子宫动脉血流监测高危妊娠的研究进展
2014-02-14宋双李辉
宋双 李辉
(中国医科大学附属盛京医院妇产科,辽宁沈阳 110004)
子宫动脉血流监测高危妊娠的研究进展
宋双 李辉*
(中国医科大学附属盛京医院妇产科,辽宁沈阳 110004)
母胎间的营养物质和代谢产物的交换是维持正常妊娠必须的条件之一,这一过程的完成,需要滋养细胞在妊娠早期成功侵袭子宫螺旋动脉壁,破坏其肌性成分,将管腔狭细和高血管阻力的子宫螺旋动脉转化为管腔宽大、低血管阻力的子宫胎盘循环动脉(uteroplacental artery),同时逐渐深入胎盘向更低压力的胎盘绒毛间隙供血,在绒毛间隙完成母体与胎儿间氧和营养物质的交换。如果子宫螺旋动脉的这种妊娠生理性改变不足,便会导致子宫胎盘循环阻力增高,进一步导致子痫前期、胎儿宫内发育受限等病理妊娠发生。因此监测子宫动脉的血管阻力对早期发现高危妊娠,并为进一步临床管理减少母儿不良预后提供帮助。
1 子宫动脉血流测定
大约有100条的子宫螺旋动脉发展成为子宫胎盘循环动脉,当子宫胎盘循环动脉血管阻力升高时,其上游的子宫动脉阻力也会增加,因此,应用超声评价其上游的子宫动脉阻力即可以用来间接评价子宫胎盘循环阻力,这一点已通过“子宫动脉血管阻力增高与滋养细胞侵袭后子宫螺旋动脉的生理改变不足的病理组织检查结果相一致”的研究成果所证实[1-3]。
将超声探头置于孕妇的腹股沟上方,彩色超声多普勒血流成像图需同时显示子宫动脉和髂外动脉,在子宫动脉和髂外动脉相交处附近获取子宫动脉的血流速度频谱图(见图1),取样角度小于25°。评价子宫动脉血管阻力的临床常用指标有搏动指数(pulsatility index,PI)、阻力指数(resistance index,RI)和子宫动脉血流频谱是否出现舒张期切迹(见图2、3)。当子宫胎盘血流阻力升高时,会表现为子宫动脉的PI、RI值升高,子宫血流频谱出现舒张期切迹。在正常妊娠的情况下,子宫动脉的血流阻力会随妊娠进展逐渐降低,而且子宫动脉血流频谱出现舒张期切迹的发生率也明显降低,当子宫动脉的血流阻力明显增高和舒张期切迹持续存在时,则提示子宫胎盘循环血量不足,常常会导致妊娠合并症和不良围产儿预后[4]。
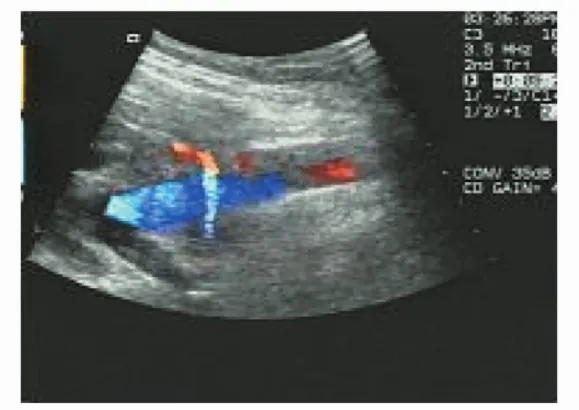
图1 子宫动脉和髂外动脉相交处附近获取子宫动脉的血流

图2 妊娠早期正常子宫动脉的流速波形

图3 妊娠早期异常子宫动脉波形(血流阻力增高且可见舒张早期切迹)
2 子宫动脉血流监测的临床应用
在早孕期和中孕期监测子宫动脉血管阻力对预测子痫前期、胎儿宫内生长受限(IUGR)、胎盘早剥和死产等有较大的临床应用价值[5-7],在晚孕期监测子宫动脉血管阻力用来监测子痫前期、胎儿宫内生长受限等高危胎儿,协助判断因胎盘供血供氧不足导致的胎儿慢性宫内缺氧状态和不良围产儿预后有重要价值[8]。
2.1 子宫动脉血流预测子痫前期和IUGR 子痫前期和IUGR会导致较高的母儿发病率和死亡率,早期筛查及严密监护子痫前期和IUGR可明显改善母儿预后,因此,很多学者都一直在努力去寻求预测子痫前期的有效方法,但至今尚未发现高敏感的预测方法。大量研究表明,妊娠早期母体螺旋动脉的滋养细胞侵袭失败导致子宫胎盘循环阻力增高是子痫前期和IUGR的发病主要原因,因此,应用子宫动脉的血流阻力来预测子痫前期和IUGR便成为研究热点。但因为应用的研究对象不同、孕周不同、标准切割值不同、疾病的定义不同导致预测的敏感性差异较大,在临床上应用该技术的预测敏感性因不理想性且假阳性率高限制了其应用[9]。Gomez O等[4]在妊娠11~14周对1091例孕妇进行子宫动脉血流检测,其检查结果发现随着孕周进展,子宫动脉的PI逐渐下降,而且双侧子宫动脉血流频谱切迹的出现率也逐渐下降,详见表1。应用子宫动脉的搏动指数(pusatility index,PI)高于第95百分位数为切割值,用来预测妊娠合并症(包括子痫前期、IUGR、胎盘早剥)的敏感性为23.9%。另外,由于仅40%左右的孕妇会出现双侧子宫动脉血流频谱切迹,因此应用子宫动脉血流频谱舒张早期切迹预测子痫前期的价值更为有限。Martin AM等[10-12]以3195例为研究对象,其研究结果显示以子宫动脉PI值2.35(第95百分位数)为切割值,用来预测子痫前期的敏感性为27%,IUGR的敏感性为11.7%,用来预测子痫前期合并IUGR且需32周前终止妊娠的敏感性为60%。妊娠中期应用子宫动脉预测子痫前期和IUGR的敏感性明显增加,英国一项多中心研究(7851例正常孕妇,孕周22~24周)结果显示以子宫动脉PI 1.65(第95百分位数)为切割值,用来预测子痫前期的敏感性为41%,IUGR的敏感性为16%,子痫前期并发IUGR的敏感性为69%。研究结果也进一步显示应用子宫动脉PI预测子痫前期和IURG明显优于子宫动脉血流频谱舒张早期切迹[13]。然而,由于在低危人群应用子宫动脉预测子痫前期和IUGR的敏感性较低,Cochrane系统评价结论显示在低危孕妇中妊娠中期进行高血压疾病的筛查并没有明显的优点[14]。
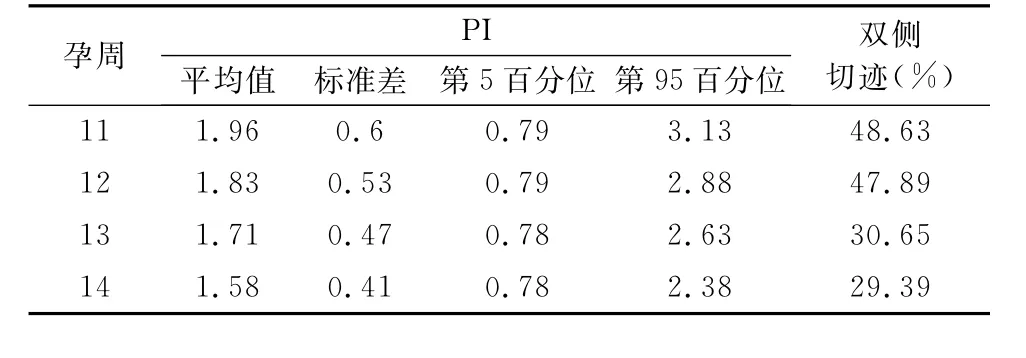
表1 妊娠11~14周子宫动脉血流检测
2.2 孕晚期应用子宫动脉血流监测高危妊娠 在孕晚期的子宫动脉血流检测主要是用来评价高危妊娠,主要有妊娠期高血压疾病、IUGR等,在子痫前期或IUGR的患者中,子宫动脉血流阻力异常增高与围产期不良预后如低脐动脉血气p H值、低Apgar评分、早产、小于胎龄儿等明显相关[15-18]。Kafkasli等[19]的研究结果显示子痫前期的患者当子宫动脉血流表现为异常升高时,围产儿不良预后的发生率要明显高于子宫动脉血流正常组。在低危妊娠中的应用价值尚存在一定争议,有学者认为在低危妊娠中妊娠晚期出现的子宫动脉血流阻力增高与不良围产儿预后也明显相关[17],然而多数学者认为子宫动脉血流在低危妊娠中的应用价值有限[20]。应用子宫动脉进行高危妊娠的监测,因为存在左右两侧的子宫动脉,而且评价指标也为PI和子宫动脉舒张早期切迹,因此在临床应用存在一定复杂性。Gudmundsson等[21]将子宫动脉血流阻力指标等进行系统评分(uterine artery scores,UAS),UAS代表的子宫胎盘血流,即胎盘母体面血流评价;同时结合脐动脉血流分级(blood flow class,BFC),BFC代表的是胎儿胎盘血流评价,将UAS与BFC整合最终提出胎盘血流评分(placental socre,PLS)用来总体评价胎盘血管阻力(PLS=UAS+BFC),具体评分方法见表2,研究表明应用PLS评价高危妊娠胎儿不良预后明显优于UAS和BFC[21]。应用PLS全面评价胎盘循环,科学合理准确判断胎儿预后。也有学者应用胎儿大脑中动脉(Middle cerebral artery)PI与子宫动脉PI比值预测子痫前期胎儿的预后,结果显示该比值小于1.08的子痫前期患者围产儿发病率和死亡率明显增高[22]。

表2 子宫动脉血流阻力评分系统(UAS),脐动脉血流评分系统分级(BFC)
综上所述,子宫动脉血流在孕早期和中期尽管在低危妊娠中用来预测子痫前期和IUGR的价值有限,但对胎盘功能受损导致的相关疾病这一高危群体的监护价值明显,结合应用子宫动脉血流和胎儿循环脐血流、脑血流等来综合评价胎儿-胎盘循环状态,临床正确干预,对减少不良围产儿预后有重要价值。
[1]Guzin K,Tomruk S,Tuncay YA,et al.The relation of increased uterine artery blood flow resistance and impaired trophoblast invasion in pre-eclamptic pregnancies[J].Arch Gynecol Obstet,2005,272:283-288.
[2]Sagol S,Ozkinay E,Oztekin K,et al.The comparison of uterine artery Doppler velocimetry with the histopathology of the placental bed[J].Aust NZ J Obstet Gynecol,1999,39:324-329.
[3]Olofsson P,Laurini RN,Marsal K.A high uterine artery pulsatility index re flects a defective development of placental bed spiral arteries in pregnancies complicated by hypertension and fetal growth retardation[J].Eur J Obstet Gynecol Reprod Biol,1993,49:161-168.
[4]Gomez O,Figueras F,Martinez JM,et al.Sequential changes in uterine artery blood flow pattern between the first and second trimesters of gestation in relation to pregnancy outcome[J].Ultrasound Obstet Gynecol,2006,28:802-808.
[5]Martin AM,Bindra R,Curcio P,et al.Screening for pre-eclampsia and fetal growth restriction by uterine artery Doppler at 11-14 weeks of gestation[J].Ultrasound Obstet Gynecol,2001,18:583-586.
[6]Harrington K,Cooper D,Lees C,et al.Doppler ultrasound of the uterine arteries:the importance of bilateral notching in the prediction of pre-eclampsia,placen-tal abruption or delivery of a small-for-gestational-age baby[J].Ultrasound Obstet Gynecol,1996,7:182-188.
[7]Becker R,Vonk R,Vollert W,et al.Doppler sonogra-phy of uterine arteries at 20-23 weeks:risk assessment of adverse pregnancy outcome by quantification of impedance and notch[J].J Perinat Med,2002,30:388-394.
[8]Maryam Afrakhteh,Aida Moeini,Morteza Sanei Taheri,et al.Uterine Doppler velocimetry of the uterine arteries in the second and third trimesters for the prediction of gestational outcome[J].Rev Bras Ginecol Obstet,2014,36(1):35-39.
[9]Llurba E,Carreras E,Gratacos E,et al.Maternal history and uterine artery Doppler in the assessment of risk for development of early-and late-onset preeclampsia and intrauterine growth restriction[J].Obstet Gynecol Int,2009,2009:275613.
[10]Gomez O,Martinez JM,Figueras F,et al.Uterine artery Doppler at 11-14 weeks of gestation to screen for hypertensive disorders and associated complications in an unselected population[J].Ultrasound Obstet Gynecol,2005,26:490-494.
[11]Martin AM,Bindra R,Curcio P,et al.Screening for pre-eclampsia and fetal growth restriction by uterine artery Doppler at 11-14 weeks of gestation[J].Ultrasound Obstet Gynecol,2001,18:583-586.
[12]Savasan ZA,Goncalves LF,Bahado-Singh RO.Second-and third-trimester biochemical and ultrasound markers predictive of ischemic placental disease[J].Semin Perinatol,2014,38:167-176.
[13]Papageorghiou AT,Yu CK,Bindra R,et al.Multicenter screening for pre-eclampsia and fetal growth restriction by transvaginal uterine artery Doppler at 23 weeks of gestation[J].Ultrasound Obstet Gynecol,2001,18:441-449.
[14]Stampalija T,Gyte GM,Alfi revic Z.Utero-placental Doppler ultrasound for improving pregnancy outcome[J].Cochrane Database Syst Rev,2010,9.CD008363.
[15]Llurba E,Carreras E,Gratacos E,et al.Maternal history and uterine artery Doppler in the assessment of risk for development of early-and late-onset preeclampsia and intrauterine growth restriction[J].Obstet Gynecol Int,2009,2009:275613.
[16]Hwang HS,Kim YH,Kwon JY,et al.Uterine and umbilical artery Doppler velocimetry as a predictor for adverse pregnancy outcomes in pregnant women with anemia[J].J Perinat Med,2010,38:467-471.
[17]Shwarzman P,Waintraub AY,Frieger M,et al.Third-trimester abnormal uterine artery doppler findings are associated with adverse pregnancy outcomes[J].J Ultrasound Med,2013,32(12):2107-2113.
[18]Li H,Gudnason H,Olofsson P,et al.Increased uterine artery vascular impedance is related to adverse outcome of pregnancy but is present in only one-third of late third-trimester pre-eclamptic women[J].Ultrasound Obstet Gynecol,2005,of neonatal outcome in patient with preeclampsia and gestational hypertension[J].J Prenat Med,2010,4(2):17-21.
[44]Yalti S,Oral O,Gurbuz B,et al.Ratio of middle cerebral to umbilical artery blood velocity in preeclamptic&hypertensive women in the prediction of poor perinatal outcome[J].Indian J Med Res,2004,120(1):44-50.
[45]Eser A,Zulfikaroglu E,Eserdag S,et al.Predictive value of middle cerebral artery to uterine artery pulsatility index ratio in preeclampsia[J].Arch Gynecol Obstet,2011,284(2):307-311.
[46]Mari G.Middle cerebral artery peak systolic velocity for the diagnosis of fetal anemia:the untold story[J].Ultrasound Obstet Gynecol,2005,25(4):323-330.
[47]Klaritsch P,Deprest J,Van Mieghem T,et al.Reference ranges for middle cerebral artery peak systolic velocity in monochorionic diamniotic twins:a longitudinal study[J].Ultrasound Obstet Gynecol,2009,34(2):149-154.
[48]van den Broek AJ,Kok JH,Houtzager BA,et al.Behavioural problems at the age of eleven years in preterm-born children with or without fetal brain sparing:a prospective cohort study[J].Early Hum Dev,2010,86(6):379-384.25(5):459-463.
编辑:刘勇
[19]KafkaslıA,Türkçüoglu I,Turhan U.Maternal,Fetal and perinatal characteristics of preeclampsia cases with and without abnormalities in uterine artery Doppler indexes[J].J Matern Fetal Neonatal Med,2013,26(9):936-940.
[20]Bolz N,Kalache KD,Proquitte H,et al.Value of Doppler sonography near term:can umbilical and uterine artery indices in low-risk pregnancies predict perinatal outcome?[J].J Perinat Med,2013,41(2):165-170.
[21]Gudmundsson S,Korszun P,Olofsson P,et al.A new score indicating placental vascular resistance[J].Acta Obstet Gynecol Scand,2003,82:807-812.
[22]Eser A,Zulfıkaroglu E,Eserdag S.Predictive value of middle cerebral artery to uterine artery pulsatility index ratio in preeclampsia[J].Arch Gynecol Obstet,2011,284(2):307-311.
(收稿日期:2014-08-15)
编辑:宋文颖
R445.1
A
10.13470/j.cnki.cjpd.2014.03.003
2014-08-11)
*通讯作者:李辉,E-mail:ligelihui@yahoo.com.cn