Clinical Observation on Acupuncture Treatment for Post-stroke Spastic Hemiplegia
2013-07-18ZhangYanLiuGuochengWangJinyuSunYunguangYangLiujiang
Zhang Yan, Liu Guo-cheng, Wang Jin-yu, Sun Yun-guang, Yang Liu-jiang
Liuzhou Hospital of Traditional Chinese Medicine, Guangxi 545001, China
Clinical Observation on Acupuncture Treatment for Post-stroke Spastic Hemiplegia
Zhang Yan, Liu Guo-cheng, Wang Jin-yu, Sun Yun-guang, Yang Liu-jiang
Liuzhou Hospital of Traditional Chinese Medicine, Guangxi 545001, China
Objective: To observe the clinical effect of contralateral needling plus rehabilitation for post-stroke spastic hemiplegia.
Methods: Thirty-six patients with post-stroke spastic hemiplegia were randomly divided into a treatment group and a control group, 18 cases in each group. The two groups were all given rehabilitation training. The contralateral needling was adopted in the treatment group on the acupoints group of brain-refreshing and orifice-opening needling method. The routine acupuncture was applied in the control group on the same acupoints. Respectively before and after the treatment, the modified Ashworth scale (MAS) and clinical spasticity index (CSI) were used to assess the therapeutic effects.
Results: The total effective rate was 94.4% in the treatment group and 67.7% in the control group, with a statistical difference in comparison of the two groups (P<0.05). In comparison of MAS and CSI scores after the treatment between the treatment group and control group, the differences were statistically significant (P<0.05).
Conclusion: The contralateral needling plus rehabilitation training is an effective method for the treatment of post-stroke spastic hemiplegia.
Acupuncture Therapy; Opposing Needling; Needling Methods; Stroke; Complications; Hemiplegia; Rehabilitation
Spastic hemiplegia is one of the commonly encountered sequelae after stroke, manifested by persistently elevated muscle tone of the limb, pain in the limb, stiffness in the joints, and even permanent joint contracture. It can severely influence the functional training and rehabilitation of the patients. The longer the spastic status lasts, the more difficult the normal motor mode can be built up. Therefore, to control spasm and promote the appearance of disengaging movement is the key in the rehabilitation of stroke[1]. How to effectively relieve the spastic status in the paralyzed limb is a difficult issue in the service of the neurological and rehabilitative clinic. In modern medicine, rehabilitative means are stressed to perform the training of anti-spastic mode, avoiding any stimulation that could cause spasm and stretching and extending the involved limb actively or passively. But the effects are not satisfactory. In the recent years, there are many reports on acupuncture treatment of spastic status after cerebrovascular diseases, and there are also large varieties of acupuncture methods[2-5]. In this study, 19 cases of post-stroke spastic hemiplegia were treated by the contralateral needling plus modern rehabilitation training, in comparison of 18 cases treated with routine acupuncture plus rehabilitation training. Now, the report is given as follows.
1 Clinical Materials
1.1 Diagnostic criteria
TheStandard for Diagnosis and Therapeutic Effect Evaluation of Stroke(Trial)[6]was referred to the diagnostic criteria of traditional Chinese medicine. TheKey Diagnostic Points for Cerebrovascular Diseases[7]was referred to the diagnostic criteria of Western medicine.
1.2 Inclusion criteria
In conformity with the above diagnostic criteria of traditional Chinese medicine and Western medicine; between grade 0-3 of the muscle tone of the upper limb by modified Ashworth scale (MAS), between 8-12 points of the muscle tone of the lower limb by clinical spasticity index (CSI); age ranged from 50-75 years old; duration from two weeks to six months; and first onset or previous history of brain stroke, but without sequelae.
1.3 Exclusion criteria
Those with unstable stroke, such as mental disorder, aphasia; those with severe complications, such as severe mental disorder or cognitive disorder, Parkinson’s disease, severe cardiac, hepatic and renal dysfunction; previous diseases severely affecting the functions of the limbs, such as neurological and muscular diseases, and rheumatoid, bone fracture and traumatic injury; previous history of stroke remained with elevated muscle tone; and those unable to complete the observation by the research method.
1.4 General data
Thirty-six cases in conformity with the inclusion criteria were the hospitalized patients from the Encephalopathy Department, Liuzhou Hospital of Traditional Chinese Medicine, and were divided randomly by their visit order into the treatment group or the control group, 18 cases in each group. In the treatment group, there were 11 males and 7 females, with the age ranging from 50 to 75 years old, at the average age of 67, with the duration ranging from 2 weeks to 24 weeks, at the average of 10.17 weeks. In the control group, there were 10 males and 8 females, with the age ranging from 51 to 74 years old, at the average age of 66, with the duration ranging from 2 weeks to 23 weeks, at the average of 9.83 weeks. In the comparison of gender, age and duration, the differences were not statistically significant (P>0.05), indicating that the two groups were comparable.
2 Therapeutic Methods
The similar symptomatic treatment was given to the two groups by traditional Chinese and Western medications. In Chinese medicine, the treatment was given to soothe and dredge the meridians and collaterals. In Western medicine, the treatment was given to control blood pressure, blood sugar, nourish the nerves, resist coagulation of blood platelets, and improve micro-circulation. During the observation period, any other medications that could influence the assessment of therapeutic effects were prohibited.
2.1 Treatment group
2.1.1 Acupuncture
Major acupoints: Jianyu (LI 15), Quchi (LI 11), Waiguan (TE 5), Hegu (LI 4), Yanglingquan (GB 34), Xuanzhong (GB 39), and Zulinqi (GB 41) on the healthy side.
Adjunct acupoints: Hegu (LI 4) was punctured toward Sanjian (LI 3) and Baxie (EX-UE 9) were added for clenched fingers; Hegu (LI 4) toward Laogong (PC 8) and Houxi (SI 3) toward Laogong (PC 8) were added for disability to extend and flex the fingers; Jianzhen (SI 9), Naoshu (SI 10), Tianzong (SI 11), Quyuan (SI 13), and Bingfeng (SI 12) were added for disability to raise the shoulder and arm; Qiuxu (GB 40) toward Zhaohai (KI 6), Shenmai (BL 62), Jiexi (ST 41), and Bafeng (EX-LE 10) were added for strephenopodia.
Operation: After routine disinfection of the above acupoints, the needles of 0.35 mm in diameter and 50 mm in length were inserted quickly with the contralateral needling method and manipulated with the lifting-thrusting, twisting and rotating techniques for tonifying. After the arrival of the needling sensation, the needles were retained for 30 min.
2.1.2 Rehabilitation training
After acupuncture, the rehabilitation treatment of kinesiotherapy was performed under the guidance of rehabilitation therapist.
Position of good limb: The patients always maintain the correct body position on bed, wheelchair and chair, mainly by the extension position of the upper limb in the mode to resist the flexor spasm, and mainly by the flexion position of the lower limb in the mode to resist extensor spasm.
Passive traction training of joints and muscles: Such as pulling the spastic muscles passively and slowly for a long time.
Passive training of joint activity: Such as passive and full range movement of the joints of the involved limb.
Manual massage and treatment by air pressure therapy apparatus: Massage from the distal part to the proximal part of paralyzed limbs or by air pressure therapy apparatus.
Standing training: To perform the standing training on the electric standing bed, standing frame or within the balance rails, to step on the oblique board with the affected limb during standing, to tract the triceps muscles.
Weight-reducing walking training: By reducing the partial body weight of the patient with the air pressure suspender of the walking training device, cutting down the walking load in the lower limb, the patient could do the walking training with the normal walking manner on the treadmill, so as to complete the periodical walking action and enhance the balance and coordination.
2.2 Control group
Major acupoints: Neiguan (PC 6), Shuigou (GV 26), Sanyinjiao (SP 6), Jiquan (HT 1), Chize (LU 5), Weizhong (BL 40), Fengchi (GB 20), Wangu (GB 12), and Tianzhu (BL 10).
Adjunct acupoints: As same as the treatment group
Operation: By brain-refreshing and orifice-opening technique with the filiform needle of 0.35 mm in diameter and 50 mm in length, after routine disinfection, Neiguan (PC 6) was punctured perpendicularly for 1-1.5 cun and manipulated with the lifting, thrusting, twisting and rotating technique for reduction for 1 min. Shuigou (GV 26) was punctured upward toward the nasal septum obliquely for 0.5 cun and manipulated with bird-pecking method, till moist in the eyes or lacrimation. Sanyinjiao (SP 6) was punctured along the posterior border of the tibia 3 cun above the medial malleolus backward and obliquely with 45° between the skin and needle for 1-1.5 cun and manipulated with the lifting and thrusting technique for tonifying, till twitching in the lower limb for three times. Jiquan (HT 1), Chize (LU 5), and Weizhong (BL 40) were punctured perpendicularly for 1-1.5 cun by the lifting and thrusting technique, till twitching in the upper limb or lower limb for three times. After Fengchi (GB 20), Wangu (GB 12), and Tianzhu (BL 10) were manipulated by the twisting and rotating technique for tonifying, and the needles were retained for 30 minutes.
The rehabilitation training was as same as in the treatment group.
The patients in the two groups were treated once every day, for 6 sessions a week. Two weeks made one course. The therapeutic effects were assessed after two courses.
3 Observation on Therapeutic Effects
3.1 Observed indexes
Spasm of the patient’s affected upper limb was assessed by MAS.
Grade 0: No increase in muscle tone.
Grade I: Slight increase in muscle tone, giving a catch when part is moved in flexion or extension; or with‘locking’ and ‘sudden releasing’ sensation in extension, or with appearance of minimum resistance in the last range of motion of the joint.
Grade I+: Slight increase in muscle tone, manifested by slight locking sensation, and always accompanied by minimum resistance in the rest range of the motion (ROM) of the joint (less than 1/2 ROM).
Grade II: More marked increase in muscle tone, but the involved part is easy for passive motion.
Grade III: Considerable increase in muscle tone, the involved part is difficult for passive motion.
Grade IV: The affected part is rigid in flexion or extension, unable to move in tonic status.
Spasm of the patient’s affected lower limb was assessed by CSI, including the three aspects of heel tendon reflex, muscle tone of the triceps in the leg (score 2) and paroxysmal ankle spasm.
0 point: No heel tendon reflex, no resistance (flaccid).
1 point: Decreased heel tendon reflex, decreased resistance (low tension, no paroxysmal spasm).
2 points: Normal heel tendon reflex, normal resistance, paroxysmal spasm for 1-2 times.
3 points: Active heel tendon reflex, mild to medium increased resistance, still able to complete the passive movement of the ankle joint within the range of motion, paroxysmal spasm over three times.
4 points: Hyperactive heel tendon reflex, severely increased resistance, unable or very difficult to complete the passive movement of the ankle joint within the range of motion, paroxysmal spasm over 30 seconds.
3.2 Criteria of therapeutic effects
Spasm of the upper limb was assessed by MAS, with the wrist joint and elbow joint as the observed targets.
Remarkable effect: MAS scores decrease by over two grades.
Effect: MAS scores decrease by two grades.
Improvement: MAS scores decrease by one grade.
Failure: MAS scores do not change or even increase.
Spasm of the lower limb was assessed by CSI. Mild spasm is 0-9 points; medium spasm is 10-12 points; and severe spasm is 13-16 points.
3.3 Statistical methods
The SPSS 13.0 software was used for data analysis. The counting data was expressed by mean ± standard deviation (). Thet-test was used for statistic analysis and the Chi-square test was used for the counting data.P<0.05 was used to express statistical significance in differences.
3.4 Therapeutic results
3.4.1 Comparison of clinical effects between the two groups
The total effective rate was 94.4% in the treatment group and 66.7% in the control group, and the difference between the two groups was statistically significant (P<0.05), indicating that the total effective rate was better in the treatment group than that in the control group (table 1).
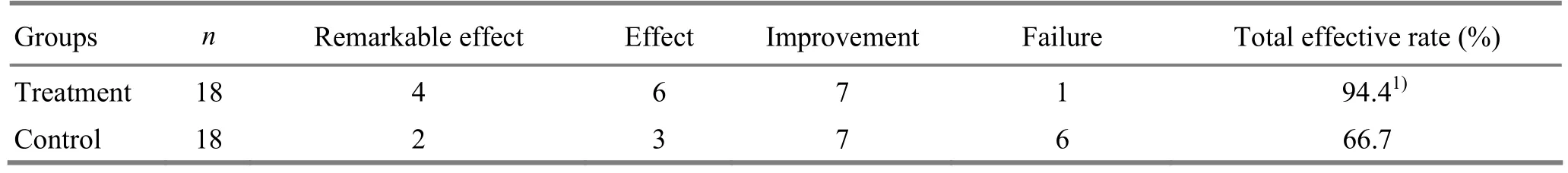
Table 1. Comparison of clinical effects between the two groups (case)
3.4.2 Comparison of MAS and CSI scores before and after treatment between the two groups
In comparison of MAS scores and CSI scores after the treatment between the two groups, the differences were all statistically significant (P<0.05), indicating that MAS scores and CSI scores were improved better in the treatment group than in the control group (table 2).
Table 2. Comparison of MAS and CSI scores between the two groups (, point)
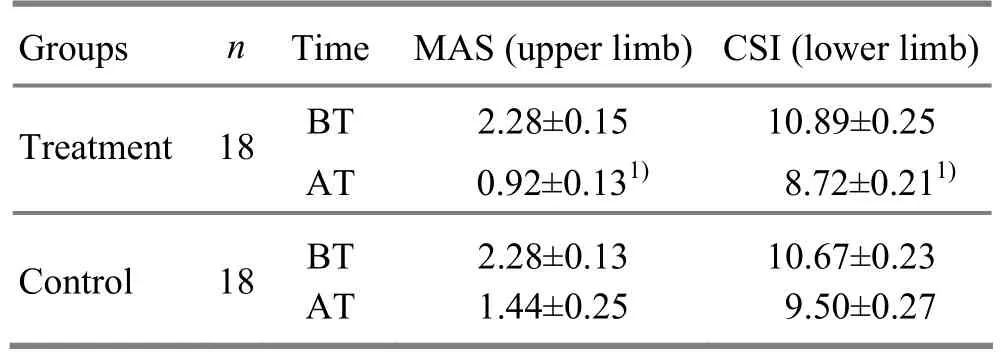
Table 2. Comparison of MAS and CSI scores between the two groups (, point)
Note: BT=Before treatment; AT=After treatment; compared to the control group, 1)P<0.05
GroupsnTime MAS (upper limb) CSI (lower limb) Treatment 18 AT 0.92±0.131)8.72±0.211)BT 2.28±0.15 10.89±0.25 Control 18 BT AT 2.28±0.13 1.44±0.25 10.67±0.23 9.50±0.27
3.5 Assessment of safety
During the treatment, no adverse reaction occurred in the patients of the two groups.
4 Discussion
Contralateral needling is first seen inLing Shu(Spiritual Pivot). As one of the ancient nine acupuncture methods, the contralateral needling has been used to treat post-stroke hemiplegia since the ancient times. In accordance with the meridian theory, the pathways of the meridians on the two sides of the human body are linked with the eight extraordinary meridians via Zang-fu organs. Some meridians are crisscrossed. Therefore, the pathways of the meridians on the two sides of the body are mutually regulated, mutually dependent, and mutually influential in pathology. In the treatment, they can be mutually adjusted. So, traditional Chinese medicine mechanism of the contralateral needling in treating diseases is mainly to select the acupoints on the healthy side to correct deficiency, get rid of excess and regulae the meridians on the two sides of the body and balance the yin and yang[8], so as to achieve the purpose of treating diseases.
The nervous anatomical mechanism of the contralateral needling has also been explored in the modern acupuncture research. It is believed that the influence of acupuncture signals the brainstem level is not only bilateral but also diffusive and extensive, which can be used to explain the contralateral needling is suitable for hemiplegia induced by stroke. It has been also found out in other study that amino acid neurotransmitter participates in the spastic paralysis appearing after stroke. By regulating the intracerebral metabolism via neurohormonal channel, acupuncture maybe reduce the contents of exciting amino acid in the cerebrospinal fluid of the patients, elevate the inhibiting amino acid level and inhibit the abnormally exciting transmission, so as to produce the effect of relieving the spastic status of the limbs[9].
The contralateral needling plus rehabilitative training for post-stroke spastic hemiplegia is not only applied with the traditional theory of meridians and acupoints in Chinese medicine and is also integrated with the anatomical and rehabilitative theory in modern medicine, so it can be used to initiate the meridian qi, supplement its insufficiency, assist dissipation of pathogens and relieve spasm[10-12].
In this study, by the application of MAS and CSI scores as the criteria for assessment of the therapeutic effects to contribute the clinical foundation in the treatment of post-stroke spastic hemiplegia by the contralateral needling plus rehabilitative training, it has been proved that this therapy is a better plan for the patients with post-stroke spastic hemiplegia, with higher medical marketing and popularizing value for extensive service.

[1] Ma C, Peng LP, Xie ZQ, Wang L, Wang XL. Influence of comprehensive treatment on apoplectic hemiplegia. Zhonghua Wuli Yixue Yu Kangfu Yixue Zazhi, 2004, 1(26): 50-51.
[2] Wang LP, Zhou W, Zhang SY. Clinical study on acupuncture effect for spastic paralysis following cerebrovascular disease. J Acupunct Tuina Sci, 2010, 8(6): 353-356.
[3] Wang LP, Zhou W, Zhang SY. Investigation and evaluation of the efficacy of scalp and body acupuncture for treating spastic paralysis after cerebrovascular diseases. Shanghai Zhenjiu Zazhi, 2007, 26(7): 3-5.
[4] Zhao XF, Li P. Efficacy of “remissive stage-reinforcing and acute stage-reducing” acupuncture for treating 30 apoplectic myospasm patients. J Acupunct Tuina Sci, 2006, 4(3): 140-143.
[5] Yu GQ. Observations on the efficacy of GV-regulating and Yang-activating acupuncture in treating postapoplectic spasmodic paralysis. Shanghai Zhenjiu Zazhi, 2009, 28(10): 577-578.
[6] Collaborative Group of Acute Encephalopathy of State Administration of Traditional Chinese Medicine. Standard for diagnosis and therapeutic effect evaluation of stroke (trial). Beijing Zhongyiyao Daxue Xuebao, 1996, 19(1): 55-56.
[7] Chinese Neuroscience Society, Chinese Neurosurgical Society. Key diagnostic points for cerebrovascular diseases. Zhonghua Shenjing Waike Zazhi, 1997, 13 (1): 3-4.
[8] Zhang JF, Sun GS. Professor Sun Liu-he’s clinical experience in using contralateral needling. Zhongyiyao Xuekan, 2005, 23(10): 36-37.
[9] Yue ZH, Yuan JL, Jiang JM. Muscle tension needling method for treatment of poststroke spasticity and effects on GLU and GABA contents in spinal fluid. Zhongguo Zhenjiu, 2004, 24(8): 565-567.
[10] Chen ZG. Effect of opposing needling combined movement method on upper limb spasm of hemiplegic patients. Zhongguo Kangfu Lilun Yu Shijian, 2004, 10(12): 744.
[11] Wang Y, Han W, Guo Y, Zhang DZ. Clinical observations on the efficacy of Jin three needles in treating post-stroke hemiplegia. Shanghai Zhenjiu Zazhi, 2010, 29(10): 638-640.
[12] Wang JH, Zhou JC, Liu G. Effect of acupuncture at Back-Shu points on motor function in hemiplegic stroke patients. Shanghai Zhenjiu Zazhi, 2010, 29(12): 770-772.
Translator: Huang Guo-qi
R246.6
A
Date: May 20, 2013
Author: Zhang Yan, M.M., attending physician.
E-mail: zjtnyx@126.com
杂志排行
Journal of Acupuncture and Tuina Science的其它文章
- Clinical Observation on Acupoint Sticking Therapy for Lumbar Intervertebral Disc Hernination
- Clinical Observation on Electroacupuncture for Post-stroke Flaccid Paralysis
- Effect of Electroacupuncture on Anxiety and Craving in Heroin Addicts During Detoxification
- Clinical Study on Acupoint Injection for Primary Osteoporosis
- Treatment of Post-stroke Spastic Hemiplegia by Acupuncture plus Rehabilitation Training
- Immediate Effects of Hegu Needling on Adhesive Scapulohumeral Periarthritis
