Effect of Combined Jin’s Three-needle and Rehabilitation Care on Post-stroke Hemiplegia
2013-07-18ZhouZhaohuiZhuangLixingXuZhanqiongLiaoMuxiZhangBin
Zhou Zhao-hui, Zhuang Li-xing, Xu Zhan-qiong, Liao Mu-xi, Zhang Bin
Acupuncture Department, the First Hospital Affiliated to Guangzhou University of Traditional Chinese Medicine, Guangdong 510405, China
Effect of Combined Jin’s Three-needle and Rehabilitation Care on Post-stroke Hemiplegia
Zhou Zhao-hui, Zhuang Li-xing, Xu Zhan-qiong, Liao Mu-xi, Zhang Bin
Acupuncture Department, the First Hospital Affiliated to Guangzhou University of Traditional Chinese Medicine, Guangdong 510405, China
Objective: To observe and compare the efficacy differences between combined Jin’s three-needle and rehabilitation training and rehabilitation training alone for hemiplegia following an ischemic stroke.
Methods: A total of 94 cases who met the inclusion criteria were randomized into an observation group using combined Jin’s three-needle and rehabilitation training and a control group using rehabilitation training alone. The therapeutic efficacies were then assessed respectively before treatment, 14 d and 28 d after treatment using neurological deficient scale (NDS) and short-form Fugl-Meyer assessment (SFFMA) scale.
Results: After treatment, the NDS and SFFMA scores in both groups were significantly improved (P<0.05); after 28-day treatment, the inter-group comparison showed a statistical significance (P<0.05).
Conclusion: Combined Jin’s three-needle and rehabilitation training and rehabilitation training alone can both enhance the nerve function recovery of patients with post-stroke hemiplegia and improve their motor function; however, the former could obtain better effects than the latter.
Acupuncture Therapy; Scalp Stimulation Areas; Stroke; Complications; Hemiplegia; Rehabilitation
Stroke is an umbrella term for acute cerebrovascular diseases in Chinese medicine. It is characterized by high incidence rate, high mortality rate, high disability rate, high recurrence rate and multiple complications. A sudden onset of stroke is often associated with yin-yang imbalance and disorder of qi and blood. Stroke can be diagnosed as yin deficiency of the liver and kidney with excessive symptoms related to wind, fire, phlegm, qi and stasis. The yin deficiency and excessive symptoms can be both cause and effect. In remission stage, stroke is characterized by retention of pathogenic qi but unrecovered healthy qi. In modern medicine, stroke can be ischemic (70%) or hemorrhagic. Statistically, approximately 80% stroke patients may suffer from functional impairment or hemiplegia, which can severely affect the family and society[1].
Further to previous scientific and clinical practice, staff from the Acupuncture Department of our hospital proposed this optimal protocol of Jin’s three-needle for ischemic post-stroke hemiplegia and obtained better clinical effects. In order to investigate the role of Jin’s three-needle in post-stroke hemiplegia, we compared the treatment effects of ischemic post-stroke hemiplegia using combined Jin’s three-needle and rehabilitation training and rehabilitation training alone. The results are now summarized as follows.
1 Clinical Materials
1.1 Diagnostic criteria
1.1.1 Diagnostic criteria in Western medicine
The diagnostic criteria in Western medicine is based on theKey Diagnostic Points for Cerebrovascular Diseases[2].
1.1.2 Diagnostic criteria in traditional Chinese medicine
The diagnostic criteria in traditional Chinese medicine is based on theStandard for Diagnosis and Therapeutic Effect Evaluation of Stroke(Trial)[3].
1.2 Inclusion criteria
Involvement of the carotid artery in the cerebrovascular accidents that has been confirmed by head CT or MRI scan; less than or equal to twice strokes lasting from 15 d to 3 months; men or women aged between 40 and 79; the limb functional impairment score of NDS ≥10; having a clear consciousness and stable vital signs; having signed the informed consent.
1.3 Exclusion criteria
Transient ischemic attack (TIA); reversible ischemic neurologic deficit (RIND); neurologic deficits caused by hemorrhagic cerebrovascular disease, brain tumor, brain trauma, cerebral parasitic disease, heart disease or metabolic disorder; women during pregnancy or lactation; more than or equal to 3 times of stroke; having complications of mental disorders and severe primary problems involving heart, liver, kidney, and hematopoietic or metabolic systems.
1.4 Grading standard for limb paralysis
This is based on the six-stage Brunnstrom approach.
Flaccidity (Brunnstrom stages I-II): No voluntary movements on the affected side can be initiated or minimal synergic reaction.
Spasticity (Brunnstrom stages III-V): Apparent spasticity of upper limb flexors and lower limb extensors.
1.5 General data
A total of 94 inpatients, treated in the Departments of Acupuncture and Neurology, the First Hospital Affiliated to Guangzhou University of Traditional Chinese Medicine, were randomized into an observation group and a control group. Of 49 cases in the observation group, there were 29 males and 20 females with an average age of (65±8) years. Of 45 cases in the control group, there were 24 males and 21 females with an average of (65±7) years. Before treatment, there were no statistical significances between two groups in gender, age and scores of NDS and SFFMA (P>0.05), indicating that the two groups were comparable.
2 Treatment Methods
2.1 Basic treatment
According to theChina Guidelines for Prevention and Treatment of Cerebrovascular Diseases, the patients were treated with medications to prevent platelet aggregation and control blood pressure, blood sugar and blood fat, along with symptom-oriented therapy and nutritional supports.
2.2 Observation group
2.2.1 Flaccid paralysis
Major points: Temporal three-needles (the 1st needle on the contralateral temple of the affected side, 2 cun within the hairline directly above the ear apex; the 2nd and 3rd needles are 1 cun parallel anterior and posterior), three hand needles [Quchi (LI 11), Waiguan (TE 5) and Hegu (LI 4)] and three foot needles [Futu (ST 32), Zusanli (ST 36) and Taichong (LR 3)].
Adjunct points: For deviated mouth corner, combine with three mouth needles [Dicang (ST 4), Yingxiang (LI 20) and Jiachengjiang (Extra)]; for slurred speech and difficulty swallowing, combine with three tongue needles [Shanglianquan (Extra), Zuoshanglianquan (1 cun left to Shanglianquan) and Youshanglianquan (1 cun right to Shanglianquan)]; for hyperactivity of liver yang, combine with Taichong (LR 3); for wind-phlegm obstructing meridians, combine with Fenglong (ST 40); for qi deficiency with blood stasis, combine with Zusanli (ST 36); and for wind stirring due to yin deficiency, combine with Taixi (KI 3).
2.2.2 Spastic paralysis
Major points: Temporal three-needles, three needles for spasticity of upper extremities [Jiquan (HT 1), Chize (LU 5) and Neiguan (PC 6)], three needles for spasticity of lower extremities [Shuxi (Extra), Yinlian (LR 11), Yinlingquan (SP 9) and Sanyinjiao (SP 6)].
Adjunct points: For aphasia, combine with three tongue needles; for deviated mouth corner, combine with three mouth needles; for severe spasm of the wrist joint, combine with three wrist needles [Yangxi (LI 5), Yangchi (TE 4) and Daling (PC 7)]; for inversion of the ankle joint, combine with three ankle needles [Taixi (KI 3), Kunlun (BL 60) and Jiexi (ST 41)]; for inability to extend upper and lower limbs due to spasticity, combine with three opening needles [Shuigou (GV 26), Yongquan (KI 1) and Zhongchong (PC 9)]; for edema of the fingers/toes, combine with Baxie (EX-UE 9) and Bafeng (EX-LE 10); and for pattern identification, refer to the treatment for flaccid paralysis.
2.2.3 Needling method
After routine disinfection with 75% alcohol, puncture above points using filiform needles of 0.32 mm in diameter and 25-50 mm in length with even reinforcing-reducing manipulation by rapid small-amplitude twisting.
2.2.4 Rehabilitation training[4]
Flaccid paralysis: Good limb-bit display on the bed; passive joint motion to prevent joint contracture or deformity; bed activities; sitting training; bridge movement; and active motion induced by excitabilityenhancing manipulation such as synergic reaction, associated movement and sensory stimulation.
Spastic paralysis: Release of muscle tone; sitting balance training; sitting-to-standing transfer; standing balance training; walking training; and upper limb controllability training.
2.2.5 Course of treatment
A course of treatment consisted of 28 d, 5 times a week, and 4 weeks in total. This was coupled with a 28-day basic medication treatment.
2.3 Control group
Same rehabilitation training protocol and course of treatment were adopted as the observation group.
3 Results Observation
3.1 Assessment criteria
The therapeutic efficacies were assessed before treatment, 14 d and 28 d after treatment using NDS and SFFMA scales[5].
3.2 Statistical method
The SPSS 11.5 version software was used for input of database and statistical analysis. For intra- and inter-group comparison before and after treatment, Chi-square test was used for numeration data,Riditanalysis for ranked data, andt-test and analysis of variance for measurement data.
3.3 Results
3.3.1 Changes in NDS scores
The one-factor analysis of variance showed that there were statistical significances in NDS scores after 14–day and 28-day treatment (P<0.05). The independent samplest-test showed that there were no inter-group statistical significances in NDS scores before and after 14-day treatment (P>0.05); however, there were inter-group statistical significances before and after 28-day treatment (P<0.05). This indicates that, after 28-day treatment, patients in the observation group had better improvement in neurologic deficit than those in the control group (table 1).
3.3.2 Changes in SFFMA scores
According to independent samples t-test, there was no statistical significance in NDS scores before and after 14-day treatment (P>0.05). According to one-factor analysis of variance, there were statistical significances in SFFMA scores before and after 14-day treatment in both groups; and a statistical significances also appeared between 14-day and 28-day treatment (P<0.05). After 28-day treatment, there was an inter-group statistical significance in SFFMA score (P<0.05), indicating that patients in the observation group had better improvement in motor functions than those in the control group (table 2).
Table 1. Between-group comparison of NDS before and after treatment (, point)
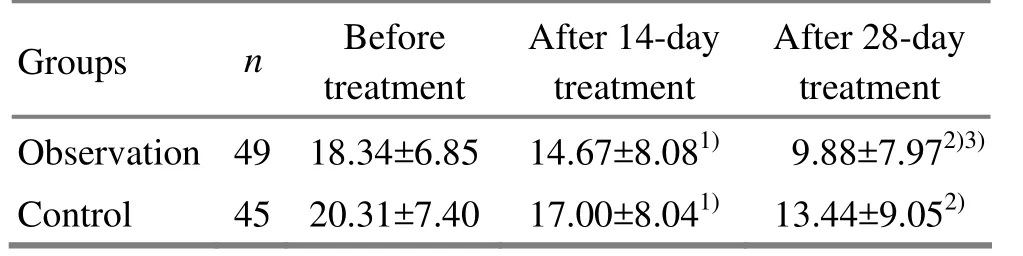
Table 1. Between-group comparison of NDS before and after treatment (, point)
Note: Intra-group before-after treatment comparison, 1)P<0.05; intra-group comparison after 14-day treatment, 2)P<0.05; inter-group comparison, 3)P<0.05
Observation 4918.34±6.8514.67±8.081)9.88±7.972)3)Control 4520.31±7.4017.00±8.041)13.44±9.052)
Table 2. Between-group comparison of SFFMA scores before and after treatment (, point)
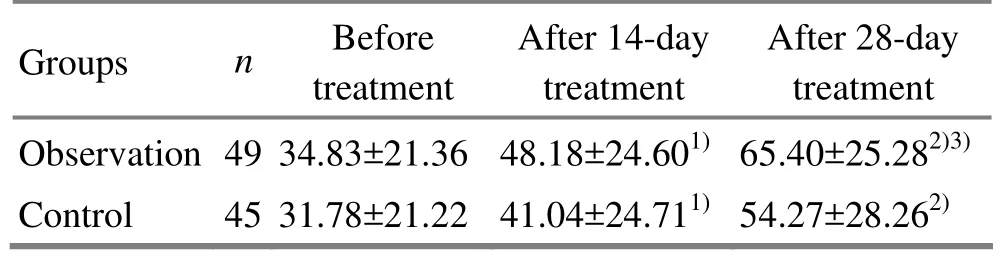
Table 2. Between-group comparison of SFFMA scores before and after treatment (, point)
Note: Intra-group before-after treatment comparison, 1)P<0.05; the intra-group comparison after 14-day treatment, 2)P<0.05; the inter-group comparison, 3)P<0.05
GroupsnBefore treatment After 14-day treatment After 28-day treatment Observation 49 34.83±21.3648.18±24.601)65.40±25.282)3)Control 45 31.78±21.2241.04±24.711)54.27±28.262)
4 Discussion
According to the condition and severity of poststroke hemiplegia, the Jin’s three-needle therapy includes three needles involving the temple, hand, foot and three needles for spasticity of the upper and lower extremities[6-8]. Since flaccid paralysis mainly manifests as contracture of yang meridians and flaccidity of yin meridians, three points involving the temple, hand and foot were selected, mainly in Yangming and Shaoyang Meridians. For spastic paralysis, three temporal points and three points for spasticity of the upper and lower extremities were selected, mainly in Taiyin and Jueyin Meridians.
Located in the temporal region along the pathways of Shaoyang Meridians, the three temporal needles can circulate qi and blood of the Liver and Gallbladder Meridians, soothe liver wind, inhibit liver yang and benefit the recovery of hemiplegic limb[9]. Of the three hand acupoints, Quchi (LI 11) and Hegu (LI 4) are Yangming Meridian (full of qi and blood) acupoints; Waiguan (TE 5), the Luo-Connecting acupoint of the Pericardium Meridian and one of the Eight Confluent Acupoints with the Yang Link Vessel, can circulate qi, alleviate pain, move blood and unblock collaterals. It isalso an experienced acupoint for post-stroke hemiplegia[10]. Of the three foot acupoints, Futu (ST 32) and Zusanli (ST 36) can supplement qi, invigorate blood and regulate meridians; full of yin blood and meridian qi, Taichong (LR 3) can clear liver heat by reducing manipulation and tonify liver yin by reinforcing manipulation[11].
The three needles for spasticity of the upper extremities are Jiquan (HT 1), Chize (LU 5) and Neiguan (PC 6). Needling Jiquan (HT 1, location: at the center of axillary fossa) can regulate meridian, activate the brachial plexus nerve and in turn enhance the repair of brain neurons. Chize (LU 5) is indicated for upper limb spasm, especially the spasm, stiffness and impaired movement of the elbows. Since the heart dominates mind and is protected by the pericardium from external pathogens, Neiguan (PC 6) is a key point for post-stroke mental illness and weakness of the hand/elbow. The three needles for spasticity of the lower extremities are Shuxi (Extra), Yinlingquan (SP 9) and Sanyinjiao (SP 6). Located in the inguinal region, Shuxi (Extra) connects the abdomen with lower extremities and is associated with the contraction of abdominal and thigh muscles[12]. Needling this point can relieve spasm and alleviate pain. Needling Yinlingquan (SP 9) close to the knee joint can alleviate spasm of the tendon and benefit joint motion. Needling Sanyinjiao (SP 6) can tonify the liver and kidney, regulate the spleen and stomach, circulate blood and unblock collaterals.
Results of this study showed that there were statistical differences in scores of NDS and SFFMA before and after 14-day treatment in both groups; a statistical differenc also appeared between 14-day treatment and 28-day treatment (P<0.05). There were inter-group statistical differences in scores of NDS and SFFMA after 28-day treatment (P<0.05), indicating that combined Jin’s three-needle with rehabilitation training and rehabilitation training alone can both enhance the recovery of nerve function in patients with post-stroke hemiplegia and improve their motor function; however, the former obtained a more remarkable effect.
Modifications of points on the basis of different stages, pathologic conditions and pattern identification enabled the Jin’s three-needle to be more flexible and directed at ‘disease’, ‘symptom’ and ‘syndrome’. Despite the good effect of Jin’s three-needle for post-stroke hemiplegia, this study only observed the 28-day therapeutic efficacy and lacked other observation indexes. As a result, it is impossible to assess the long-term and comprehensive efficacy of Jin’s three-needle for ischemic post-stroke hemiplegia. Due to the strict inclusion criteria involving the initial onset age, frequencies, primary diseases and drug combination, further research is needed for a better understanding.
[1] Fang XH. The present epidemic status and the influential elements of stroke in China. Zhongguo Nao Xueguan Bing Zazhi, 2004, 1(5): 233-237.
[2] Chinese Neuroscience Society, Chinese Neurosurgical Society. Key diagnostic points for cerebrovascular diseases. Zhonghua Shenjingke Zazhi, 1996, 29(6): 379-380.
[3] Collaborative Group of Acute Encephalopathy of State Administration of Traditional Chinese Medicine. Standard for diagnosis and therapeutic effect evaluation of stroke (trial). Beijing Zhongyiyao Daxue Xuebao, 1996, 19(1): 55-56.
[4] Nan DK. Rehabilitation Medicine. 3rd Edition. Beijing: People’s Medical Publishing House, 2004.
[5] Yun XP. Assessment of Rehabilitation Care. Beijing: Huaxia Press, 2005: 393-396.
[6] Yuan Q. Acupoints combination characteristics of Jin's triple acupuncture. J Acupunct Tuina Sci, 2007, 5(2): 65-67.
[7] Wang Y, Han W, Guo T. Clinical observations on the efficacy of Jin three needles in treating post-stroke hemiplegia. Shanghai Zhenjiu Zazhi, 2010, 29(10): 638-640.
[8] Xie Q, Zhuang LX, He J. Observations on the efficacy of Jin’s three-needle therapy for post-stroke shoulder-hand syndrome. Shanghai Zhenjiu Zazhi, 2011, 30(7): 462-463.
[9] Yuan Q. An Overall Picture of Jin Rui’s Acupuncture. Beijing: People’s Medical Publishing House, 2007: 50-51.
[10] Peng ZF. Jin’s Three-needle Therapy. Shanghai: Shanghai Scientific & Technical Publishers, 2000: 25-27.
[11] Shen XY. Science of Meridians and Acupoints. Beijing: China Press of Traditional Chinese Medicine, 2003: 58.
[12] Hu SY, Qian LL, Qin L. Relationship between foundation of inguinal morphological structure features and pain. Wuhan Tiyu Xueyuan Xuebao, 2002, 36(3): 49-50.
Translator: Han Chou-ping
R246.6
A
Date: May 10, 2013
Author: Zhou Zhao-hui, M.M., physician.
E-mail: zjtnyx@126.com
杂志排行
Journal of Acupuncture and Tuina Science的其它文章
- Clinical Observation on Acupoint Sticking Therapy for Lumbar Intervertebral Disc Hernination
- Clinical Observation on Electroacupuncture for Post-stroke Flaccid Paralysis
- Effect of Electroacupuncture on Anxiety and Craving in Heroin Addicts During Detoxification
- Clinical Study on Acupoint Injection for Primary Osteoporosis
- Treatment of Post-stroke Spastic Hemiplegia by Acupuncture plus Rehabilitation Training
- Immediate Effects of Hegu Needling on Adhesive Scapulohumeral Periarthritis
