Clinical Study on Acupuncture for Quality of Life in Patients with Age-related Macular Degeneration
2013-07-18XiaYongLiuRuiSunJingjinXinShienCuiHuashunLiuShimin
Xia Yong, Liu Rui, Sun Jing-jin, Xin Shi-en, Cui Hua-shun, Liu Shi-min
1 Acupuncture and Tuina College, Shanghai University of Traditional Chinese Medicine, Shanghai 201203, China
2 Eye and ENT Hospital of Fudan University, Shanghai 200031, China
3 Shuguang Hospital Affiliated to Shanghai University of Traditional Chinese Medicine, Shanghai 200021, China
Clinical Study on Acupuncture for Quality of Life in Patients with Age-related Macular Degeneration
Xia Yong1, Liu Rui2, Sun Jing-jin1, Xin Shi-en3, Cui Hua-shun3, Liu Shi-min1
1 Acupuncture and Tuina College, Shanghai University of Traditional Chinese Medicine, Shanghai 201203, China
2 Eye and ENT Hospital of Fudan University, Shanghai 200031, China
3 Shuguang Hospital Affiliated to Shanghai University of Traditional Chinese Medicine, Shanghai 200021, China
Objective: To observe the effect of acupuncture on the quality of life in patients with age-related macular degeneration (AMD).
Methods: A total of 47 dry AMD cases (94 eyes) were randomly allocated into three groups, 22 cases (44 eyes) in the acupuncture group, 15 cases (30 eyes) in the Western medicine group and 10 cases (20 eyes) in the control group. Cases in the acupuncture group were treated with acupuncture, cases in the Western medicine group with vitamin C and E and cases in the control group received no treatment except for out-patient follow-up.
Results: Acupuncture could significantly improve eye symptoms of dry AMD cases including blurred vision, drastic decrease in visual acuity, distorted vision, central scotomas, visual fatigue and dry eyes as well as other systemic symptoms related to macular degeneration.
Conclusion: Acupuncture can substantially improve the quality of life in patients with dry AMD.
Acupuncture Therapy; Age-related Macular Degeneration; Quality of Life
Age-related macular degeneration (AMD), also known as senile macular degeneration, is a major cause of blindness in older adults (>50 years)[1]. This condition is often associated with aging[2]and genetic factors[3-7]. AMD is a chronic eye condition that results in a drastic decrease in the center of the visual field (the macula), affecting one or both eyes and causing progressive visual impairment or even permanent blindness if left untreated. This study observed the impact of acupuncture on quality of life in AMD patients, using scores of eye symptoms and systemic symptoms of traditional Chinese medicine (TCM) as indexes.
1 Clinical Data
1.1 Diagnostic criteria
This is based on the diagnostic criteria for dry AMD stipulated by the Ocular Fundus Diseases Group, National Academy of Ophthalmology in 1986 and the criteria in theOphthalmology[8]. Aged above 50; significant decrease in visual acuity; macular changes such as depigmentation or pigmentary alterations, drusen, beaten-bronze appearance, atrophic spots; and absence of macular hemorrhage or fluorescence leakage.
1.2 Differential diagnosis
Peripheral drusen: Drusen is located outside the macular region (not inside).
Myopic degeneration: Other than atrophic changes in macular region,severe myopia is often accompanied by typical changes of optic nerve papilla and absence of drusen.
Central serous chorioretinopathy (CSC): Aged below 50, eminence of central serous retina, detachment of pigment epithelium, stippled atrophy of pigment epithelium and absence of drusen.
Hereditary macular degeneration: Aged below 50, absence of drusen and having a family history.
Toxic retinopathy: Poisoning by chloroquine can cause stippled depigmentation coupled with pigmentation (Bull’s eye maculopathy), absence of drusen and having a history of drug administration.
1.3 Inclusion criteria
Aged >50 and disease duration >4 months; willing to sign the informed consent and agreed to participate in this clinical study; and discontinued other therapies over 3 months before joining this study.
1.4 Exclusion and rejection criteria
Those who failed to meet the above inclusion criteria; having received other therapies that may affect evaluation of this study; having other medical conditions during the study; having incomplete data; failed to stick to the treatment protocol and failed to examine observation indexes according to the protocol.
1.5 Study subjects
Forty-seven cases (94 eyes) were recruited in the study from the outpatient departments of Shanghai Acupuncture and Meridian Research Institute and Shuguang Hospital Affiliated to Shanghai University of Traditional Chinese Medicine (eastern section) as well as Eye and ENT Hospital of Fudan University. These cases were grouped by a randomized, controlled and blinded clinical trial design. After signing the informed consent, they were randomly allocated into three groups, an acupuncture group of 22 cases (44 eyes), a Western medicine group of 15 cases (30 eyes) and a control group of 10 cases (20 eyes). During the clinical trial, the researchers, practitioners and statistical personnel were separated. There were no significant differences in general materials among the three groups (P>0.05), indicating that they were comparable (table 1).
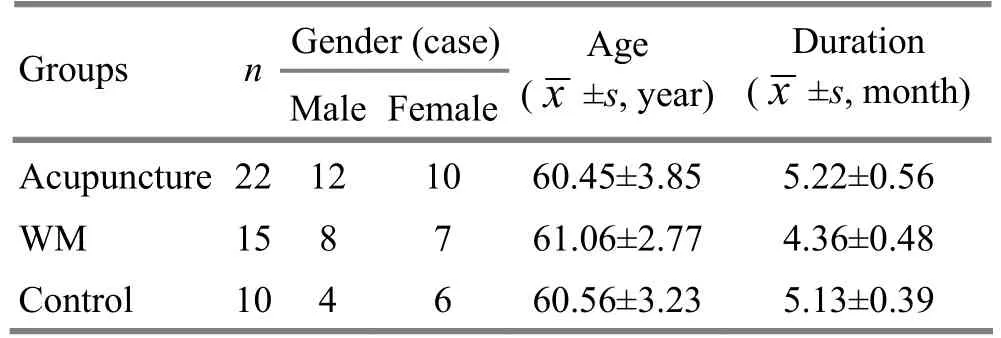
Table 1. Inter-group comparison of general materials
1.6 Statistical method
The SPSS 18.0 version software was used for statistical management, () for expression of measurement data, andQ-test was conducted.
2 Treatment Methods
2.1 Acupuncture group
Points: Jingming (BL 1), Shangming (Extra, locates at midpoint of the supraorbital arch), Neitongziliao [(Extra, locates at superior to the eyeball, lateral border between the eyeball and supraorbital wall and at the same level with Tongziliao (GB 1)], Jianming (Extra, locates at approximately 0.4 cun below the inner canthus), (Fig.1), Chengqi (ST 1), Qiuhou (EX-HN 7) and Taichong (LR 3). Jingming (BL 1), Shangming (Extra) and Neitongziliao (Extra) were used as one group of points; Jianming (Extra), Chengqi (ST 1) and Qiuhou (EX-HN 7) as another group, the two groups were used alternately, one group for each treatment).
Method: Locations of above points are based onNomenclature and Location of Acupuncture Points(GB/T 12346-2006)[9]. Stainless steel filiform needles of 0.25 mm in diameter and 40 or 50 mm in length were used for the treatment. Points around the eye socket were punctured 1.5-2 cun, coupled with mild lifting, thrusting and rotating manipulation until the appearance of an intense soreness and distension behind the eyeballs. Reducing manipulation by lifting, thrusting and rotating was applied to Taichong (LR 3) and other adjunct points. The needles were retained for 30 min. The treatment was done twice a week, 2 months for a course of treatment.
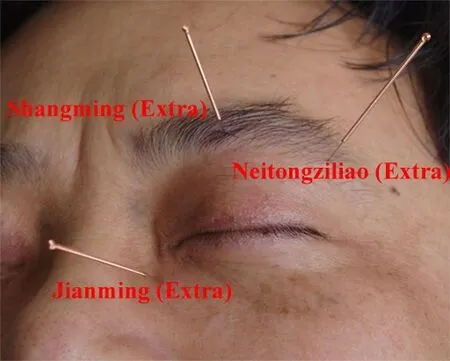
Fig.1 Periocular points
2.2 Western medicine group
Cases in Western medicine group took Vitamin C 0.2 g and Vitamin E 0.1 g for each dose, 3 doses a day, and 2 months for a course of treatment.
2.3 Control group
No intervention measures were taken in the control group except for 2-month outpatient follow-up.
3 Therapeutic Efficacy Observation
3.1 Observation indexes
3.1.1 Scoring of eye symptoms
The eye symptoms (blurred vision, drastic decrease in visual acuity, distorted vision, central scotomas, visual fatigue, seeing things in changed colors and dry eyes) were scored.
Method: For the first visit, each symptom was scored 3; after three months of treatment, unimproved symptoms remained 3, somewhat improvement scored 2, substantial improvement scored 1 and total absence of symptoms scored 0.
3.1.2 Scoring of TCM symptoms
The scoring method was same as that of eye symptoms.
3.2 Treatment results
3.2.1 Comparison of TCM symptoms among the three groups
After treatment, TCM symptoms in the acupuncture group were substantially improved, but not in the Western medicine group and the control group. This indicated that acupuncture obtained better overall effects than Western medicine (table 2).
3.2.2 Comparison of eye symptoms among the three groups
After treatment, except for seeing things in changed colors, other eye symptoms were significantly improved in the acupuncture group (P<0.05) but not in the Western medicine group and the control group (P>0.05). After treatment, except for seeing things in changed colors, there were significant differences between the acupuncture group and the other two groups (P<0.05) and there were no significant differences between the Western medicine group and control group (P>0.05), indicating that except for seeing things in changed colors, acupuncture obtained better effects than the other two in improving other eye symptoms (table 3).
Table 2. Inter-group comparison of TCM symptoms before and after treatment (, point)

Table 2. Inter-group comparison of TCM symptoms before and after treatment (, point)
Note: Intra-group comparison with score of before treatment, 1)P<0.05; compared with the results after treatment of the Western medicine group and the control group, 2)P<0.05
Tastelessness (no thirsty) 13 3.00±0.002.03±0.011)2)103.00±0.003.00±0.00 13 3.00±0.00 3.00±0.00 Thirsty with a desire to drink water 6 3.00±0.002.00±0.011)2)53.00±0.003.00±0.00 6 3.00±0.00 3.00±0.00 Dry stools 11 3.00±0.002.04±0.021)2)93.00±0.003.00±0.00 11 3.00±0.00 3.00±0.00 Poor memory 21 3.00±0.001.60±0.011)2)143.00±0.003.00±0.00 21 3.00±0.00 3.00±0.00 Dizziness 19 3.00±0.001.58±0.011)2)133.00±0.003.00±0.00 19 3.00±0.00 3.00±0.00 Headache 12 3.00±0.002.00±0.011)2)103.00±0.003.00±0.00 12 3.00±0.00 3.00±0.00 Lumbar and knee soreness/weakness 21 3.00±0.001.51±0.031)2)143.00±0.003.00±0.00 21 3.00±0.00 3.00±0.00 Poor appetite 18 3.00±0.001.78±0.011)2)133.00±0.003.00±0.00 18 3.00±0.00 3.00±0.00 Dry, bitter mouth 11 3.00±0.001.59±0.021)2)113.00±0.003.00±0.00 11 3.00±0.00 3.00±0.00 Frequent urination 20 3.00±0.001.00±0.011)2)133.00±0.003.00±0.00 20 3.00±0.00 3.00±0.00 Tinnitus 15 3.00±0.002.00±0.011)2)123.00±0.003.00±0.00 15 3.00±0.00 3.00±0.00 Insomnia 20 3.00±0.001.59±0.011)2)133.00±0.003.00±0.00 20 3.00±0.00 3.00±0.00 Dream-disturbed sleep 17 3.00±0.001.43±0.021)2)103.00±0.003.00±0.00 17 3.00±0.00 3.00±0.00 Palpitations 12 3.00±0.002.31±0.011)2)123.00±0.003.00±0.00 12 3.00±0.00 3.00±0.00 Gastric distension 9 3.00±0.002.42±0.011)2)53.00±0.003.00±0.00 9 3.00±0.00 3.00±0.00 Hot drink preference 8 3.00±0.002.49±0.011)2)83.00±0.003.00±0.00 8 3.00±0.00 3.00±0.00 Loose stools 8 3.00±0.002.49±0.011)2)73.00±0.003.00±0.00 8 3.00±0.00 3.00±0.00 Spontaneous sweating 15 3.00±0.001.99±0.011)2)103.00±0.003.00±0.00 15 3.00±0.00 3.00±0.00 Sallow face 13 3.00±0.002.22±0.011)2)113.00±0.003.00±0.00 13 3.00±0.00 3.00±0.00 Night sweats 9 3.00±0.002.42±0.011)2)93.00±0.003.00±0.00 9 3.00±0.00 3.00±0.00 Low back pain 14 3.00±0.002.04±0.021)2)113.00±0.003.00±0.00 14 3.00±0.00 3.00±0.00
Table 3. Inter-group comparison of eye symptoms before and after treatment (, point)

Table 3. Inter-group comparison of eye symptoms before and after treatment (, point)
Note: DVD=Drastic vision decrease; STCC=Seeing things in changed colors; intra-group comparison with score of before treatment, 1)P<0.05; compared with the results after treatment of the Western medicine group and the control group, 2)P<0.05
Acupuncture group Western medicine group Control group Items Affected eyes Before treatment After treatment Affected eyes Before treatment After treatment Affected eyes Before treatment After treatment Blurred vision 44 3.00±0.00 2.00±0.031)2)30 3.00±0.002.90±0.0420 3.00±0.003.00±0.00 DVD 32 3.00±0.00 1.00±0.011)2)25 3.00±0.003.00±0.0016 3.00±0.003.00±0.00 Distorted vision 10 3.00±0.00 1.00±0.021)2)8 3.00±0.003.00±0.006 3.00±0.003.00±0.00 Central scotomas 32 3.00±0.00 1.00±0.011)2)20 3.00±0.003.00±0.0014 3.00±0.003.00±0.00 Visual fatigue 36 3.00±0.00 1.00±0.021)2)30 3.00±0.003.00±0.0018 3.00±0.003.00±0.00 STCC 8 3.00±0.00 2.50±0.03 6 3.00±0.003.00±0.004 3.00±0.003.00±0.00 Dry eyes 24 3.00±0.00 1.00±0.011)2)18 3.00±0.003.00±0.0012 3.00±0.003.00±0.00
3.3 Adverse events during treatment
During treatment, 10 of 22 cases (male/female ratio=1:9) in the acupuncture group experienced bleeding and hematoma in the orbital region, no adverse events occurred in the Western medicine group and the control group.
4 Discussion
Common symptoms of AMD cases include blurred vision, dramatic decrease in visual acuity, distorted vision, central scotomas, visual fatigue, seeing things in changed colors and dry eyes. According to this clinical study, after treatment, acupuncture could substantially improve eye symptoms except for seeing things in changed colors and thus increased the patients’ quality of life. Patients came with the help of a family member for the first visit due to severe eye discomfort but could come independently after a period of treatment.
Seeing things in changed colors means an inability to distinguish normal colors. It is similar to color blindness or weakness and has always been an intractable eye condition. This clinical study has shown that acupuncture didn’t work well for seeing things in changed colors. Further research is still needed in this aspect.
Since visual function is closely associated with Zang-Fu organs and meridians, we’ve also observed other systemic symptoms related to macular degeneration such as headache, dizziness, poor memory, poor appetite, dry bitter mouth, dry stools, frequent urination and lumbar and knee soreness/weakness. After treatment, the above symptoms in the acupuncture group were substantially improved compared with the Western medicine group and the control group. This indicates that acupuncture can obtain better overall effects for AMD.
Normal functions of the eyes rely on qi nourishment of the five Zang and six Fu organs. Of points selected in this clinical study, Jingming (BL 1) is a major local point for eye problems with its distinctive effects of unblocking collaterals and sharpening the eyes. Chengqi (ST 1) activates qi and blood and is also a major point for eye problems. Other local points, Shangming (Extra), Neitongziliao (Extra), Jianming (Extra) and Qiuhou (EX-HN 7), were combined to circulate qi and blood around the eyes. Taichong (LR 3) was used for systemic regulation[10-14].
Due to increased vascular fragility and longer clotting time in elderly females, acupuncture may easily cause bleeding and hematoma. As a result, it should be cautious in needling points around the orbit in those patients[15].
[1] Gu H, Liu NP. Progress in genetic studies of age-related macula degeneration. Zhonghua Yanke Zazhi, 2012, 48(2): 176-178.
[2] Xu D, Cai YS. Biology of free radicals and pathomechanism of eye tissue injury. Foreign Medical Science (Section of Ophthalmology), 1997, (3): 131-133.
[3] Yoshida A, Yoshida M, Yoshida S, Shiose S, Hiroishi G, Ishibashi T. Familial cases with age-related macular degeneration. Jpn J Ophthalmol, 2000, 44(3): 290-295.
[4] Yu J, Wu LZ, Xu L. Preliminary study of mitochondrial DNA deletions in age-related macular degeneration. Yanke Xuebao, 1997, 13(2): 52-55.
[5] Allikmets R, Shroyer NF, Singh N, Seddon JM, Lewis RA, Bernstein PS, Peiffer A, Zabriskie NA, Li Y, Hutchinson A, Dean M, Lupski JR, Leppert M. Mutation of the Stargardt disease gene (ABCR) in age-related macular degeneration. Science, 1997, 277(5333): 1805-1807.
[6] Bernstein PS, Leppert M, Singh N, Dean M, Lewis RA, Lupski JR, Allikmets R, Seddon JM. Genotype-phenotype analysis of ABCR variants in macular degeneration probands and siblings. Invest Ophthalmol Vis Sci, 2002, 43(2): 466-473.
[7] Kliffen M, Lutgens E, Daemen MJ, de Muinck ED, Mooy CM, de Jong PT. The APO*E3-Leiden mouse as an animal model for basal laminar deposit. Br J Ophthalmol, 2000, 84(2): 1415-1419.
[8] Hui YN. Ophthalmology. 6th edition. People’s Medical Publishing House, 2004: 176-177.
[9] General Administration of Quality Supervision, Inspection and Quarantine of the People’s Republic of China, Standardization Administration of the People’s Republic of China. Nomenclature and Location of Acupuncture Points (GB/T 12346-2006). Standards Press of China, 2006.
[10] Zhang B, Peng L, Zhou LZ, Mu JP, Cheng JM. Observation on the therapeutic efficacy of moxibustion and acupoint injection in treating optic atrophy. Shanghai Zhenjiu Zazhi, 2012, 31(11): 833-834.
[11] Zhang CH, Zhang LL, Ma XP, Yang L, Hong J, Liu J, Wu LX. Research on acupuncture-moxibustion for dry eye syndrome. J Acupunct Tuina Sci, 2013, 11(2): 72-78.
[12] Tao XY, Ru K, Lang S, Zhu WL, Fu J, Chen J, Ye C, Tao Y, Li Y, Yu YH. Observations on the efficacy of acupuncture at periocular extraordinary points in treating juvenile myopia. Shanghai Zhenjiu Zazhi, 2010, 29(10): 643-644.
[13] Guo MH, Cui EC, Li XY, Zong L. Diverse needling methods for dry eye syndrome: a randomized controlled study. J Acupunct Tuina Sci, 2013, 11(2): 84-88.
[14] Ren H. Observations on the efficacy of point injection in treating 76 acquired abducent paralysis patients. Shanghai Zhenjiu Zazhi, 2008, 27(1): 11-12.
[15] Xia Y, Shu S, Li Y, Liu SM, He JS. Therapeutic effect and side effect of treatment on hyperthyroid exophthalmos with the combination of acupuncture and medication. Zhongguo Zhenjiu, 2010, 30(10): 806-809.
Translator: Han Chou-ping
R246.82
A
Date: August 15, 2013
Author: Xia Yong, M.D., associate professor
Liu Shi-min, M.D., associate professor.
E-mail: liusmin@sina.com
杂志排行
Journal of Acupuncture and Tuina Science的其它文章
- Shu-Stream Points for Two Cases with Time-related Disease
- Therapeutic Observation on Swift Needling with Fire Needle plus Medication for Herpes Zoster
- Tuina Is Superior to Electroacupuncture in Treating Thoracic Facet Joint Disorder
- Clinical Study on Electroacupuncture for Cervical Intervertebral Disc Herniation
- Therapeutic Efficacy Observation on Combining Herbal Cake-partitioned Moxibustion with Plumblossom Needle Therapy for Cervical Radiculopathy
- Clinical Observation on Acupuncture Therapy for Depression at Perimenopause
