Clinical Study on Acupoint Injection for Primary Osteoporosis
2013-07-18XiaShushuQuQunwei
Xia Shu-shu, Qu Qun-wei
1 Hospital of Hubei University, Wuhan 430062, China
2 Red Cross Hospital of Shiyan City, Hubei Province, Shiyan 442000, China
Clinical Study on Acupoint Injection for Primary Osteoporosis
Xia Shu-shu1, Qu Qun-wei2
1 Hospital of Hubei University, Wuhan 430062, China
2 Red Cross Hospital of Shiyan City, Hubei Province, Shiyan 442000, China
Objective: To observe the therapeutic efficacy of acupoint injection in treating primary osteoporosis.
Methods: A hundred and fourteen eligible subjects were randomized at 2:1 into two groups. Seventy-six subjects in the observation group were intervened by acupoint injection, and 38 subjects in the control group were intervened by oral medication. Symptom and signs scores were observed before and after treatment. A two-year follow-up study was conducted to compare the long-term therapeutic efficacy between the two groups.
Results: The recovery and markedly effective rate was 68.4% in the observation group versus 47.4% in the control group, and the difference was statistically significant (P<0.05). During the 2-year follow up study, 5 subjects in the observation group and 8 in the control group had new fracture, occupying 6.6% and 21.1% respectively, and the difference was statistically significant (P<0.05).
Conclusion: In treating primary osteoporosis, acupoint injection has better short and long term therapeutic efficacies compared to oral medication, and it’s convenient with high security evaluation.
Acupoint Therapy; Hydro-acupuncture; Osteoporosis; Points, Back-Shu; Acupuncture Therapy
Osteoporosis is a harmful and intractable senile disease with high incidence. It can be present without any symptoms at the early stage, and only be aware when pain or fracture happens. It severely damages the general health of the middle-aged and senile people. Currently, there are many preventive and treatment medicines and methods. We have majorly applied acupoint injection to the Back-Shu acupoints to treat 76 patients with primary osteoporosis since 2009. The report is now given as follows.
1 Clinical Materials
1.1 Diagnostic criteria
The diagnostic criteria were referring to theDiagnosis and Treatment Guideline on Primary Osteoporosis(2011)[1]and theGuiding Principles for Clinical Study of New Chinese Medicines[2]. General fatigue and deteriorating lumbar and back pain are the major symptoms, and minor injury may cause fracture; kyphotic deformity of spine is often present; X-ray reveals decreased bone density, especially in spine, hip, and the upper part of femur, as well as sideways curve of the spine, and wider intervertebral space; bone density is measured as 2.5 standard deviation or more below the mean peak bone mass.
1.2 Inclusion criteria
In conformity to the above diagnostic criteria; postmenopausal females and male subjects over 50 years old; having signed informed consent form.
1.3 Exclusion criteria
Being against the above diagnostic criteria; secondary osteoporosis; long-term use of other anti-osteoporosis medications which cannot be terminated at once; coexisting diseases of cardiocerebrovascular, liver, kidney, and hematopoietic systems; psychological diseases; unwilling to receive the treatment adopted in this study.
1.4 General data
Totally 114 subjects were enrolled. They were clinically manifested by various degrees of lumbar and back pain, with tender or percussion pain of spinous process, lumbar stiffness, and limited bending scope of waist. Of them, 28 had numbness of lower limbs, 40 had obvious loss of height and hunched back, 88 had hyperosteogeny of thoracic and lumbar vertebrae, and 66 had spinal compression fracture of various degrees (28 with fracture of one vertebra, 17 with fracture of two vertebrae, 14 with fracture of 4-5 vertebrae, and 3 with fracture of over 5 vertebrae).
All subjects were divided into 2 groups at 2:1 according to their visiting sequence. There were no statistically significant differences between the two groups in comparing gender, age, disease duration, and severity (P>0.05), indicating the comparability (table 1).
The subjects all completed the study. The clinical process is shown in Fig.1.
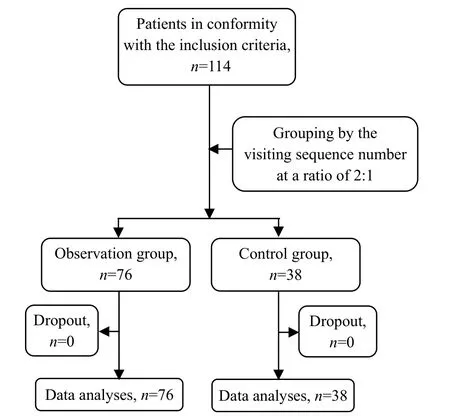
Fig.1 Clinical management flow chart
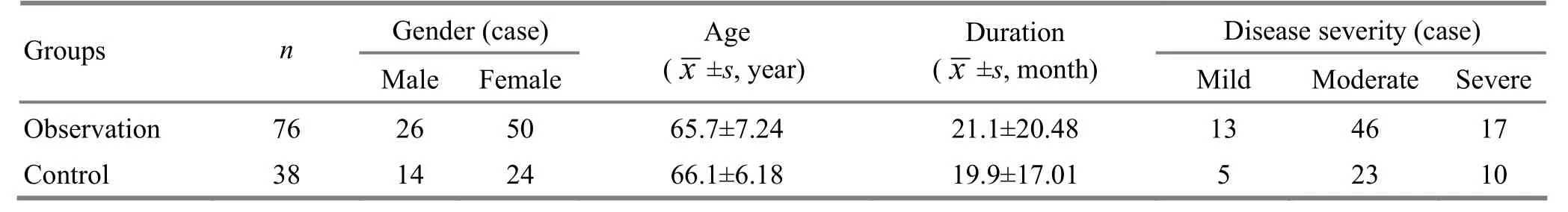
Table 1. Comparison of general data between the two groups
2 Treatment Methods
2.1 Observation group
Major acupoints: Ganshu (BL 18), Pishu (BL 20). Weishu (BL 21), and Shenshu (BL 23).
Adjunct acupoints: Ashi points beside vertebrae.
Operation: The acupoints were used alternately and four acupoints were selected each time. After sterilization, a 10 mL syringe was used to draw CompoundDang Gui(Radix Angelicae Sinensis) Injection 2 mL, Ossotide Injection 2 mL, and Vitamin D2and Calcium Colloid Injection 2 mL. When the fluids were fully mixed, the needle was inserted swiftly into the point obliquely towards the spine at an angle of 30° till depth of 2-3 cm. The needle was lifted and thrusted to produce needling sensations, and 1.5 mL fluid was injected for each point if there was no withdrawal blood. Ten treatments were considered as a treatment course. During the first course, the treatment was given once per day, one-week interval between every two courses, and the treatment was given once two days afterwards. Three treatment courses were given at most.
2.2 Control group
The control group received oral medications: Compound Calcium Amino Acid Chelate Capsules, 1-2 capsules each time, once per day;Xian Ling Gu BaoCapsules, 3 capsules each time, twice per day. Thirty-day treatment was considered as a course, 1-week interval between every two courses, and at most 2 treatment courses were given.
3 Observation on Therapeutic Effects
3.1 Criteria of therapeutic effects
According to the grading scale of osteoporosis symptoms of theGuiding Principles for Clinical Study of New Chinese Medicines[2], 6 symptoms, includinglumbago and backache, soreness and weakness of waist and knees, lower limb pain, lower limb flaccidity, difficulty walking, and dizziness, were graded as normal, mild, moderate, and severe levels, and were respectively scored 0, 1, 2, and 3. The subjects were scored before and after treatment by fixed staff who didn’t participate in treatment and grouping, and the global symptom and signs scores would be calculated based on the component scores.
The therapeutic efficacy was evaluated according to the reduction rate of symptoms and signs scores, which was calculated with the global symptom and signs scores.
Reduction rate of symptom and signs scores = (Pretreatment score-Post-treatment score) ÷ Pretreatment score × 100%.
Clinical recovery: Clinical symptoms and signs of traditional Chinese medicine (TCM) are gone or substantially gone, and the reduction rate of symptom and signs scores ≥95%.
Marked effect: The TCM symptoms and signs have marked improvement, and the reduction rate of symptom and signs scores ≥70%, but <95%.
Effect: The TCM symptoms and signs are improved, and the reduction rate of symptom and signs scores≥30%, but <70%.
Invalid: The TCM symptoms and signs are not improved, or even deteriorated, and the reduction rate of symptom and signs scores <30%.
All patients were interviewed via telephone or face to face during the following 2 years, to observe the frequency of fracture and refracture.
3.2 Statistical analysis
All data were processed by using DPS 9.5 statistical software. Numeration data were dealt with Chi-square test; measurement data were expressed by () and dealt with Fisher’s least significant difference (LSD)t-test.
3.3 Treatment results
3.3.1 Comparison of therapeutic effects
Recovery and marked effect rate = (Number of clinical recovery case + Number of marked effect case) ÷ Total case number of the group × 100%.
There was a significant difference between the two groups in comparing the recovery and marked effect rate (P<0.05), indicating that the observation group had a better therapeutic efficacy than the control group (table 2).
3.3.2 Comparison of follow-up study results
Regarding the fracture case during the two-year follow-up study, there were 5 cases in the observation group, occupying 6.6%, and 8 cases in the control group, occupying 21.1%, and the difference was statistically significant (P<0.05). It indicated that the observation group had a better long-term therapeutic efficacy than the control group.
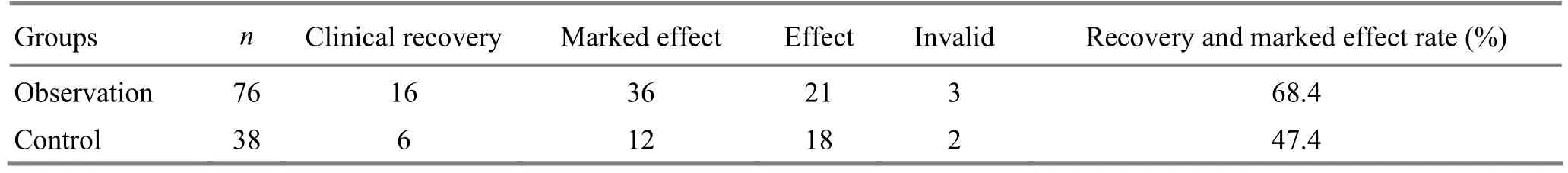
Table 2. Comparison of therapeutic effects (case)
4 Discussion
Primary osteoporosis is majorly manifested by pain, loss of height, and spine deformity such as hunched back, and fracture. It is classified into type Ⅰ (postmenopausal osteoporosis) and type Ⅱ (elderly osteoporosis), and idiopathic osteoporosis[1]. Its major pathogenesis should be imbalance of bone metabolism and decrease of bone mass and calcium. TCM theory holds that the kidney is the congenital source, governing bone and responsible for production of bone marrow. Deficiency of kidney-qi will lead to shortage of source to transform into marrow, malnutrition and fragility of bone, and subsequent lumbago and backache. The liver and kidney share the same source. Hence, kidney-yin deficiency can lead to liver-yin deficiency, and vice versa. They can both cause depletion of marrow and weakness of bone. The spleen is the post-natal source, governing limbs and muscles. When the spleen is too weak to transport and transform, the congenital essential qi cannot be supplemented, and depletion of essence and marrow and fragility of bones will gradually develop. Long-term deficiency of liver, spleen, and kidney, and dysfunction of liver in dispersing and spleen in transporting and transforming may cause stagnation of qi and blood. When kidney-yang is too deficient or primordial qi is too weak to warm and nourish vessels or circulate blood, there will appear blood stagnation, blockage of meridians and collaterals, dysfunction of qi-blood circulation, and poor nutrition of limbs and muscles. In a word, the key pathogenesis and etiology of the disease should be kidney deficiency, but it also involves deficiency of liver-yin, spleen-qi, and qi and blood, as well as the excessive symptoms such as blood stagnation. It will finally lead to depletion of marrow and flaccidity of tendons, and osteoporosis will then develop.
The therapeutic efficacy of acupuncture-moxibustion for osteoporosis is confirmed[3-7]. Shenshu (BL 23), Ganshu (BL 18), Pishu (BL 20), and Weishu (BL 21)were selected to nourish and strengthen liver and kidney, tonify spleen and stomach, promote blood circulation and unblock meridians to stop pain, and effectively improve the pathogenic changes of the osteoporosis patients. The Vitamin D2and Calcium Colloid Injection can supplement Vitamin D and calcium; the Ossotide Injection is majorly composed of multiple peptides involved in bone metabolism, working to regulate bone metabolism, stimulate the proliferation of osteoblast, promote the formation of fresh bone, regulate the metabolism of calcium and phosphorous, increase the density of bone calcium, prevent and treat osteoporosis, and relieve bony pain[8]; the CompoundDang Gui(Radix Angelicae Sinensis) Injection can promote blood circulation, unblock stagnation and kill pain. The three injections were combined to correct the imbalance of bone metabolism. In acupoint injection, with the function of acupoint, the medicine can produce a direct, higher, precise, efficient, and longer effect. Not to mention that acupoint injection is also characterized by less adverse effect[9-10]. Therefore, the study finally achieved a satisfactory efficacy by combining the above three medicines in acupoint injection. The 2-year follow-up study suggested that acupoint injection can reduce the rate of fracture, indicating that this treatment can increase bone mass and calcium, and make bone stronger. This treatment is easy-to-operate and safe with content therapeutic efficacy, and is worth promoting.
[1] Chinese Society of Osteoporosis and Bone Mineral Research of the Chinese Medical Association. Diagnosis and treatment guideline on primary osteoporosis (2011). Zhonghua Guzhishusong He Gukuangyan Jibing Zazhi, 2011, 4(1): 2-17.
[2] Ministry of Health of the People’s Republic of China. Guiding Principles for Clinical Study of New Chinese Medicines. Beijing: China Medico-Pharmaceutical Science & Technology Publishing House, 2005: 356-360.
[3] Pang Y, Zhao LH, Nong ZN, Ye FW, Liang JS, Su XD, Zhong X, Zhang JZ, Feng Z. Clinical study of acupuncturemoxibustion treatment for primary osteoporosis. Shanghai Zhenjiu Zazhi, 2008, 27(12): 15-16.
[4] Zhou ZH, Wang NQ, Pan FF, Wu ZH, Dai XY. Clinical observation on combined acupuncture and medication for osteoporosis in postmenopausal women. J Acupunct Tuina Sci, 2011, 9(6): 370-375.
[5] Wang XY, Zhang Y, Guo F. The influences of electroacupuncture plus estrogen on bone quantity and insulin-like growth factor in ovariectomized rats. Shanghai Zhenjiu Zazhi, 2006, 25(11): 33-35.
[6] Wang H, Bao SY, Zhou XL. Influence of “doublereinforcing and one-unblocking” acupuncture on the mineral content and the density of bone and estradiol in a rat model of postmenopausal osteoporosis. Shanghai Zhenjiu Zazhi, 2005, 24(10): 39-41.
[7] Pan FF, Zhou ZH, Wang YP, Wang XY, Zhao LX, Chen HD. Effect of combined use of acupuncture and medicine on serum E2and bone mineral density in postmenopausal osteoporosis rats. Shanghai Zhenjiu Zazhi, 2012, 31(6): 444-446.
[8] Meng XL, Ma DY, Wang C, Bai L, Li Y, Chen C. Clinical research of bone peptide for injection combined with Alendronate treatment. Shiyong Yaowu Yu Linchuang, 2012, 15(8): 490-491.
[9] Kang ZQ, Chen HD. Research progress of effect and action mechanism of acupoint injection. Zhejiang Zhongxiyi Jiehe Zazhi, 2010, 20(2): 119-120.
[10] Ouyang G, Wang DY, Li XM, Zhao L. Influence ofHuang Qi(Radix Astragali) injection on bone density of patients with primary osteoporosis. Tianjin Zhongyi, 2002, 19(5): 18-20.
Translator: Hong Jue
Received Date: April 18, 2013
R245.9
A
nts in the observation group
acupoint injection.
Author: Xia Shu-shu, M.D., associate chief physician
Qu Qun-wei, associate chief physician.
E-mail: hbsyshsz@foxmail.com
杂志排行
Journal of Acupuncture and Tuina Science的其它文章
- Clinical Observation on Acupoint Sticking Therapy for Lumbar Intervertebral Disc Hernination
- Treatment of Post-stroke Spastic Hemiplegia by Acupuncture plus Rehabilitation Training
- Clinical Observation on Electroacupuncture for Post-stroke Flaccid Paralysis
- Effect of Electroacupuncture on Anxiety and Craving in Heroin Addicts During Detoxification
- Clinical Observation on Acupuncture Treatment for Post-stroke Spastic Hemiplegia
- Immediate Effects of Hegu Needling on Adhesive Scapulohumeral Periarthritis
