Treatment of Post-stroke Spastic Hemiplegia by Acupuncture plus Rehabilitation Training
2013-07-18LiFangling
Li Fang-ling
Rehabilitation Department, Linxiang Hospital of Traditional Chinese Medicine, Hunan 414300, China
Treatment of Post-stroke Spastic Hemiplegia by Acupuncture plus Rehabilitation Training
Li Fang-ling
Rehabilitation Department, Linxiang Hospital of Traditional Chinese Medicine, Hunan 414300, China
Objective: To observe the clinical effects of acupuncture plus rehabilitation training for post-stroke spastic hemiplegia.
Methods: Eighty patients with post-stroke spastic hemiplegia in conformity with the inclusion criteria were randomly divided into two groups, a treatment group and a control group, 40 cases in each group. Both two groups were given treatments of routine Western medicine and rehabilitation training. Those in the treatment group were treated by puncturing antagonistic muscles, and those in the control group were given routine acupuncture treatment, to observe the changes in the scores of modified Ashworth scale (MAS), Fugl-Meyer assessment (FMA) and Barthel index (BI) after treatments in the two groups.
Results: After treatment, the scores of MAS, FMA and BI in the two groups were statistically different from those of the same group before the treatment (allP<0.01). After treatment, the differences in the scores of MAS, FMA and BI were all statistically significant (P<0.01 orP<0.05).
Conclusion: Acupuncture of antagonistic muscles plus rehabilitation training is better than routine acupuncture plus rehabilitation in the treatment of post-stroke spastic hemiplegia.
Acupuncture Therapy; Hemiplegia; Stroke; Complications; Rehabilitation; Myospasm
Stroke is a clinically common disease. The muscular spasm in the limbs after stroke hinders the restoration of the limb functions and seriously influences the patient’s quality of life. Therefore, to relieve the muscular spasm of the limbs is the key to rehabilitation treatment of stroke. I treated 40 cases of post-stroke spastic hemiplegia by puncturing antagonistic muscles plus rehabilitation training, in comparison of 40 cases under routine acupuncture plus rehabilitation training. Now, the report is given as follows.
1 Clinical Materials
1.1 Diagnostic criteria
1.1.1 Diagnostic criteria of Western medicine
The diagnostic criteria of Western medicine were based upon theKey Diagnostic Points for Cerebrovascular Diseases[1]stipulated in the Fourth National Conference on Cerebrovascular Diseases, and confirmed by CT or MRI.
1.1.2 Diagnostic criteria of traditional Chinese medicine (TCM)[2]
The major symptoms were hemiplegia, loss of consciousness, slurred speech or aphasia, abnormal sensation of half body, deviated mouth and tongue. The minor symptoms were headache, dizziness, choking cough with drinking water, deviated eye without blinking, and ataxia. Characterized by acute onset and inducing factors before the onset, there were often signaling symptoms. The age of the onset was over 40 years old. The diagnosis was confirmed upon over two major symptoms, or one major symptom and two minor symptoms, in combination with the onset, inducing factors, signaling symptoms and age. Without the above-mentioned conditions, the diagnosis was confirmed by imaging examination.
1.1.3 Staging criteria of disease[2]
Acute stage: The course of disease is within two weeks, and one month is the longest period for those with Zang-fu organs involvement.
Remission stage: The course of disease is two weeks to six months.
Sequelae stage: The course of disease is over six months.
1.2 Inclusion criteria
In conformity with the above diagnostic criteria of Western medicine and traditional Chinese medicine; within six months in the duration; with age ranging from 40-75 years old; male or female; with stable pathological condition and spastic muscles in the limbs; muscle tension >grade 0, but ≤grade 3 by modified Ashworth scale (MAS); having signed informed consent.
1.3 Exclusion criteria
Those not in conformity with the inclusion criteria; muscular spasm caused by other diseases; those with severe conscious disorder or unstable condition; those administrated by other anti-spastic agents; those complicated with severe primary diseases in the cardiac, cerebral, hepatic, renal and hematopoietic system and endocrine system; and those with mental disorder and those afraid of acupuncture or out of cooperation.
1.4 General data
Eighty cases with post-stroke spastic hemiplegia in conformity with the inclusion criteria came from the Rehabilitation Department, Linxiang Hospital of Traditional Chinese Medicine and were divided randomly into two groups, a treatment group and a control group by random table of Doll’s clinical cases, 40 cases in each group. The differences in gender, age, duration, onset pattern and hemiplegia between the two groups were not statistically significant (P>0.05), and the two groups were comparable (table 1).
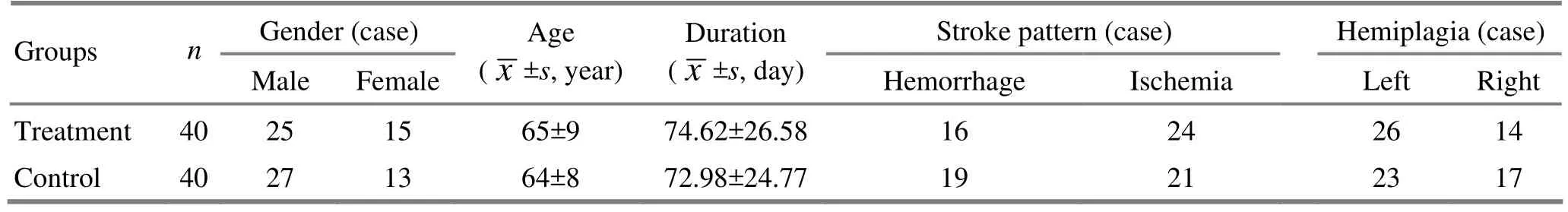
Table 1. Comparison of general information between the two groups
2 Therapeutic Methods
The two groups were given by routine neurological treatment, including regulating blood pressure, blood sugar and blood lipids, and improving cerebral metabolism, resisting infection and preventing complications, etc.
In addition, the rehabilitation training of the limb functions was based upon Bobath method, including placing the good limb on the bed, maintaining the activity of the joints, relieving the muscular spasm around the controlling points of the body movement, and static traction and passive motion and massage of the muscular spasm. ‘One to one’ treatment was given with above rehabilitation training by professional rehabilitation therapist, for 30 min each time.
2.1 Treatment group
Acupoints: Jianyu (LI 15), Quchi (LI 11), Hegu (LI 4), Houxi (SI 3), Waiguan (TE 5), Baxie (EX-UE 9), Weizhong (BL 40), Chengshan (BL 57), Xuehai (SP 10), Yinlingquan (SP 9), Sanyinjiao (SP 6), Zhaohai (KI 6), Taichong (LR 3) on the sick side.
Operation: The patient took a supine position. After routine disinfection of the acupoints, the needles of 0.30 mm in diameter and 25-50 mm in length were inserted quickly with one hand into the deep level of the muscle according to the patient’s body figure. After the arrival of the needling sensation, the needles were manipulated by weak stimulation (the twisting angle<180°, the lifting and thrusting amplitude <0.5 cm), and by the even needling technique for reduction. The needles were retained for 30 min and manipulated once every 10 min.
2.2 Control group
Acupoints: Jiquan (HT 1), Chize (LU 5), Neiguan (PC 6), Daling (PC 7), Huantiao (GB 30), Biguan (ST 31), Yanglingquan (GB 34), Zusanli (ST 36), and Jiexi (ST 41)[3].
Operation: After the acupoints were routinely disinfected, the needles of 0.30 mm in diameter and 25-75 mm in length were inserted quickly with one hand into the depth according to the patient’s body figure. After the arrival of the needling sensation, Neiguan (PC 6) was manipulated with the reducing technique. Chize (LU 5) was manipulated by the lifting and thrusting technique till the limb throbbed. The rest acupoints were manipulated by even needing technique. The needles were retained for 30 min and manipulated once every 10 min.
The rehabilitation training and acupuncture treatment were given once every day in the two groups, for five sessions per week and two weeks as one course. Totally, two courses were given.
3 Therapeutic Effects Observation
3.1 Observation indexes
3.1.1 MAS score[4]
The MAS score was used to assess the spasm degree of the patient’s limbs, by marking 0, 1, 2, 3, 4 and 5 points respectively in accordance with grade 0, I, I+, II, III and IV.
3.1.2 Fugl-Meyer assessment (FMA) score[4]
FMA score was used to assess the motor functions of the patient’s limb. By FMA score, 100 points meant normal motor functions; 96-99 points meant mild motor dysfunctions; 85-95 points meant moderate motor dysfunctions; 50-84 points meant obvious motor dysfunctions; 50 points and below meant severe motor dysfunctions.
3.1.3 Barthel index (BI) score[5]
BI score was used to assess the activities of daily living (ADL) of the patients. By BI score, 100 points meant normal; ≥60 points meant basic self-care; 41-59 points meant moderate disabilities, need help in life; 21-40 points meant severe disabilities, and obvious dependence in life; ≤20 points meant complete dependence in life.
The above indexes were assessed once respectively before and after treatment.
3.2 Statistic methods
The SPSS 16.0 software was used for statistical analysis. The counting data were expressed by mean ± standard deviation (). The counting data were expressed by rate or constituent ratio. The Chi-square test was used for the counting data. Thet-test was used while the counting data could meet the normality and variance homogeneity. The rank test was used while the counting data could not meet the normality and variance homogeneity.
3.3 Therapeutic results
In comparison of MAS score, FMA score and BI score after the treatment with those of the same group before the treatment in the two groups, the differences were statistically significant (P<0.01). In comparison of MAS score, FMA score and BI score after the treatment between the treatment group and control group, the differences were statistically significant (P<0.01,P<0.05), indicating that the improvement of the patients was better in the treatment group than in the control group (table 2).
Table 2. Comparison of various scores before and after treatment between the two groups (, point)

Table 2. Comparison of various scores before and after treatment between the two groups (, point)
Note: Compared to the same group before the treatment,P<0.01; compared to the control group after treatment, 2)P<0.01, 3)P<0.05
GroupsnTime MAS score FMA score BI score Treatment 40 Before treatment After treatment 2.84±0.98 1.59±1.011)3)47.54±10.26 72.41±9.351)2)45.86±7.39 66.85±10.241)3)Control 40 Before treatment After treatment 2.91±0.92 1.96±1.071)49.23±8.86 65.84±7.981)46.64±6.96 60.28±8.631)
4 Discussion
Post-stroke spastic paralysis is mostly manifested by flexion spasm of predominantly upper limb flexor muscles and tonic spasm of predominantly lower limb extensor muscles. It is the abnormal mode of motion based upon the spasm due to loss of the controlling ability of the high center on the involuntary motor functions and under the control of lower center[6]. Clinically, the changes of myodynamia are often focused upon predominantly in the assessment of post-stroke hemiplegia, and the key of the treatment is supposed to develop the myodynamia. Thus, the joint motion of the muscles in the limb is intensified, so as to lead to misuse syndrome, and aggravating spasm in the limb and hindering the rehabilitation of the patients.
Based upon the basic principle of modern rehabilitative medicine and the developing laws of the rehabilitation of post-stroke hemiplegia, in the treatment of post-stroke spastic hemiplegia, the attention should be stressed to coordinate the balance of muscular tension among the limb muscles, i.e. to strengthen the movement of the extensor muscles of the upper limb and flexor muscles of the lower limb, and antagonize the movement of the flexors muscles ofthe upper limb and extensor muscles of the lower limb, coordinate and balance the muscular tension between the agonist and antagonist muscles, promote the joint motion into separate motion, inhibit and control the muscular spasm of the limbs, so as to build up the normal motion mode. Judging from the characteristics of post-stroke spastic hemiplegia, the relative flaccidity of the extensor muscles of the upper limb (site of three yang meridians) and relative spasm of the flexors muscles (site of three yin meridian) are mainly manifested, opposite in the lower limb. Judging from pattern identification by the theory of meridians, it is induced by loss of balance between yin and yang. Therefore, the treatment should be designed to regulate yin and yang, restore the relative balance between yin and yang, to realize the goal of ‘yin in good condition and yang in good action’[7].
In accordance with the knowledge of modern medicine and meridian theory on post-stroke spastic hemiplegia, and by changing the idea to ‘select the acupoints only from the Yangming Meridians for paralysis’ in traditional Chinese medicine, I selected the acupoints on the extensor side and flexor side of the limb and applies different needling techniques to stimulate the spastic muscles and antagonistic muscles in alternation, so as to realize the balance of biomechanics and relieve the muscular spasm. Among the acupoints, Jianyu (LI 15), Quchi (LI 11) and Hegu (LI 4) are used jointly to dissipate wind, dredge the collaterals and lubricate the joints. Houxi (SI 3) and Waiguan (TE 5) are used in combination to clear away heat, dissipate wind, and dredge the meridians. Baxie (EX-UE 9) is used to relieve the local muscular spasm. The antagonistic muscles are distributed in the pathway of the Bladder Meridian of Foot Taiyang and Yang Heel Vessel of the lower limb, and Weizhong (BL 40) and Chengshan (BL 57) are from the Bladder Meridian and Zhaohai (KI 6) links with the Yang Heel Vessel. Therefore, Weizhong (BL 40), Chengshan (BL 57), and Zhaohai (KI 6) are stimulated to dredge the meridian qi of the Bladder Meridian and the Yang Heel Vessel for relieving spasm of the limb[8]. Xuehai (SP 10), Yinlingquan (SP 9), Sanyinjiao (SP 6) have the effects to strengthen the spleen and benefit the stomach, regulate qi and dissolve phlegm. Also, Sanyinjiao (SP 6) is a crossing acupoint of Three Yin Meridians of Foot and has the effects to reinforce the liver and kidney. Xuehai (SP 10) and Quchi (LI 11) are used to activate blood, expel wind and dredge the meridian jointly. Zhaohai (KI 6) is able to tonify the kidney, refill essence and benefit marrow. As the Yuan-Primary and Shu-Stream acupoint of the Liver Meridian of Foot Jueyin, Taichong (LR 3) is used to promote qi activity and dredge the meridians and collaterals. The combination of all acupoints is able to strengthen the spleen, benefit the kidney, tonify and soothe the liver, clear away heat, dissipate wind, activate blood, dissolve phlegm, and dredge the meridians and collaterals. Also, stroke is a syndrome with deficiency in constitution and excess in manifestations. Deficiency in the liver and kidney and insufficiency in qi and blood are the main reason, and pathogenic wind, fire, phlegm, qi and blood stasis are the inducing factors. The above acupoints are the effective acupoints for muscular spasm and are also able to support the anti-pathogenic ability and expel pathogens jointly, based upon the basic pathogenesis of stroke. Therefore, those acupoints can effectively contract the antagonistic muscles, relax the spastic muscles, maintain smooth circulation of qi and blood in the sick limb and restore the balance between yin and yang, so as to improve the motor functions of the limb.
It is pointed out in the theory of modern rehabilitative medicine that after stroke, the central nervous system has the re-organizing ability or moldability in structure and function, and some brain neuron could regenerate under appropriate conditions. The repeated training of Bobath technology-based neuromuscular facilitation techniques can continuously stimulate various neurons on the movement paths, regulate the excitability, so as to obtain the correct output of movement stimulation, and build up the normal movement mode and restore the motor functions[9].
It is indicated by the results from this study that acupuncture on antagonistic muscles plus rehabilitation training can obviously decrease the MAS score, elevate FMA score and BI score, better than routine acupuncture plus rehabilitation training (P<0.05 orP<0.01), indicating that acupuncture on antagonistic muscles plus rehabilitation training is better than routine acupuncture plus rehabilitation training in relieving the muscular spasm and improving the motor functions of the limb, and in daily living ability, almost identical to the research results of Zhang WM, et al[10]and the report of Jin Z, et al[11].
[1] Chinese Neuroscience Society, Chinese Neurosurgical Society. Key diagnostic points for cerebrovascular diseases. Zhonghua Shenjingke Zazhi, 1996, 29(6): 379-380.
[2] Ministry of Health of the People’s Republic of China. Guiding Principles for Clinical Study of New Chinese Medicines. Beijing: China Medico-Pharmaceutical Science & Technology Publishing House, 2002: 99-104.
[3] Shi XM. Acupuncture and Moxibustion Science. Beijing: China Press of Traditional Chinese Medicine, 2004.
[4] Dou ZL. Spasm: Evaluation and Treatment. Beijing: People’s Medical Publishing House, 2004: 41-42.
[5] Department of Medical Administration, Ministry of Health of the People’s Republic of China. Diagnostic and Therapeutic Standards of China Rehabilitative Medicine. Beijing: Huaxia Publishing House, 1999: 220-231.
[6] Jiang GM, Wu SP, Jia C, Liu YF. Observation of clinical effects in the treatment of post-stroke spastic hemiplegia by puncturing antagonist muscles and agonist muscles by different stimulating intensity. Zhenjiu Linchuang Zazhi, 2008, 24 (11): 1-3.
[7] Zhao XF, Li P. Efficacy of “remissive stage-reinforcing and acute stage-reducing” acupuncture for treating 30 apoplectic myospasm patients. J Acupunct Tuina Sci, 2006, 4(3): 140-143.
[8] Shen WN. Clinical observations on yin-reducing acupuncture for the treatment of post-stroke spastic hemiplegia. Shanghai Zhenjiu Zazhi, 2010, 29(6): 364-366.
[9] Jin RJ, Zhu TM, Wang Q. Clinical observation on spastic paralysis caused by cerebral infarction treated by electric stimulation on acupuncture of antagonistic muscles and facilitation techniques. Chengdu Zhongyiyao Daxue Xuebao, 2010, 33(3): 9-12.
[10] Zhang WM, Zheng P. Post-apoplexy spasm treated with acupuncture on antagonistic muscles combined with modern rehabilitation training therapy. Shijie Zhongxiyi Jiehe Zazhi, 2011, 6(4): 291-293, 304.
[11] Jin Z, Li ZX, Wang YL, Wang LJ, Bao DP. Clinical observations on double-needle acupuncture for the treatment of post-stroke leg hypermyotonia. Shanghai Zhenjiu Zazhi, 2011, 30(2): 93-95.
Translator: Huang Guo-qi
R246.6
A
Date: April 18, 2013
Author: Li Fang-ling, attending physician.
E-mail: b2134618@163.com
杂志排行
Journal of Acupuncture and Tuina Science的其它文章
- Efficacy Observation on Acupuncture Combined with Auricular Point Sticking Treatment for Primary Dysmenorrhea
- Immediate Effects of Hegu Needling on Adhesive Scapulohumeral Periarthritis
- Clinical Observation on Acupoint Sticking Therapy for Lumbar Intervertebral Disc Hernination
- Clinical Study on Acupoint Injection for Primary Osteoporosis
- Effect of Electroacupuncture on Anxiety and Craving in Heroin Addicts During Detoxification
- Clinical Observation on Electroacupuncture for Post-stroke Flaccid Paralysis
