Superoxide dismutase activity and malondialdehyde levels in patients with travel-induced psychosis
2012-07-10YiGONGRuolianZHAOBaochunYANG
Yi GONG*, Ruolian ZHAO, Baochun YANG
Superoxide dismutase activity and malondialdehyde levels in patients with travel-induced psychosis
Yi GONG*, Ruolian ZHAO, Baochun YANG
Background:Oxidative stress is a neurotoxic factor that may precipitate acute psychoses.
Aim:Assess the relationship of travel-induced psychosis and oxidative stress.
Methods: Twenty-one inpatients with travel-induced psychosis related to prolonged train travel were evaluated using the Brief Psychiatric Rating Scale (BPRS) at the time of admission and their plasma superoxide dismutase (SOD) activity and malondialdehyde (MDA) concentrations were assessed on the morning following admission. These assessments were repeated after the psychotic symptoms resolved, which typically occurred after 2-6 days of low-dose antipsychotic treatment. The SOD and MDA results in the patients were compared to those of 21 normal age and gender matched control subjects.
Results:At admission the patient group had significantly higher SOD activity and MDA concentrations than the control group. After resolution of the psychotic symptoms the BPRS scores, SOD activity, and MDA concentrations all showed significant declines but the SOD activity and MDA concentrations remained higher than in the matched control group. At admission there was a non-significant positive correlation of the BPRS total score with SOD activity (r=0.32, p=0.164) and with MDA concentration (r=0.34, p=0.126). The before versus after drop in the BPRS total score was weakly correlated with the drop in the SOD activity (r=0.28, p=0.217) and with the drop in the MDA concentration (r=0.29, p=0.211).
Conclusion:These findings suggest that the neurotoxic effects of oxidative stress are directly related to the development of travel-induced psychosis. This may be relevant to the understanding of other acute psychotic states such as schizophrenia.
1. Introduction
Travel-induced psychosis is a relatively common condition in China that is primarily seen in individuals who have experienced prolonged travel in very crowded trains. It was first classified as a distinct diagnosis in 1998 in the second revised edition of theChinese Classification and Diagnostic Criteria of Mental Disorders(CCMD-2-R),[1]at which time it was called ‘transient mental disorder.’Then a few years later in the third edition of the Chinese classification system[2]it was renamed ‘travel-induced psychosis’ and its diagnostic criteria were specified. The primary clinical symptoms listed included disturbances of consciousness, fragmentary delusions, hallucinations and bizarre behavior. During the acute development of travel-induced psychosis the individual experiences disturbances of perception, thought and affect that can be associated with potentially serious behavioral disturbances such as attacking others, jumping from moving vehicles, and so forth. The reported incidence of travel-induced psychosis in China is 8.1 per 1000 population, which is higher than the incidence of schizophrenia (1-1.5 per 1000).[3]Given the professional interest in this condition, there are several studies of travel-induced psychosis reported in China. But there are very few such studies from other countries, presumably because it is not listed as a distinct diagnosis in either the 10thedition of theInternational Classification of Diseases(ICD-10)[4]or the 4thedition of theDiagnostic and Statistical Manual of Mental Disorders(DSM-IV).[5]In these diagnostic systems such cases would be classified as acute transient psychoses.
Wu and colleagues[6]identified five risk factors for travel-induced psychosis (in order of importance): increased in-vehicle CO2concentration, the unavailability of seating (requiring long periods of standing), long travel times, introversion, and first experience of traveling by train. Despite the central focus on the causative role of CO2concentration, there are currently no studies about oxidative stress in such patients. These adverse traveling environments, particularly if prolonged over severaldays, could trigger disordered oxygen metabolism, acidic metabolite accumulation and cerebral hypoxia, leading to the accumulation of dopamine and excitatory amino acids in the striatum, hippocampus, and other cerebral structures, and to the production of neurotoxic metabolites such as free radicals.[7]The excess of radicals could then cause oxidative damage to brain cell lipids and induce transient mental disorders.[8]Parallel studies about oxidative stress in schizophrenia,[9]report that the development of acute psychotic symptoms in patients with schizopohrenia is closely related to oxidative stresses, as indicated by elevated erythrocyte superoxide dismutase (SOD) activity (which reflects the level of oxygen radicals in the plasma) and malondialdehyde (MDA) concentrations (a metabolite of lipid peroxidation that reflects the degree of somatic cell damage).
The current study compares these measures of oxidative stress (SOD and MDA) between normal control subjects and individuals with travel-induced psychosis and assesses changes in these measures in the patients as their acute psychotic symptoms resolve.
2. Subjects and methods
2.1 Subjects
2.1.1 Patients with travel-induced psychosis
As shown in Figure 1, twenty-one individuals with travel-induced psychosis admitted to the Kunming Mental Hospital from November 2009 to June 2010 were enrolled in the study. All 21 individuals developed psychotic symptoms during a prolonged trip by train. They included 13 men and 8 women with a mean (sd) age of 32.3 (7.3) years. On admission they had been suffering from travel-induced psychosis — based on the criteria specified in the third edition of theChinese Classification and Diagnostic Criteria of Mental Disorders[2](CCMD-3) — for one to two days. None of them had a family history of mental disorders, none had used psychoactive substances (alcohol, marijuana, heroin, etc.), and none of them had neurological or other chronic illnesses. All of them had persecutory delusions or other delusional thinking; 17 had auditory hallucinations; and9 had disturbed consciousness. During the onset of the condition 12 had injured other passengers and 9 had injured themselves.

Figure 1. Flowchart of the study
Consent for treatment (and for participation in the study) was obtained from relatives or guardians who were usually contacted by phone (because they lived in distant locations). All subjects were treated with lowdose antipsychotic medication: six received haloperidol (10 mg/d), eight received quetiapine (100–200 mg/d), and seven received risperidone (2 mg/d). Nine patients also received adjunctive treatment with clonazepam (2 mg/d) and seven received adjunctive treatment with estazolam (4 mg/d). The mean (sd) duration of antipsychotic treatment was 6.2 (7.2) days. The mean duration of psychotic symptoms (including the time prior to admission) was 3.6 (1.3) days. All patients recovered social functioning and insight within six days of treatment and were subsequently discharged.
2.1.2 Control subjects
Twenty-one healthy volunteers who signed written informed consent to participate in the study were recruited from among students at the Kunming School of Medicine (n=16) and workers at the Kunming Mental Hospital (n=5) and were 1-to-1 matched for gender and age with members of the patient group. They included 13 males and 8 females and had a mean (sd) age of 33.0 (9.5) years. None of them had a family history of mental illness.
2.2 Methods
2.2.1 Blood sample collection
All patients were admitted within hours of leaving the train where the psychotic symptoms started and a fasting blood sample (5 ml) was collected from the basilic vein of each subject between 7:00 am and 7:30 am the following morning, that is, less than 24 hours after leaving the train. Control subjects also had a fasting blood sample drawn at 7:00 am to 7:30 am. Ethylene diamine tetraacetic acid (EDTA) was added in the sample to prevent coagulation. After centrifugation (2500 g, 5 min), the serum layer was collected and kept at -40 °C for subsequent analysis. After recovery from the psychotic symptoms another plasma sample was collected in the same manner from individuals in the patient group.
2.2.2 Oxidative stress determination
Serum MDA concentration and SOD activity were assayed by modified 2-thiobarbituric acid (TBA) spectrophotometry and the xanthine oxidase method as described in the instructions for the commercial kits (Nanjing Jiancheng Bioengineering Institute, Nanjing, Jiangsu, China).[10,11]Each assay included three parallel samples.
2.2.3 Evaluation of severity of psychotic symptoms
The psychotic symptoms of individuals in the patient group were rated by clinical psychiatrists using the Brief Psychiatric Rating Scale[12](BPRS) on the day of admission and a second time on the same day as the second blood draw.
2.3 Statistical analysis
Data were analyzed by paired t-tests and repeatedmeasures two-way analysis of variance (ANOVA) using the SPSS 11.5 statistical package (SPSS, Chicago, IL, USA). The relationship of the duration of psychotic symptoms, of the first and second BPRS, SOD and MDA measures, and of the before versus after change in BPRS, SOD and MDA measures were assessed using Spearman’s ranked correlation coefficients. Given the relatively small number of patients (n=21) we chose to consider correlation coefficients with an absolute value of 0.30 or greater (which corresponded to a p-value <0.20) as potentially important.
3. Results
As shown in Table 1, the MDA concentration and SOD activity of individuals with travel-induced psychosis in the morning after admission were significantly higher than those in age and gender matched control subjects. Re-evaluation a few days later after the acute psychotic symptoms had resolved showed a significant drop in the BPRS total score, in the SOD activity and in the MDA concentration. However, the MDA concentration and SOD activity remained significantly higher in the patients than in the matched controls.
Table 2 shows the ranked correlations of the various measures collected during the study. The total duration of psychotic symptoms — which is one measure of severity — was not significantly associated with any of the biochemical measures, but it was negatively correlated at the trend level with the post-treatment total BPRS score and with the magnitude of the pre-post change in SOD activity. The total BPRS score at admission was positively correlated at the trend level with the admission SOD activity, with the admission MDA concentration and with the magnitude of the pre-post change in MDA concentration. The post-treatment total BPRS score was not correlated with any of the SOD or MDA measures but the magnitude of the pre-post drop in BPRS total score was positively correlated at the trend level with both the pre-treatment and post-treatment measures of SOD activity and MDA concentration. And the SOD activity at admission and the magnitude of the change in the SOD activity both had significant positive correlations with the admission, post-treatment and pre-post change in MDA concentration.
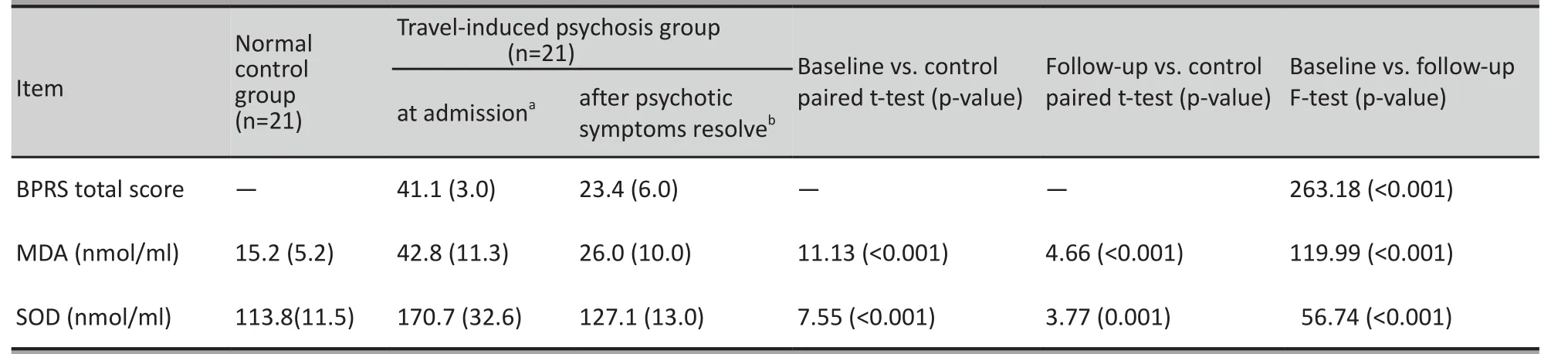
Table 1. Comparison of BPRS scores, MDA concentration and SOD activity between controls and cases (before and after treatment) and before and after treatment in patients with travel-induced psychosis (mean [sd])
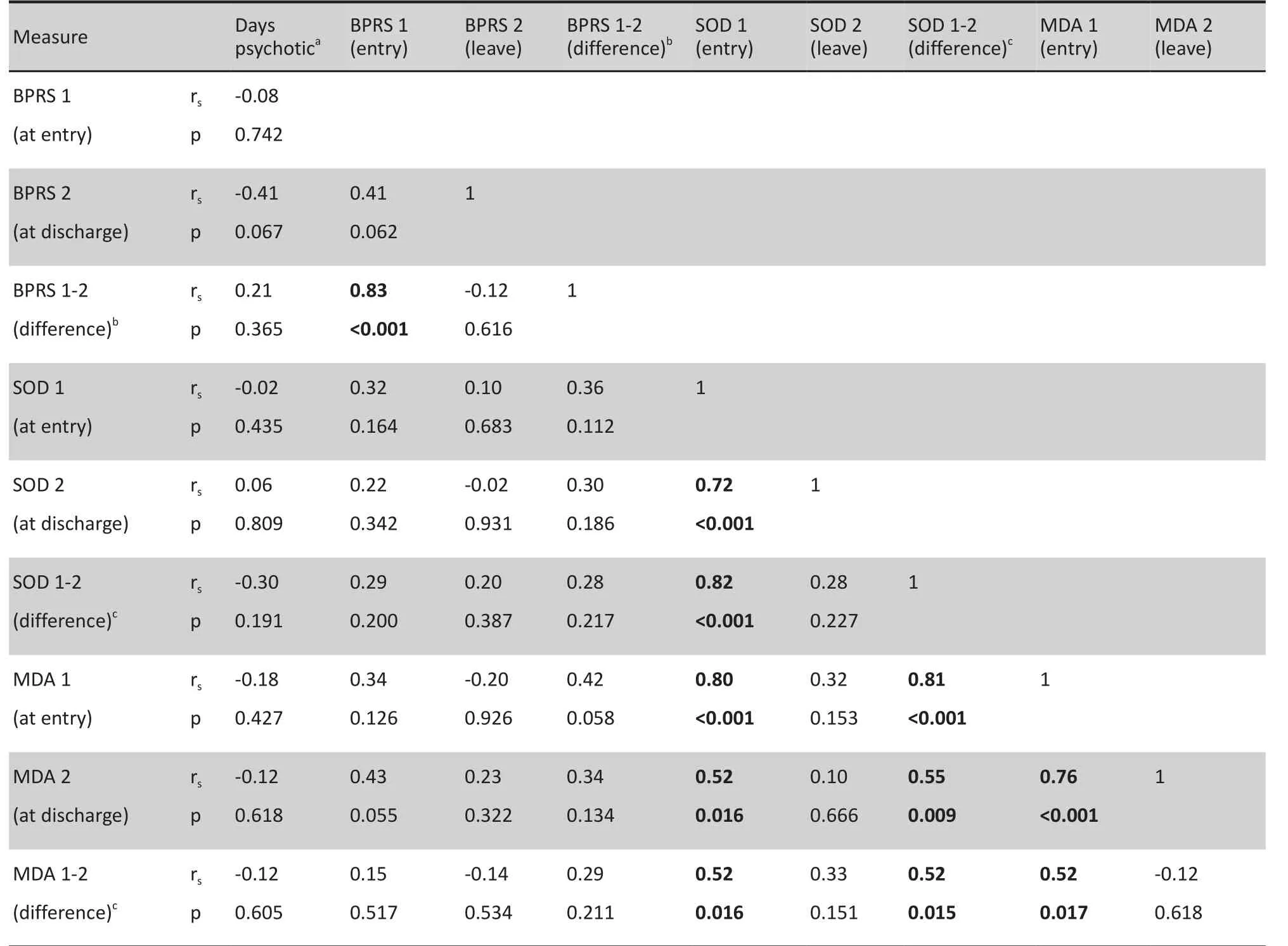
Table 2. Ranked correlation of clinical measures and oxidative stress measures before and after treatment in 21 patients with travel-induced psychosis
4. Discussion
4.1 Main findings
We find that individuals with travel-related psychosis have significantly higher plasma SOD activity and MDA concentrations than control subjects, suggesting a causative role of abnormalities in oxygen radical and anti-oxidative functions. The increased plasma SOD activity in patients is, presumably, attributable to an enhanced enzymatic defense response to the elevated oxygen radical levels.[13-15]The increased serum MDA concentration indicates accumulation of lipid peroxides reflecting increased somatic cell damage by radicals.[16]After a few days of low-dose antipsychotic treatment, the BPRS scores, SOD activity, and MDA concentration all decreased significantly. These changes are consistent with earlier observations[17]that MDA concentration changes were closely related to improvement in psychotic symptoms. The antipsychotics may block dopamine receptors and, thus, prevent radical formation and the subsequent peroxidation damage by radicals. Reduction of such neurotoxic factors facilitates neuron repair, alleviating the associated psychotic symptoms.
In the current study the relationship between the severity of psychotic symptoms (as measured by BPRS) and the SOD and MDA measures was moderate. On admission the rank correlation coefficients of BPRS total scores with SOD activity and MDA concentration ranged from 0.15 to 0.43; and the correlation of the magnitude of the pre-post change in BPRS scores with the magnitude in the change of the SOD and MDA measures ranged from 0.28 to 0.34. However, these correlations did not reach statistical significance, presumably because of the relatively small sample size.
Re-assessment of the biochemical measures, after the psychotic symptoms resolved, found that despite a substantial improvement the SOD and MDA levels in the patient group remained significantly different from the normal controls. This suggests the persistence of oxidative stress (or of the markers of oxidative stress) for prolonged periods even after removal from the toxic environment. Further studies are needed to assess the duration of these abnormalities after acute episodes of psychosis.
4.2 Limitations
Several issues limited our analyses of these cases of travel-induced psychosis. The main problem is that the small number of cases limited our power to identify important relationships and increased the likelihood of type II errors (e.g., only correlations larger than 0.45 were statistically significant). And most patients wanted to be discharged and return to their distant homes immediately after resolution of their psychotic symptoms so it was not possible to continue monitoring the patients until their SOD and MDA measures returned to normal. Given the urgency of treating the acute psychotic symptoms in the patient group it was also not possible to determine the extent to which antipsychotic medications were responsible for the resolution of symptoms; the changed environment after the individual leaves the train may have been the major factor in the rapid resolution of symptoms. Moreover, the lack of precision in the estimates of the time of onset of the psychotic symptoms and the variability in the time between leaving the train (the environment in which the symptoms occurred) and the first blood draw made it impossible to compose a clear time line for the cases, which may have introduced uncontrolled biases in the analysis. And we did not adjust for smoking history which may have influenced the SOD and MDA measures.
4.3 Significance
Despite these limitations the results comparing SOD activity and MDA concentrations in patients with travelinduced psychosis to age and matched controls are very robust. The evidence that travel-induced psychosis is associated to the neurotoxic effects of oxidative stress is quite strong but not yet definitive because the direct causal pathway has not yet been elaborated.
These findings have implications for our understanding of other types of acute psychosis, including the acute exacerbations of psychotic symptoms that occur in schizophrenia. Expansion of the dopamine hyperactivity hypothesis for schizophrenia to include a consideration of radicals has stimulated a new wave of studies about the role of oxidative stress in the development and manifestations of schizophrenia. The symptoms during the acute phase of travel-induced psychosis are quite similar to those seen during acute episodes of schizophrenia, suggesting that psychotic symptoms associated with schizophrenia may also be related to the neurotoxicity of oxygen radicals. Based on this hypothesized relationship there would be value in testing the utility of adjunctive treatment of acute episodes of positive symptoms of schizophrenia (and acute travel-related psychosis) with radical scavengers such as vitamin C, vitamin E and mannitol.
Conflict of interest
The authors report no conflict of interest related to this manuscript
Funding
The study was funded by the Kunming Mental Hospital.
1. Ministry of Health of China.Chinese Classification and Diagnostic Criteria of Mental Disorders. 2nd ed, Revised. Beijing: 1998. (in Chinese)
2. Chinese Society of Psychiatry, Chinese Medical Association.Chinese Classification and Diagnostic Criteria of Mental Disorders. 3rd ed. Jinan: Shandong Science and Technology Press, 2001. (in Chinese)
3. Yang C, Zhao HQ, Gao ZQ. Research progress of travel psychosis..Journal of International Psychiatry2010; 37(3): 189-190. (in Chinese)
4. World Health Organization.ICD-10 Classifications of Mental and Behavioural Disorder: Clinical Descriptions and Diagnostic Guidelines. Geneva: World Health Organisation, 1992.
5. American Psychiatric Association.Diagnostic and Statistical Manual of Mental Disorders. 4th ed. Washington, DC: American Psychiatric Association, 1994.
6. Wu WY, Geng L, Lu Z, Zhang YZ, Li CB, Liu DY, et al. A summing up analysis of travelling psychosis.Chin J Psychiatry1997; 30(2): 95-99. (in Chinese)
7. Abdalla DSP. Superoxide dismutase and glutathione peroxidase activities in schizophrenic and manic-depressive patient.Clinical Chemistry1986; 2(32): 805.
8. Wang HL. The importance of free radicals and thier enzyme defense systems to mental health.Journal of International Psychiatry1990; 12(17): 69. (in Chinese)
9. Yu YF, Zhang X, Li J, Tang HY, Li SJ, Liu XX. Measurement of plasma superoxide dismutase activity and malondialdehyde concentration in schizophrenia.Chin J Nerv Men Dis1997; 23(6): 347. (in Chinese)
10. Zhang FX. Factors that affect the xanthine oxidase method for assessing serum superoxide dismutase activity.Yunan Medicine2001; 2(6):32. (in Chinese)
11. Chen HZ. Thiobarbituric acid assay to assess lipid peroxidation.Central China Medicine2002; 3(3):62. (in Chinese)
12. Zhang MY.Handbook of Evaluation Scales in Psychiatry. Changsha: Hunan Science and Technology Press, 2003: 81-94; 94-111. (in Chinese)
13. Hou XY, Zhang GY. Mechanisms underlying dopaminergic neurotoxicity in ischemic cerebral damage.Progress in Physiological Science1999; 30(4): 315-316. (in Chinese)
14. Michelou Am.Clinical use of superoxide dismutase and possible pharmacological approaches. London: Academic Press, 1982: 278.
15. Wang HL, Gao BL, Cui Z, Jiang Q, Shi JA, Sun J. A study on content of blood CuZn-superoxide dismutase relationship with various mental diseases.Chin J Neurology1994; 6(27): 6. (in Chinese)
16. Fang YZ.Free radical and enzyme. Beijing: Science Press, 1989: 226. (in Chinese)
17. Yuan GZ, Huang YP, Yao JJ, Li X, Yu HY. A study of the blood superoxide dismutase level in schizophrenia and affective disorder patients.Chin J Psychiatry2001; 34(3): 150-152. (in Chinese)
背景氧化应激是一种神经毒性因素,可能会促使急性精神病的发生。
目的评估旅途精神病(travel-induced psychosis)与氧化应激的关系。
方法对乘坐长途火车诱发的 21 例旅途精神病住院患者,在其入院时采用简明精神病评定量表(Brief Psychiatric Rating Scale, BPRS)评定精神症状,入院次日清晨测定其血清超氧化物歧化酶(super oxide dlsmutase,SOD)活性和丙二醛(malondialdehyde,MDA)含量;待患者精神病性症状缓解后(通常为小剂量抗精神病药治疗后 2~6天),再次进行上述检测。选取性别、年龄匹配的 21 名健康志愿者为对照组,比较患者与对照者的血清SOD活性和MDA含量。
结果入院时患者的血清SOD活性和MDA含量均高于对照组。精神症状缓解后,患者的BPRS评分、血清SOD活性和MDA含量均显著下降,但后两者仍高于对照组。入院时患者的BPRS总分与SOD活性呈正相关(r=0.32,p=0.164),与MDA含量也呈正相关(r=0.34, p=0.126),但均无统计学意义。治疗后BPRS总分的下降与SOD活性的下降弱相关(r=0.28,p=0.217),也与MDA含量的下降也呈弱相关(r=0.29,p=0.211)。
结论研究结果提示,氧化应激的神经毒性作用与旅途精神病的发生直接相关。这或许能够帮助我们理解其他急性精神病性障碍(如精神分裂症)的发生。
旅途精神病患者血清超氧化物歧化酶活性及丙二醛水平
龚毅* 赵若连 杨保春
昆明市精神病院,云南昆明
*通信作者:15925202082@139.com
2011-08-31; accepted: 2012-05-02)
10.3969/j.issn.1002-0829.2012.03.005
Kunming Mental Hospital, Kunming, Yunnan Province, China
* Correspondence: 15925202082@139.com
猜你喜欢
杂志排行
上海精神医学的其它文章
- Consultation-liaison psychiatry in China
- Retrospective analysis of treatment effectiveness among patients in Mianyang Municipality enrolled in the national community management program for schizophrenia
- Effectiveness of a rehabilitative program that integrates hospital and community services for patients with schizophrenia in one community in Shanghai
- Randomized controlled trial on adjunctive cognitive remediation therapy for chronically hospitalized patients with schizophrenia
- Cross-sectional study on the relationship between life events and mental health of secondary school students in Shanghai, China
- How to avoid missing data and the problems they pose: design considerations