention in a hyperkalaemic state was clinically considered hazardous in an unwell patient and drainage was delayed to allow for correction.
2. Materials and methods
We investigated the outcomes of patients who underwent nephrostomy for hyperkalaemia with renal failure secondary to ureteric obstruction between January 2003 and December 2008 at a single centre. Hyperkalaemia was defined as serum potassium greater than 5.0 mmol/ L and graded as mild (5.0 mmol/L-6.0 mmol/L), moderate (6.1 mmol/L-7.0 mmol/L) or severe (>7.1 mmol/L). Data was extracted from the radiology information system, biochemistry database, medical, interventional radiology and nursing notes and entered into a pre-designed data extraction sheets. Patients with no records available were excluded from the study. An experienced radiologist (AT) or registrar under supervision performed all procedures.
Following parameters were recorded for each patient: age, sex, clinical presentation, presence of concurrent disease, creatinine, potassium, haemoglobin concentration, time interval in doing the nephrostomy since their first presentation to the hospital, any pre-nephrostomy medical correction of hyperkalaemia and complications. The success of the procedure was defined as resolution of hyperkalaemia and improvement in renal function.
3. Results
During our study period, a total of 61 patients, 40 males and 21 female, with mean age of 69.7 years (range 35 to 94 years) underwent 69 procedures (Figures 1-3). All patients had hyperkalaemia and hydronephrosis due to ureteric obstruction. Pre-nephrostomy hydronephrosis was unilateral in 37 cases, bilateral in 27 cases, with one transplant kidney. In four patients the biochemistry failed to improve after unilateral nephrostomy and a subsequent contralateral nephrostomy was necessary.
The underlying cause was malignant ureteric obstruction in 46 patients, obstruction from ureteric calculi in 8 patients, pyonephrosis in 4 patients and obstruction from a combination of retroperitoneal fibrosis and/or inflammatory aortic aneurysm in the remaining three patients. Prior to the nephrostomy, the serum potassium was mildly elevated in 42 cases, moderately elevated in 17 cases and severely elevated in 10 cases. The overall mean potassium before intervention was 6.1 mmol/L (range: 5.1 mmol/L-9.3 mmol/L) (Table 1).
Twenty-nine (42%) had medical treatment of the hyperkalaemia prior to nephrostomy. This was to prevent further increase in serum potassium whilst waiting for a nephrostomy because intervention in a hyperkalaemic state was considered hazardous and drainage was delayed to allow correction (Figures 1a and 1b). Of these 29 cases, the mean potassium level was reduced from 6.7 mmol/L (range 5.4 mmol/L-9.3 mmol/L) before medical treatment to 5.8 mmol/L (4.0 mmol/L-7.4mmol/L) with a mean reduction of 0.9 mmol/L (range: 0.8 mmol/L-4.2 mmol/L) (Figure 3).A combination of medical measures was used for most patients, with insulin dextrose being the commonest (n=20), oral calcium resonium (n=17) and haemodialysis (n=8) in others. Mean delay from presentation to nephrostomy was 1.9 d.
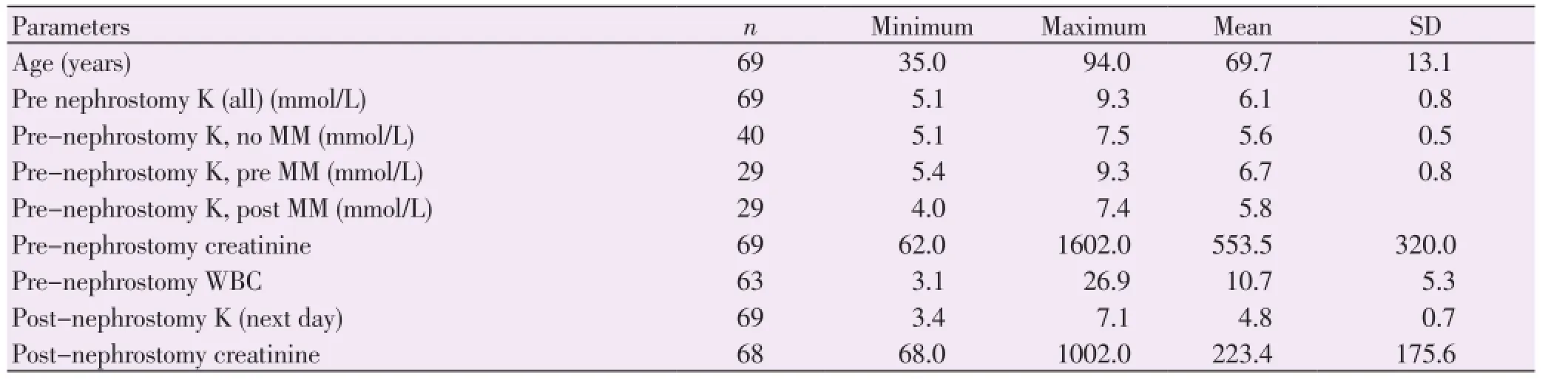
Table 1 Pre and post nephrostomy potassium, creatinine and WBC count.

Figure 1. ECG from patient with serum potassium of 9.3 mmol/L (a) and more normal ECG from the same patient after nephrostomy and normalisation of the serum potassium (b).In Figure 1a, the P waves are small, PR interval is prolonged; the QRS complex is widened at 154 ms; the T waves are taller than the R wave; the ST segment is sloping and the QT interval is long.

Figure 2. Algorithm showing outcomes of all patients undergoing PCN.
Forty (58%) had nephrostomy without prior medical treatment of the hyperkalaemia. The mean serum potassium in these patients was 5.6 mmol/L (range 5.1 mmol/L-7.5 mmol/L). Twenty-four of these procedures (60%) were done within 24 h of presentation. The mean time delay from presentation to nephrostomy was 1.4 d (range: 0-3 d).
Five patients (7%) had complications from PCN including atrial fibrillation (AF) in 3 patients and transient pyrexia in 2 patients, both of which settled with antibiotics. Of the three patients with AF, 2 had no medical treatment prior to nephrostomy. Whilst AF in two patients resolved spontaneously the third needed temporary treatment with verapamil. There were no other hyperkalaemia or procedure related complications.
Bilateral PCN was done in 27 cases, resulting in normalisation of the serum biochemistry in 22 (81%) cases. In the remaining 5 cases there was no improvement in the serum potassium or creatinine. Unilateral nephrostomy was performed initially in 37 cases, and one transplant kidney. In 25 (66%) cases there was normalisation of theserum potassium and creatinine, but with no significant improvement in other 13 cases. Of the latter, 2 cases needed the contralateral side drained and two other cases needed a repeat procedure due to nephrostomy catheter extrusion (Figure 1).
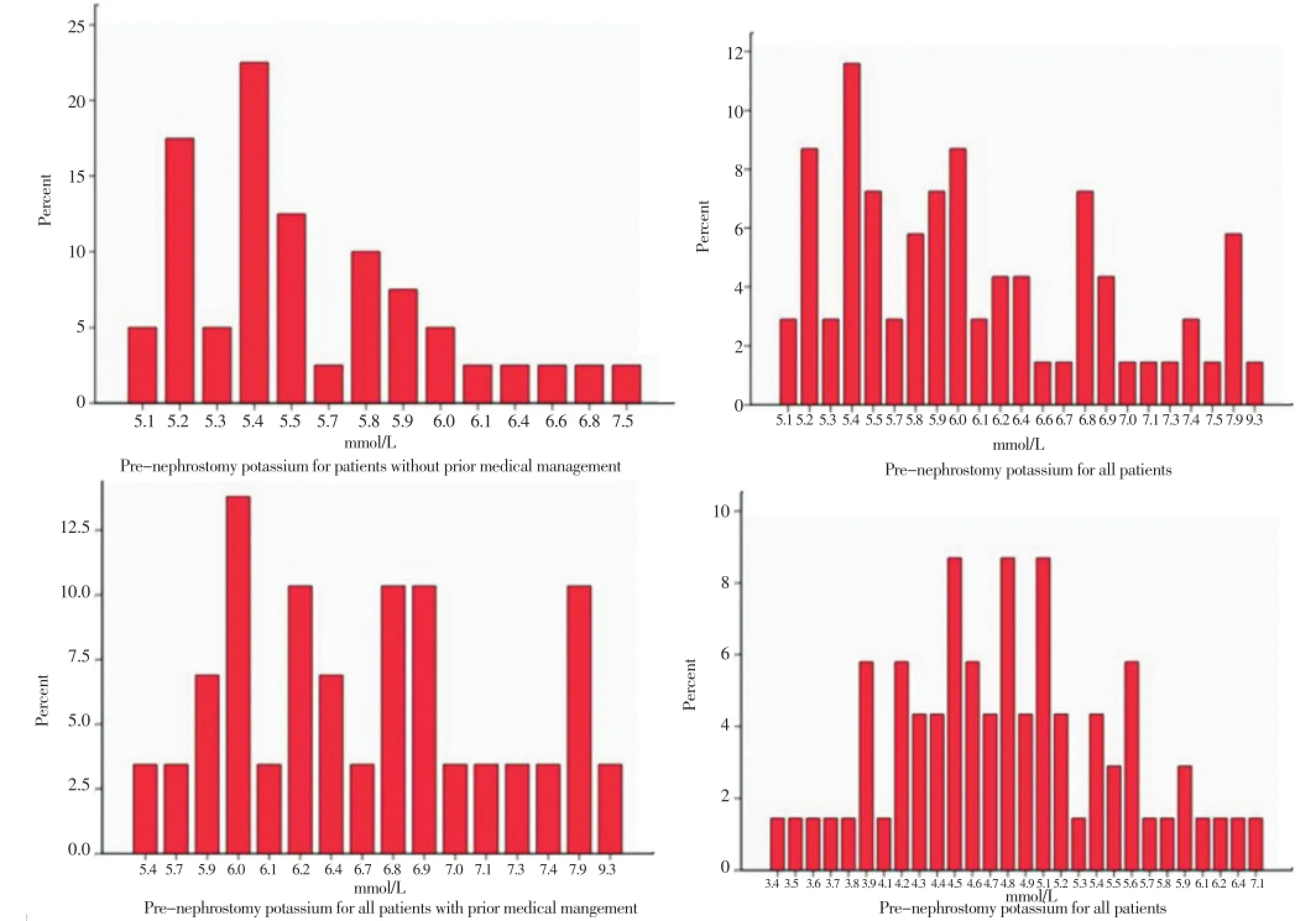
Figure 3. Pre- and post-nephrostomy potassium for patients with and without medical management.
4. Discussion
4.1. Principle findings
The safest and most effective treatment of hyperkalaemia due to obstructive uropathy is early relief of obstruction (drainage of both kidneys where there is bilateral hydronephrosis). From the data, there is no obvious relationship between the severity of hyperkalaemia, the response to nephrostomy and the time taken for potassium and creatinine to normalise after nephrostomy. In our study, initial PCN was performed within 24 h of presentation in 42 (62%) of patients and was successful in normalising serum potassium and creatinine in 50 (72%) and 25 (36%) of the patients within 48 h. The minor complication rate was 7%, with AF, pyrexia and confusion more likely in patients with stone disease and leucocytosis, but was not associated with severity of hyperkalaemia. The complications in our study were well within acceptable levels as published by the American College of Radiologists (4% haemorrhage and 10% septicaemia/ septic shock).
4.2. Limitations of the study
This study is limited by small size and retrospective data collection. However, the authors believe that there is an important message for clinicians dealing with hyperkalaemia due to obstructive uropathy and for radiologists providing this service. There is a selection bias in patients undergoing medical management prior to nephrostomy versus nephrostomy as the first line treatment. This was because no prior data existed on the safety of nephrostomy on hyperkalaemic patients, and for clinically unwell patients or where delay in arranging nephrostomy was anticipated, we wanted to correct the potassium level prior to nephrostomy.
4.3. Meaning of the study (possible mechanism and implications for future policy and practices)
The serum potassium and creatinine returned to normal post drainage after a mean of 1.6 d and 3.3 d respectively in50 patients in our study. Early nephrostomy is recommended for hyperkalaemia due to obstructive uropathy. There appears to be no advantage from reducing the serum potassium by medical means prior to intervention unless drainage is delayed. The risk of dying due to the arrythmogenic effect of hyperkalaemia during such a procedure is unclear but probably low with no fatalities reported in the literature. The urgency of the intervention is usually based on factors such as sepsis, pain, hyperkalaemia and the need for preservation of renal function especially in a solitary kidney. A large study of hospital in-patients confirmed the association of hyperkalaemia and increased mortality[5]. However there appeared to be a stronger association with the rate of change of serum potassium rather than the peak value. Levels of 10 mmol/L appear compatible with survival[6].
Identification of patients most at risk is difficult. The electrocardiographic changes of hyperkalaemia are unreliable especially in patients with chronic renal impairment partly due to associated serum calcium flux and partly due to poor observer sensitivity[5-9]. There are some evidences that other elevated metabolites in renal failure may be just as likely as potassium to cause cardiac or noncardiac morbidity[10]. Dialysis and other medical measures to decrease the serum potassium may be reassuring if drainage is not immediately available. However, dialysis requires the insertion of a central venous catheter and results in rapid electrolyte changes, both of which are potentially hazardous. The risk of cardiac arrhythmia and arrest for end stage renal patients are reported to be higher for dialysed than for nondialysed patients although this effect may not be significant in these unmatched groups[11,12].
Radiologists performing nephrostomies on patients with hyperkalaemia may be reassured by the absence of published cardiac complications. The rationale for prior medical treatment appears weak and this study found no reason to delay nephrostomy. However, this implies access to imaging and interventional expertise, which is by no means universal for UK hospital in-patients in spite of recent recommendations[13].
Our experience suggests that PCN need not be delayed for medical attempts to correct potassium unless the patient is haemodynamically compromised or there is a delay in arranging the nephrostomy. Early drainage of obstructive uropathy by PCN is an effective strategy to correct associated hyperkalaemia and restore renal function. PCN as the initial management for hyperkalaemia from ureteric obstruction is a safe procedure with acceptable complication rates. A careful attention to the agreed protocols/ algorithms, preprocedure antibiotic regimens, patient optimisation and a dedicated uro-radiology unit is essential to achieve optimal results.
Conflict of interest statement
The authors report no conflict of interest.
[1] Lynch MF, Anson KM, Patel U. Percutaneous nephrostomy and ureteric stent insertion for acute renal deobstruction: consensus based guidance. Br J Med Surg Urol 2008; 1(3): 120-125.
[2] Wilson JR, Urwin GH, Stower MJ. The role of percutaneous nephrostomy in malignant ureteric obstruction. Ann R Coll Surg Engl 2005; 87: 21-24.
[3] Gasparini M, Carroll P, Stoller M. Palliative percutaneous and endoscopic urinary diversion for malignant ureteral obstruction. Urology 1991; 38: 408-412.
[4] Hausegger KA, Portugaller HR. Percutaneous nephrostomy and antegrade ureteral stenting: technique-indications-complications. Eur Radiol 2006; 16(9): 2016-2030.
[5] Paice B, Gray JM, McBride D, Donnelly T, Lawson DH. Hyperkalaemia in patients in hospital. Br Med J (Clin Res Ed)1983; 286: 1189-1192.
[6] Ali Y, Gupta RK, Kehinde EO, Johnny KV. Extreme hyperkalaemia secondary to malignant ureteric obstruction: case report. East Afr Med J 2006; 83(11): 637-640.
[7] Aslam S, Friedman EA, Ifudu O. Electrocardiography is unreliable in detecting potentially lethal hyperkalaemia in haemodialysis patients. Nephrol Dial Transplant 2002; 17: 1639-1642.
[8] Wrenn KD, Slovis CM, Slovis BS. The ability of physicians to predict hyperkalemia from the ECG. Ann Emerg Med 1991; 20(11): 1229-1232.
[9] Montague BT, Ouellette JR, Buller GK. Retrospective review of the frequency of ECG changes in hyperkalemia. Clin J Am Soc Nephrol 2008; 3(2): 324-330.
[10] de Jager DJ, Grootendorst DC, Jager KJ, van Dijk PC, Tomas LM, Ansell D, et al Cardiovascular and noncardiovascular mortality among patients starting dialysis. JAMA 2009; 302(16): 1782-1789.
[11] US Renal Data System. USRDS 2009 Annual Data Report: atlas of chronic kidney disease and end-stage renal disease in the United States. Bethesda: National Institutes of Health, National Institute of Diabetes and Digestive and Kidney Diseases; 2009.
[12] ACR-SIR-SPR practice guideline for the performance of percutaneous nephrostomy. 2014. [Online] Available from: http://www.acr.org/~/media/ACR/Documents/PGTS/guidelines/ Percutaneous_Nephrostomy.pdf [Accessed on 9th January, 2015]
[13] Adding insult to injury. A review of care of patients who died in hospital with a primary diagnosis of acute kidney injury. London: NCEPOD; 2009. [Online] Available from: http://www.ncepod.org. uk/2009report1/Downloads/AKI_report.pdf [Accessed on 9th January, 2015]
ment heading
10.1016/S2221-6189(14)60060-3
*Corresponding author: Bhaskar K Somani, Consultant Urological Surgeon (Stone Lead) and Honorary Senior Lecturer, University Hospitals Southampton NHS Trust, Southampton, UK.
Tel: 02380795272
E-mail: bhaskarsomani@yahoo.com
Hyperkalaemia
Obstructed hydronephrosis
Renal failure
杂志排行
Journal of Acute Disease的其它文章
- Acute and sub-acute toxicity study of Clerodendrum inerme, Jasminum mesnyi Hance and Callistemon citrinus
- Time-critical AMI Detection: A novel and fast technique using the 12-lead ECG
- Epidemiological survey on scorpionism in Gotvand County, Southwestern Iran: an analysis of 1 067 patients
- The acute effect of the antioxidant drug “U-74389G” on red blood cells levels during hypoxia reoxygenation injury in rats
- Successful treatment of lower urinary tract obstruction with peritonealamniotic and vesicoamniotic shunting
- Simvastatin-induced Toxic Epidermal Necrolysis
