Randomized controlled trial on adjunctive cognitive remediation therapy for chronically hospitalized patients with schizophrenia
2012-07-10HongboLUYuyingLIFengLIXinyiJIAOWenSHIKanglinGUOPengfeiLIU
Hongbo LU*, Yuying LI, Feng LI, Xinyi JIAO, Wen SHI, Kanglin GUO, Pengfei LIU
Randomized controlled trial on adjunctive cognitive remediation therapy for chronically hospitalized patients with schizophrenia
Hongbo LU1*, Yuying LI1, Feng LI1, Xinyi JIAO2, Wen SHI1, Kanglin GUO1, Pengfei LIU1
Background:Cognitive remediation therapy (CRT) is one of the promising new non-drug approaches to reducing cognitive deficits of patients with schizophrenia that has not yet been fully evaluated in China.
Aim:Assess the efficacy of CRT in improving the cognitive functioning, social functioning and insight of patients with chronic schizophrenia.
Methods:126 clinically stable inpatients with chronic schizophrenia were randomly allocated to an intervention group (with CRT) and a treatment as usual group (TAU) (which used standard occupational and recreational therapy methods). The treatment frequency and duration were the same for the two groups: five times per week for three months. The Wisconsin Card Sorting Test (WCST) was used to evaluate before versus after changes in cognitive function, the Scale of Social Skills of chronic schizophrenia Inpatients (SSSI) was used to assess social functioning, and the Insight and Treatment Attitude Questionnaire (ITAQ) was use to assess insight.
Results:Four patients dropped out during the study leaving 60 in the CRT group and 62 in the TAU group in the final analysis. Both groups showed significant improvement in WCST measures over the three-month trial but the improvement in the CRT group was significantly greater than that for the TAU group on all of the WCST measures assessed. The total SSSI score improved significantly in both groups over the three months, but the improvement in the two groups was not significantly different. The total ITAQ score also showed significant improvement in both groups over the three months and the degree of improvement was significantly greater in the CRT group than in the TAU group.
Conclusions:As an adjunctive treatment to antipsychotic medication, a three month course of CRT is more effective at improving the cognitive functioning and insight of hospitalized patients with chronic schizophrenia than routine occupational and recreational therapy.
1. Introduction
Schizophrenia is a severe mental illness with unknown etiology, poor prognosis and a high disability rate. There are no proven preventive measures[1,2]but several medications can treat the clinical symptoms of the disorder. Deficits in cognition, social functioning and insight into the illness often occur but there are few effective interventions for dealing with these components of the illness. In an attempt to simultaneously address the clinical symptoms and the cognitive and social deficits, newer therapeutic approaches to schizophrenia have combined psychopharmacology and different types of cognitive therapies. Cognitive remediation therapy (CRT) is one of the promising new non-drug therapies[2]that specifically focuses on the cognitive deficits commonly seen in schizophrenia. The current study assesses the efficacy of the CRT paradigm[3,4]developed by Ann Delahunly and Rodney Morice in the treatment of the cognitive deficits, social dysfunction and lack of insight of patients with chronic schizophrenia in China.
2. Subjects and Methods
2.1 Subjects
The enrollment of patients is shown in Figure 1. Patients admitted to the Third People’s Hospital of Lanzhou Municipality from March to December 2010 for acute relapses were screened for participation in the study after they completed 2-4 weeks of treatment for their acute symptoms. Individualseligible for participation in the study met diagnostic criteria for schizophrenia (based on the third edition of theChinese Classification and Diagnostic Criteria of Mental Disorders[5]), had a duration of illness of at least five years, were clinically stable at the time of enrollment (i.e., total score of Positive and Negative Syndrome Scale[6][PANSS] <60 or a drop in the total PANSS score of more than 50% after initial treatment of acute symptoms), were 18-65 years of age, and were receiving maintenance treatment with a combination of clozapine and risperidone (the most common combined treatment regimen for chronic patients in our setting). Excluded patients included those with co-morbid mental retardation, perceptual disorders, organic brain disease, serious medical disorders, impulse control problems, or severe depressive or anxiety symptoms, and those who were pregnant or lactating. All participating patients and their guardians signed informed consent for the study.
The 126 eligible patients were randomly assigned to a CRT group or to a treatment as usual (TAU) group. The 63 patients in the CRT group included 40 men and 23 women with a mean (sd) age of 37 (8) years who had a mean duration of formal schooling of 11 (5) years, and a mean duration of illness of 23 (9) years. At the time of enrollment in the study their mean total PANSS score was 45.3 (13.1) and they were all receiving combined treatment with clozapine (mean dose of 278 [121] mg/d) and risperidone (mean dose of 3.4 [1.4] mg/d).
The 63 patients in the TAU group included 37 men and 26 women with a mean age of 38 (9) years who had a mean duration of formal schooling of 10 (4) years and a mean duration of illness of 24 (8) years. At the time of enrollment in the study their mean total PANSS score was 46.2 (13.6) and they were all receiving combined treatment with clozapine (mean dose of 285 [126] mg/d) and risperidone (mean dose of 3.9 [1.2] mg/d).
None of the subjects changed the dosage of antipsychotic medication over the three months of the study. There were no statistically significant differences in the gender, age, years of education, duration of illness, total PANSS score on enrollment, or dosage of medication between the two groups.
2.2 Intervention
The CRT employed in this study used a Chinese version of the CRT manual[3,4]developed by Ann Delahunly and Rodney Morice. CRT is a comprehensive neuropsychological training method targeting various major cognitive deficits of schizophrenia that combines verbal reinforcement, errorless learning, individualized guidance and other cognitive therapeutic techniques. The cognitive functioning of patients in three primary areas—cognitive flexibility, working memory and planning—is improved as they complete cognitive tasks of increasing difficulty under the guidance of four trainedtherapists.[7-10]Training sessions lasted for 45 minutes each and were repeated five days a week for three months.
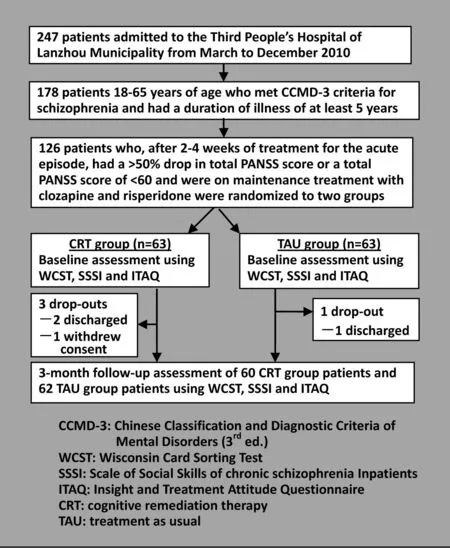
Figure 1. Flowchart for the study
2.3 Instruments
The Wisconsin Card Sorting Test[11](WCST) was used to evaluate before versus after changes in cognitive function, the Scale of Social Skills of chronic schizophrenia Inpatients[12](SSSI) was used to assess social functioning, and the Insight and Treatment Attitude Questionnaire[13](ITAQ) was used to assess insight. Five outcome measures were assessed for the WCST: total number of completed cards; number of cards correctly categorized, number of perseverative errors, number of random errors, and number of categories completed. SSSI is an interviewer-rated questionnaire developed in China specifically for chronic psychiatric inpatients with 10 items (score on 0-2 point Likert scales) that have good internal consistency (alpha=0.89), test-retest reliability (rs=0.97), and inter-rater reliability (rs=0.98);[12]the total score (range 0-20) is used in the current study, with lower scores representing better functioning. The ITAQ is an interviewer-rated scale with 11 items (scored on 0-2 point scales) that have good internal consistency (alpha=0.91),[14]test-retest reliability (r=0.87),[14]and inter-rater reliability (Kappa=0.86);[15]the total score (range 0-22) is used in this analysis, with higher scores representing better insight. Two psychologists were trained to administer these instruments; their interrater reliability for the three instruments was assessed by comparing their results for 15 patients (ICC for WCST=0.80, ICC for SSSI=0.87, and ICC for ITAQ=0.92). These psychologists were not blind to the treatment status of the patients they evaluated.
2.4 Statistical analysis
All data were analyzed using SPSS 17 statistical software. Paired t-tests were used to compare before versus after results within groups, independent-sample t-tests were used to compare baseline scores in the two groups and F-tests were used to compare differences in the magnitude of the changes between the two groups over the three-months of treatment (adjusting for baseline values).
The study was approved by the Institutional Review Board of the Third People’s Hospital of Lanzhou Municipality.
3. Results
During the 3-month course of the study three patients dropped out of the CRT group (two were discharged and one withdrew consent) and one patient who was discharged dropped out from the TAU group. As shown in Table 1 the CRT group had significant improvements in all five measures derived from the WCST over the three-month trial but TAU only showed significantimprovement in one of the five measures (total number of completed cards). The improvements in these WCST measures in the CRT group were significantly greater than those in the TAU group.

Table 1. Mean (sd) scores for different WCST measures before treatment and after three months of treatment in the two groups
As shown in Table 2, the ITAQ total score improved significantly in both groups over the treatment period and the improvement in the CRT group was significantly greater than that in the TAU group. The SSSI total score also improved significantly over the three months in both groups; the magnitude of improvement in the SSSI total score was greater in the CRT group than in the TAU group but this difference did not reach statistical significance (p=0.074).
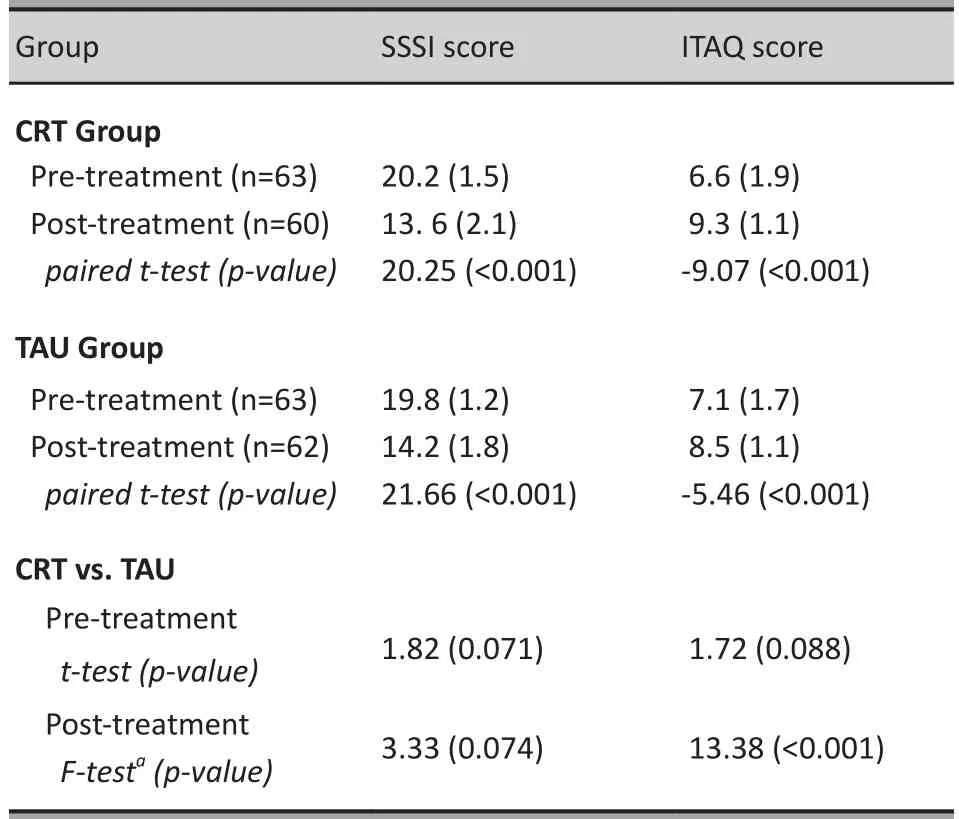
Table 2. Mean (sd) SSSI and ITAQ total scores before treatment and after three months of treatment in the two groups
4. Discussion
4.1 Main findings
Similar to studies in other countries,[16]we found that adjunctive treatments focused on cognitive functioning, social functioning and insight for inpatients with chronic schizophrenia can significantly improve objective measures of their functioning. Three months of non-specific standard occupational and recreational therapy combined with routine mental health education sessions (‘treatment as usual’) also had significant beneficial effects on social functioning and insight but had limited effects on cognitive functioning. The manualized cognitive remediation therapy intervention employed in this study resulted in a significantly greater improvement in executive functioning and in insight than was seen with TAU.
Both treatment groups had significant improvements in social functioning over the three months of treatment but the improvement in the CRT group, though larger than in the TAU group, was not significantly better than that in the TAU group. One possible reason for the lack of significant group differences with the SSSI is the difficulty of assessing social functioning in schizophrenia,[17,18]particularly in inpatient settings where the range of social skills that can be assessed is quite limited.
Several important questions remain to be answered by subsequent studies. Are the greater improvements seen with CRT persistent over time or would prolongation of the treatments beyond three months result in a decrease (or increase) in the differential outcomes for TAU and CRT? How long are the improvements sustained after a course of treatment: do patients need to have continuous CRT or ‘booster sessions’ of CRT to sustain their improvements in cognition, social functioning and insight? And do outpatients with schizophrenia experience similar improvements with CRT to those seen in these inpatients?
4.2 Limitations
Several limitations need to be considered when evaluating these results. The evaluation of outcomes was not done blindly so it is difficult to be certain that there was no bias in the evaluations. The WCST only assesses one component of cognitive functioning (executive functioning) so other measures would need to be used to more comprehensively assess cognitive functioning. All patients involved in the study were inpatients with chronic schizophrenia, so the improvement in cognitive functioning and insight found may not be relevant for outpatients or for patients with a relatively short duration of illness.
4.3 Significance
This randomized controlled trial provides clear evidence of the benefits of a three-month course of CRT as an adjunctive treatment for patients with chronic schizophrenia who have been hospitalized following an acute relapse of illness. Further study is needed to determine whether or not CRT should be continuously or intermittently provided to hospitalized patients. Other studies with outpatients are needed to determine whether or not the benefits identified with Chinese inpatients with schizophrenia would also be seen in community-based patients.
Conflict of interest
The authors report not conflict of interest related to this study.
Funding
The study was supported by the Third People’s Hospital of Lanzhou Municipality.
1. Ye FY. Effectiveness of psychosocial interventions in the rehabilitation of schizophrenia.China Foreign Medical Treatment2010; 29(23): 62. (in Chinese)
2. Lecardeur L, Stip E, Giguere M, Blouin G, Rodriguez JP, Champagne-Lavau M. Effects of cognitive remediation therapies on psychotic symptoms and cognitive complaints in patients with schizophrenia and related disorders: a randomized study.Schizophr Res2009; 111(1-3): 153-158.
3. Tan SP, Zou YZ, Jin Z, Qu Y, Yang FD, Xiao GR, et al. Cognitive remediation therapy can renormalize brain activation related to working memory in patients with schizophrenia: a functional magnetic resonance imaging study.Chin J Psychiatry2007; 40(1): 19-23. (in Chinese)
4. Qu Y, Xiao GR, Ma YH, Qi YG, Xu SL, Zhang JH, et al. Effects of cognitive remediation therapy on improving clinical symptoms and social functions in patients with chronic schizophrenia.Journal of Clinical Rehabilitative Tissue Engineering Research2007; 11(52): 10553-10556. (in Chinese)
5. Chinese Society of Psychiatry, Chinese Medical Association.Chinese Classification and Diagnostic Criteria of Mental Disorders. 3rd ed. Jinan: Shandong Science and Technology Press, 2001. (in Chinese)
6. Kay SR, Opler LA, Fiszbein A. The Positive and Negative Syndrome Scale (PANSS) for schizophrenia.Schizophr Bull1987; 12: 261-276.
7. Pfammatter M, Junghan UM, Brenner HD. Efficacy of psychological therapy in schizophrema: conclusions from meta-analyses.Schizophr BulI2006; 32 (Suppl 1): S64-S80.
8. Wexler BE, BelI MD. Cognitive remediation and vocational rehabilitation for schizophrenia.Schizophr Bull2005; 31(4): 931-941.
9. Hogarty GE, Greenwald DP, Eack SM. Durability and mechanism of effects of cognitive enhancement therapy.Psychiatr Serv2006; 57(12): 1751-1757.
10. Wykes T, Huddy V, Cellard C, McGurk SR, Czobor P. A metaanalysis of cognitive remediation for schizophrenia: methodology and effect sizes.Am J Psychiatry2011; 168(5): 472-485.
11. Liu ZN. Clinical use of the Wisconsin Card Sorting Test.Foreign Medical Sciences (Section of Psychiatry)1999; 26(1): 6-9. (in Chinese)
12. Guo GY. Reliability and validity of the scale of social skills of chronic schizophrenia in-patients.Chin J Nerv Ment Dis1995; 28(1): 16-18. (in Chinese)
13. McEvoy JP, Apperson LJ, Appelbaum PS, Ortlip P, Brecosky J, Hammill K, et al. Insight in schizophrenia. Its relationship to acute psychopathology.J Nerv Ment Dis1989; 177: 43-47.
14. Zhang JX, Li XB, Weng Z, Liu JT, Liu XC, Yuan W, et al. Clinical use of Insight and Treatment Attitude Questionnaire.Shandong Archives of Psychiatry1994; 4(1): 10-13. (in Chinese)
15. Liu HQ, Zhang PY, Shang L, Yang PD, Wu HW. Insight in schizophrenia: Use of the Insight and Treatment Attitude Questionnaire.Shanghai Arch Psychiatry1995: 7(3): 158-161. (in Chinese)
16. Wykes T, Spaulding WD. Thinking about the future cognitive remediation therapy-what works and could we do better?Schizophr Bull2011; 37(Suppl 2): S80-90.
17. Green MF, Nuechterlein KH, Gold JM, Barch DM, Cohen J, Essock S, et al. Approaching a consensus cognitive battery for clinical trials in schizophrenia: the NIMH-MATRICS conference to select cognitive domains and test criteria.Biol Psychiatry2004; 56(5): 301-307.
18. Deppen P, Sarrasin Bruchez P, Dukes R, Pellanda V, Vianin P. Cognitive remediation program for individuals living with schizophrenia (Recos): preliminary results.Encephale2011; 37(4): 314-321.
(received: 2011-09-13; accepted: 2012-02-08)
背景认知矫正治疗(Cognitive Remediation Therapy,CRT)是一种很有希望的、新的非药物治疗方法,能够减少精神分裂症患者的认知缺损。但未在国内得到充分的验证。
目的探讨认知矫正治疗对慢性精神分裂症患者认知功能、社会功能及自知力的疗效。
方法将126例病情相对稳定的慢性精神分裂症住院患者随机分成干预组和对照组。干预组接受行认知矫正治疗,对照组接受常规的工娱治疗,两组在治疗频度和治疗持续时间一致,均为每周5次,共3个月。于治疗前及治疗末分别采用威斯康星卡片分类测验(Wisconsin Card Sorting Test,WCST)评估认知功能 ,采用住院慢性精神分裂症患者社会功能评定量表(Scale of Social Skills of chronic schizophrenia Inpatients,SSSI)评估社会功能以及采用自知力与治疗态度问卷(Insight and Treatment Attitude Questionnaire,ITAQ)评估自知力。
结果研究过程中有 4 例患者脱落,干预组 60 例、对照组 62 例最终进入结果分析。治疗 3 个月后,两组的WCST测评结果均较治疗前显著改善,而干预组的WCST各指标的改善均比对照组明显。两组在 3 个月治疗后的SSSI总分均显著改善,但改善程度在两组间无显著性差异;两组的ITAQ总分也均有提高,但干预组的改善程度比对照组更明显。
结论在药物治疗的基础上,为期3个月的认知矫正治疗对改善慢性精神分裂症住院患者的认知功能及自知力比常规的工娱治疗更为有效。
慢性精神分裂症住院患者辅以认知矫正治疗的随机对照研究
吕红波1* 李玉英1李峰1焦歆益2师雯1郭康林1刘鹏飞1
1兰州市第三人民医院,甘肃兰州
2甘肃省监狱管理局兰州医院,甘肃兰州
*通信作者: hongbolv0308@126.com
roup
routine occupational and recreational therapy and general mental health education including instructor-led music therapy, dance therapy and physical exercises as well as psychological counseling during daily ward rounds. This treatment also lasted 45 minutes per day and was provided five days per week for three months. The four therapists who provided CRT were different from the clinicians who provided TAU.
10.3969/j.issn.1002-0829.2012.03.004
1The Third People’s Hospital of Lanzhou Municipality, Lanzhou, Gansu Province, China
2Lanzhou Hospital, Gansu Province Prison Administration, Lanzhou, Gansu Province, China
*Correspondence: hongbolv0308@126.com
猜你喜欢
杂志排行
上海精神医学的其它文章
- Consultation-liaison psychiatry in China
- Retrospective analysis of treatment effectiveness among patients in Mianyang Municipality enrolled in the national community management program for schizophrenia
- Effectiveness of a rehabilitative program that integrates hospital and community services for patients with schizophrenia in one community in Shanghai
- Superoxide dismutase activity and malondialdehyde levels in patients with travel-induced psychosis
- Cross-sectional study on the relationship between life events and mental health of secondary school students in Shanghai, China
- How to avoid missing data and the problems they pose: design considerations