Bilateral mandibular distraction in micrognathism or hypoplasia of mandible, hazrat fatemeh hospital
2014-03-22MohammadEsmaiilHassaniHamidKarimiHoseinHassaniAliHassani
Mohammad-Esmaiil Hassani, Hamid Karimi, Hosein Hassani, Ali Hassani
1Assistant Professor of Plastic Surgery, Faculty of Medicine, Iran University of Medical Sciences, Tehran , Iran
2Family Practice, Davis University, Modesto, California, USA
3Family Practice , Michigan Medical University, Ann Arbor, Michigan, USA
Bilateral mandibular distraction in micrognathism or hypoplasia of mandible, hazrat fatemeh hospital
Mohammad-Esmaiil Hassani1, Hamid Karimi1, Hosein Hassani2, Ali Hassani3
1Assistant Professor of Plastic Surgery, Faculty of Medicine, Iran University of Medical Sciences, Tehran , Iran
2Family Practice, Davis University, Modesto, California, USA
3Family Practice , Michigan Medical University, Ann Arbor, Michigan, USA
Objective: To determine the results of Bilateral Distraction Osteogenesis (DO) versus traditional methods in treatment of micrognathia. Methods: During 6 years we had 67 patients with micrognathia. In group A, randomly 35 were treated with traditional methods (Saggital osteotomy and/or bone grafts) and group B 32 cases were treated with Bilateral External Distraction Osteogenesis.Follow up was 36+/- 6 months.X-Ray , CT scan and cast modelling were done for all of the patients. SNA, SNB angles were measured in cephalograms. The patients were examined after one, two, three, six, 12 months for any complications and signs of bone resorption and relapse. Bony and soft tissue advancements were measured and compared with each other.
Results: During 6 years we had 67 patients with class II malocclusion. Mean SNA angle in group A was 80.8 (80-81.5) and 80.9 (80-82) in group B. Mean SNB angle in group A was 77.6 (76.5-78) and 77.4 (76.5-78.5).After treatment mean SNB in group A was 79.1 and the difference was significant comparing to pre-op measurement (P<0.005).Mean SNB in group B after treatment was 79.2 which was significantly different comparing with SNB angle before surgery. The mean SNA in both group were not statistically and significantly different. The mean SNB after surgery in both group were not statistically and significantly different. Mean Mandibular advancement in group A was 11.9 mm (7.5- 18 mm) and group B with DO treatment was12.1 mm (8-19 mm) which was not significantly different . The patient in group A evaluate the surgical results as excellent (60%) and good ( 28.5%). The patient in group B evaluate the results as excellent (78.1%) and good (15.6%).
Conclusion: The Bilateral Distraction Oseogenesis method can bring forwards the retruded mandible effectively and its results has no difference with older methods. It is an effective and reliable procedure for hypoplasia of Mandible and the results are comparable with older methods.
ARTICLE INFO
Article history:
Article history:
Received 12 December 2014
Received in revised form 3 January 2015
Accepted 10 January 2015
Available online 20 January 2015
Micrognathia
Hypoplasia
Mandible
Distraction
Osteogenesis
1. Introduction
Micrognathia is a Greek term and it means small lower jaw.
Mandibular hypoplasia results in a small mandible due to failure of growth and development. On the other hand, Retrognathia is used to describe a jaw that is posteriorly displaced but not necessarily changed in size. And the use of the term mandibular atresia should be discouraged[1-3].
The etiology of Mandibular micrognathia can be classified as congenital, Developmental, or acquired. One of the most frequent causes of congenital mandibular hypoplasia is mal development of the first and second bronchial arches.
This can result in functional disturbances. Deficiencies in the length and width of any part of the lower jaw characterize mandibular hypoplasia. The degree of involvement of each section varies; unilateral and bilateral. When the deformity is bilateral, generalized micrognathia is observed[1,2].
Early consultation with the orthodontist is essential. The surgeon should particularly advise proper timeof orthodontic therapy, since it may result in great complications subsequent to surgical treatment.
Diagnosis and planning of surgical examination of the patient is the important issue. A number of investigations are required to formulate a surgical strategy: photographs, cephalometric and panoramic roentgenograms, CT scans and dental study models. More complicated deformities may call for additional investigations.
One of the traditional method for treatment of micrognathia is “ Sagittal splitting osteotomy of Mandible with or without bone graft.
In this study we wanted to evaluate the results of Bilateral Sagittal splitting technique with Bilateral External Distraction Osteogenesis.
2. Materials and methods
In this study during 6 years we had 67 patients with hypoplasia of Mandible.
2.1. We randomly divided them into two groups.
In group A traditional Sagittal Osteotomy were done. And in group B Bilateral Distraction Osteogenesis were done.
2.2. All pre-op measurements were the same .
X-Ray, CT scan, lab test, Casts, Cephalograms, SNA and SNB angle measurments were done for all of the patients.
2.3. Patients were followed for 36+/- 6 months.
In follow up period X-Ray, CT scan and Cephalograms were taken to campare the results of SNA and SNB angles, Bone advancement , soft tissue advancements and any signs of relapse or bony resorption.
Patients and surgeons evaluate the results as: Excellent, good, moderate and fair.
All of the Data were gathered in a special questionnaire and Data were analyzed with SPSS 16 software.
Pless than 0.05 was considered significant.
3. Results
During 6 years we had 67 patients with micrognathoia with class II malocclusion. They were divided into two groups randomly. In group A 35 patients were treated with Sagittal plitting method and in group B 32 patients were treated with Distraction Osteogenesis.
3.1. Male 51 and female 16 cases.
Mean age was 18.5 years old (from 12-36 years ).
Mean SNA angle in group A was 80.8 degree (80-81.5) and 80.9 (80-82) in group B.
Mean SNB angle in group A was 77.6 degree (76.5-78) and 77.4 (76.5-78.5) .After treatment mean SNB in group A was 79.1 and its difference was significant comparing to pre-op measurement (P<0.005).
Mean SNB in group B after treatment was 79.2 which was significantly different comparing with SNB angle before surgery.
The mean SNA in both group before surgery were not statistically and significantly different.
Mean SNB after surgery in both groups were not different significantly. Table 1 Mean Mandibular advancement in group A was 11.9 mm (7.5-18 mm) and group B with DO treatment was 12.1 mm (8-19 mm) which was not significantly different.
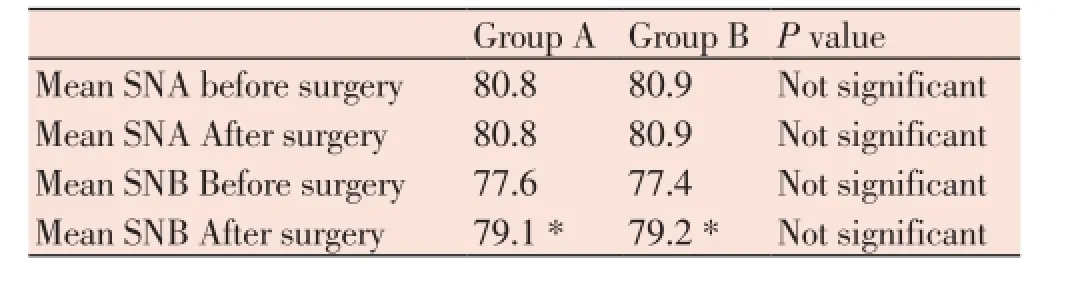
Table 1. Comparison between angles before and after surgery and between the two groups.
CT scan after surgery showed no resorption in both groups. Mean Relapse was 2.5 mm in group A and 2.1 mm in group B which was not significantly different.
The patient in group A evaluate the surgical results as excellent (60%) and good (28.5%).
The patient in group B evaluate the results as excellent (78.1%) and good (15.6%). Picture 1-9.
The surgeon evaluate the results in group A as excellent 68.5% and good 25.7%.
And in group B as excellent 78.1% and good 18.7%.
4. Discussion
Hypoplasia of Mandible has been recognized from a long time ago and several techniques for its reconstruction have been introduced in the literature[1-3].
Some of them are syndromic such as; Pierre Robin sequence or Treacher Collins syndrome, craniofacial microsomia or Goldenhar syndrome, Nager syndrome and narrow mandible with anterior dental crowding[4-7].
Some of the methods are: Body Osteotomy , Elongation Osteotomies of Body of Mandible, C shape Osteotomy,L shape Osteotomy, Horizontal osteotomies through the ramus, The oblique osteotomy, Segmental intredental Osteotomy, Kolle’s Operation, Sagittal Osteotomy and finally and recently Distraction osteotomy[1,8].
Distraction osteogenesis or callostasis is a technique of new bone formation by gradual advancement of osteotomized bony parts. The method was first developed for thigh and leg lengthening but recently this process has been widely used the cranio-maxillofacial bones deficiencies.
The process include unlimited bone lengthening and reconstruction of segmental defects with distraction of softtissue and producing enough coverage for the newly formed bones.
Several designs of extra-oral and intra-oral distraction devices were introduces to fix different areas of craniofacial bone deformities. However intraoral distractors is claimed to have several advantages including minimal scarring and being less annoying to the patients specially younger ones. Clinical cases using distraction osteogenesis as an alternative method to traditional surgical procedures for maxillo-mandibular lengthening and reconstruction of alveolar segmental defects after tumour resection before implant installation[9-11].
There are several reports about efficacy of ramus osteotomy and its lack of sensory nerve impairment. But it needs a big and long operation and in most of all bone grafts which need another operative site for bone harvest .
Some other authors prefer Sagittal ramus Osteotomy with immediate advancement , but still this technique sometimes needs bone graft and its complications[12].
Distraction osteogenesis should not be seen as a replacement for conventional osteotomies, but as a valuable alternative treatment[13]. Newly Distraction osteogenesis or callotesis whether internal or external is a good option with several advantages, such as gradual extention of tissues , better soft tissue expansion and results[14], fewer sensory nerve impairment, no need for bone grafts, fast result and fast gaining conclusion ( in less than 25 days you can stop the distraction and the patients can see the results) , better quality of Mandible, Better ways for adjustment of Mandible to Maxilla, better Occlusion, several option to Distract both side of Mandible with two devices and with different velocity ( to treat unbalance of both side of Mandible in asymmetric deformities of mandible) and so on[15]. Advantages of distraction osteogenesis over conventional traditional osteotomies which are often used are application at a younger age, lower risk of nerve damage, the advancement of the jaw or parts of the jaw over a greater distance, better stability of the treatment result, no need for bridging with bone grafts, lower surgical risk and shorter surgery time so lesser complications[13].
This device can be used in even growing ages so there is no need to wait for completion of bony growth in the face . and in earlier ages the patients can be treated by Distraction[16-18].
Anyhow Distraction Osteogenesis continues to grow as a leading method of surgical correction for a variety of craniofacial defects. Current research shows significant very good results of its application[9].
There different types of Distractors , some are External , some Internal and some are semi-internal exist.
The so-called semiburied device reduces scarring and has the mechanical advantages of being applied directly to the bone, lesser chance of dislodgment, and more favorable for a vertical vector. However, its use requires more bone reserve and it has sadly requiring a second operation for removal.
Therefore semiburied distraction is safe, reliable, and indicated for lengthening of the hypoplastic mandible if adequate bone stock is available for its attachment[10].
The angle of DO device is very important and needs careful attention. A strong correlation was noted between the vector of distraction and rotation of the symphyseal plane, movement of the mandibular symphysis, and change in interocclusal angle. A horizontal vector of distraction resulted in minimal counterclockwise rotation of the symphyseal plane, greater downward Bvertical translation of the mandibular symphysis, and minimal closure of an anterior open bite. In contrast, a vertical vector resulted in greater counterclockwise rotation of the symphyseal plane, greater horizontal projection of the mandibular symphysis, and greater closure of an anterior open bite[19].
Mandibular distraction osteogenesis was reported to improve facial asymmetry and retrognathia (50.1 percent), correct the slanted lip commissure (24.7 percent), and improve or level the mandibular occlusal plane (11.1 percent) in unilateral asymmetry cases, whereas bilateral mandibular distraction osteogenesis has benefit in preventing tracheostomies for 91.3 percent of neonates or infants with respiratory distress, and in relieving symptoms of obstructive sleep apnea for 97.0 percent of children and 100 percent of adult patients[2].
This device has also been used for mandibular widening in the transverse plane and lengthening of the vertical mandibular ramus. It has also become shown that distraction osteogenesis is a very useful alternative treatment for conventional osteotomy for the lengthening of the horizontal mandibular ramus for retrognathia[13].
The bone after DO is to a great scale stable and has ability to grow. When bony structures and growth centers for the mandibular forward and downward displacement are rudimentary or missing in syndromic patients, DO can not’correct’ the condition and post-distraction growth will be minimal.But non-syndromic patients have a better potential to respond favourably to DO and jhave better growth[16].
Severally it is reported that distraction osteogenesis have obviated the need for tracheostomy in most newborns with micrognathia and severe airway obstruction[3].
There are some complications that are reported in the literature such as: Inferior alveolar nerve (IAN) neurosensory disturbances, minor infection, device Failure or dislodgement, anterior open bite, permanent dental damage, and skeletal relapse . and some others reported that complications of MDO include relapse (64.8% incidence), tooth injury (22.5%), hypertrophic scarring (15.6%), nerve injury (11.4%), infection (9.5%), inappropriate distraction vector (8.8%), device failure (7.9%), fusion error (2.4%), and temporomandibular joint injury (0.7%)[15].
Overall complications that resolved spontaneously were seen in 11.0%, medically or technically manageable complications, without hospitalization, were seen in 10.8%, and permanent complications were seen in 9.6%[12].
Most of these complications are minimal and can be treated rapidly and easily. In our study we had not any permanent Inferior alveolar nerve sensory impairment or pinsite infection .
Relaspe was seen in 9 (13.4%) of our patients, 5 in group A and 4 in group B . The mean relapse were 2.5 mm in group A and 2.1 mm in group B . the difference was not significant . Despite numerous papers for many advantages of distraction osteogenesis, however, scientific evidence is still lacking.[13]and So far, there has been no evidencebased review of mandibular distraction osteogenesis for mandibular lengthening[2] and clinical trials are required to assess the long-term stability and to compare the treatment with conventional treatment methods[2]. Therefore we have conducted the present study to evaluate the results of the two methods in treatment of Mandibular hypoplasia .
Our results shown that Distraction osteogenesis can advance the deficient Mandible and new bone can be produced. The occlusional plane can be treated easily and the advancement are comparable to the sagittal splitting method. SNB angle improve prominently and the difference with pre-op measurments is highly significant. And the difference with the convetional method is not significant.
So it is concluded that the DO has the same results as the conventional methods and it has not the disadvantages of them.
5. Conclusioin
With our evidences it is shown that the external Distraction osteogenesis is the method of choice for treatment of Mandibular hypoplasia . And the results are comparable with the traditional methods
Complication are much less than traditional methods. And relapse of both methods are the same.
Conflict of interest statement
The authors report no conflict of interest.
Aknowledgement
There are no conflict of interest among the authors. There is nothing to declare .
[1] Ow A, Cheung LK. Skeletal stability and complications of bilateral sagittal split osteotomies and mandibular distraction osteogenesis: an evidence-based review. J Oral Maxillofac Surg. 2009; 67(11): 2344-53.
[2] Ow AT, Cheung LK. Meta-analysis of mandibular distraction osteogenesis: clinical applications and functional outcomes. Plast Reconstr Surg 2008; 121(3): 54e-69e.
[3] Fritz MA, Sidman JD. Distraction osteogenesis of the mandible. Curr Opin Otolaryngol Head Neck Surg 2004; 12(6): 513-8.
[4] Rachmiel A, Emodi O, Rachmiel D, Aizenbud D. Internal mandibular distraction to relieve airway obstruction in children with severe micrognathia. Int J Oral Maxillofac Surg 2014; 43(10): 1176-81.
[5] Lam DJ, Tabangin ME, Shikary TA, Uribe-Rivera A, Meinzen-Derr JK, de Alarcon A, Billmire DA, Gordon CB. Outcomes of mandibular distraction osteogenesis in the treatment of severe micrognathia.JAMA Otolaryngol Head Neck Surg 2014; 140(4): 338-45.
[6] Hong P, McNeil M, Kearns DB, Magit AE. Mandibular distraction osteogenesis in children with Pierre Robin sequence: impact on health-related quality of life. Int J Pediatr Otorhinolaryngol 2012; 76(8): 1159-63.
[7] Hong P, Bezuhly M. Mandibular distraction osteogenesis in the micrognathic neonate: a review for neonatologists and pediatricians. Pediatr Neonatol 2013; 54(3): 153-60.
[8] Sidman J, Tatum SA. Distraction osteogenesis. Facial Plast Surg Clin North Am 2014; 22(1): 139-46.
[9] Saman M, Abramowitz JM, Buchbinder D. Mandibular osteotomies and distraction osteogenesis: evolution and current advances. JAMA Facial Plast Surg 2013; 15(3): 167-73.
[10] Davidson EH, Brown D, Shetye PR, Greig AV, Grayson BH, Warren SM, et al. The evolution of mandibular distraction: device selection. Plast Reconstr Surg 2010; 126(6): 2061-70. doi: 10.1097/PRS.0b013e3181f526d9.
[11] Jović N. Distraction osteogenesis in the treatment of facial and mandibular deformities. Vojnosanit Pregl 2006; 63(3): 297-304.
[12] Verlinden CR, van de Vijfeijken SE, Tuinzing DB, Jansma EP, Becking AG, Swennen GR. Complications of mandibular distraction osteogenesis for developmental deformities: a systematic review of the literature. Int J Oral Maxillofac Surg 2014. pii: S0901-5027(14)00340-3.
[13] Jansma J, Becking AG. Distraction osteogenesis and orofacial anomalies. Ned Tijdschr Tandheelkd 2008; 115(6): 324-30.
[14] Fu XH, Chen J, Ping FY, Yan FG, Shan YD. Soft tissue profile changes in micrognathia after distraction osteogenesis. Zhonghua Zheng Xing Wai Ke Za Zhi 2008; 24(4): 271-4.
[15] Master DL, Hanson PR, Gosain AK. Complications of mandibular distraction osteogenesis. J Craniofac Surg 2010; 21(5): 1565-70.
[16] Peltomäki T. Stability, adaptation and growth following distraction osteogenesis in the craniofacial region. Orthod Craniofac Res 2009; 12(3): 187-94.
[17] Kolstad CK, Senders CW, Rubinstein BK, Tollefson TT. Mandibular distraction osteogenesis: at what age to proceed.;Int J Pediatr Otorhinolaryngol 2011; 75(11): 1380-4.
[18] Diner PA, Tomat C, Hamou C, Vazquez MP, Picard A. Maxillary and mandibular distraction osteogenesis in growing patients: lessons learned after 14 years and update on indications. Ann R Australas Coll Dent Surg 2008; 19: 116-22.
[19] Vendittelli BL, Dec W, Warren SM, Garfinkle JS, Grayson BH, McCarthy JG. The importance of vector selection in preoperative planning of bilateral mandibular distraction. Plast Reconstr Surg 2008; 122(4): 1144-53.
ment heading
10.1016/S2221-6189(14)60064-0
*Corresponding author: Hamid Karimi M.D. P.O.Box : 19395-4949, Tehran , Iran.
Tel : + 98 912 3179089
Fax: + 98 21 88770048
E-mail : hamidkarimi1381@yahoo.com
karimihamid11@gmail.com
杂志排行
Journal of Acute Disease的其它文章
- Acute and sub-acute toxicity study of Clerodendrum inerme, Jasminum mesnyi Hance and Callistemon citrinus
- Time-critical AMI Detection: A novel and fast technique using the 12-lead ECG
- Epidemiological survey on scorpionism in Gotvand County, Southwestern Iran: an analysis of 1 067 patients
- The acute effect of the antioxidant drug “U-74389G” on red blood cells levels during hypoxia reoxygenation injury in rats
- Successful treatment of lower urinary tract obstruction with peritonealamniotic and vesicoamniotic shunting
- Simvastatin-induced Toxic Epidermal Necrolysis
