A new technique for the reconstruction of complex portal vein anomalies in right lobe living liver donors
2012-07-07OnurYaprakNecdetGulerCemBalciMuratDayangacTolgaDemirbasRefikKilliYamanTokatandYildirayYuzer
Onur Yaprak, Necdet Guler, N Cem Balci, Murat Dayangac, Tolga Demirbas, Refik Killi, Yaman Tokat and Yildiray Yuzer
Istanbul, Turkey
New Techniques
A new technique for the reconstruction of complex portal vein anomalies in right lobe living liver donors
Onur Yaprak, Necdet Guler, N Cem Balci, Murat Dayangac, Tolga Demirbas, Refik Killi, Yaman Tokat and Yildiray Yuzer
Istanbul, Turkey
Living donor liver right lobe transplantation using donors with variation of the right sectorial portal vein is considered a challenging procedure in terms of the donor's safety and the complexity of reconstruction in the recipient. We describe an innovative technique to reconstruct double portal vein orifices via a deceased donor iliac vein graft.The postoperative course of the recipient was uneventful. Doppler ultrasound on the fourth postoperative month revealed equivalent flow in both portal vein branches. Reconstruction of double right portal vein branches using a cryopreserved iliac vein is a valuable technique for utilizing right lobe grafts with challenging portal vein anatomy.
liver transplantation; living donor; portal vein variations; venous plasty
Introduction
Living donor liver transplantation is being performed more frequently in countries with a limited cadaveric organ supply. A right liver lobe graft is preferred to a left lobe graft because of its volume advantage despite the vascular and biliary variations that occur more frequently in the right lobe. The incidence of portal venous variations is between 10% and 35% in different series.[1-3]It is not uncommon to create two orifices in the donor for anastomosis of the portal vein, if an associated anatomic variation exists. Several methods have been described for the anastomosis of two portal venous orifices to the recipient. Among these, back-wall plasty combining two orifices to one and graft interposition either with excision of the recipient portal vein or using a cadaveric iliac vein are the most commonly used techniques.[4,5]Patients with complex portal venous anomalies are usually not considered as donors because the distance and the angle between anterior and posterior branches of the portal vein challenges the reconstruction.[6]In this report, we describe an innovative approach to venous plasty reconstruction technique by using deceased donor iliac vein grafts in portal vein variations.
Surgical technique
A 62-year-old woman with the diagnosis of HCV cirrhosis was admitted to our hospital for right lobe living donor liver transplantation. The MELD score was 17 and the liver function status was Child C. The donor was her 33-year-old son. Volumetric CT angiography revealed a right lobe of 714 g and the estimated graft weight to recipient body weight ratio was 1.05. The donor anterior segment of the right portal vein originated from the left portal vein (Fig. 1). During the donor operation, the parenchyma was initially dissected, thereafter, the right biliary duct, right hepatic artery and right anterior- posterior portal vein branches were transected 3 mm above the confluence. The graft was taken to the back-table and perfused with HTK solution. The diameters of the anterior and posterior portal vein orifices were 9 and 7 mm, respectively (Fig. 2). The distance between the two orifices was 14 mm,and the outer distance was 30 mm. In our method, two cryopreserved cadaveric iliac vein grafts were used to reconstruct the double orifices. We used the first graft to preserve the physiologic angle between the two orifices. The second graft however was an interposition graft which was used to include the two orifices like a funnel. A cryopreserved cadaveric iliac vein was irrigated and dilated with physiologic saline. The upper 3 cm portion of the iliac vein was removed and incised in its long axis to create an elliptical patch. Two oval holes were created on the patch to accommodate the corresponding portal vein orifices. The anterior and posterior portal vein orifices were anastomosed to the holes in the patch using continuous 7.0 polypropylene sutures with the preservation of anterior and posterior portal veins in their original places. Separately, a 5-cm segment of iliac vein was anastomosed circumferentially to the elliptical patch with the end-to-side technique using continuous 7.0 polypropylene sutures. The diameter of the second graft was adjusted to the outer distance of the two orifices which measured 3 cm (Fig. 3).
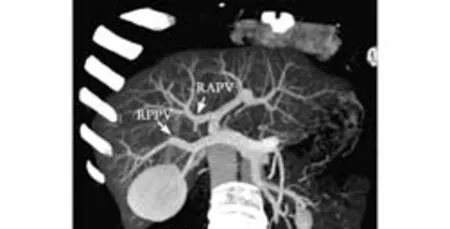
Fig. 1. CT angiography of the donor reveals common trunk of the right anterior sectoral branch and the left portal vein representing a portal vein anomaly. RAPV: right anterior portal vein; RPPV: right posterior portal vein.

Fig. 2. Back-table image of the graft shows two portal vein orifices that are distant from each other.
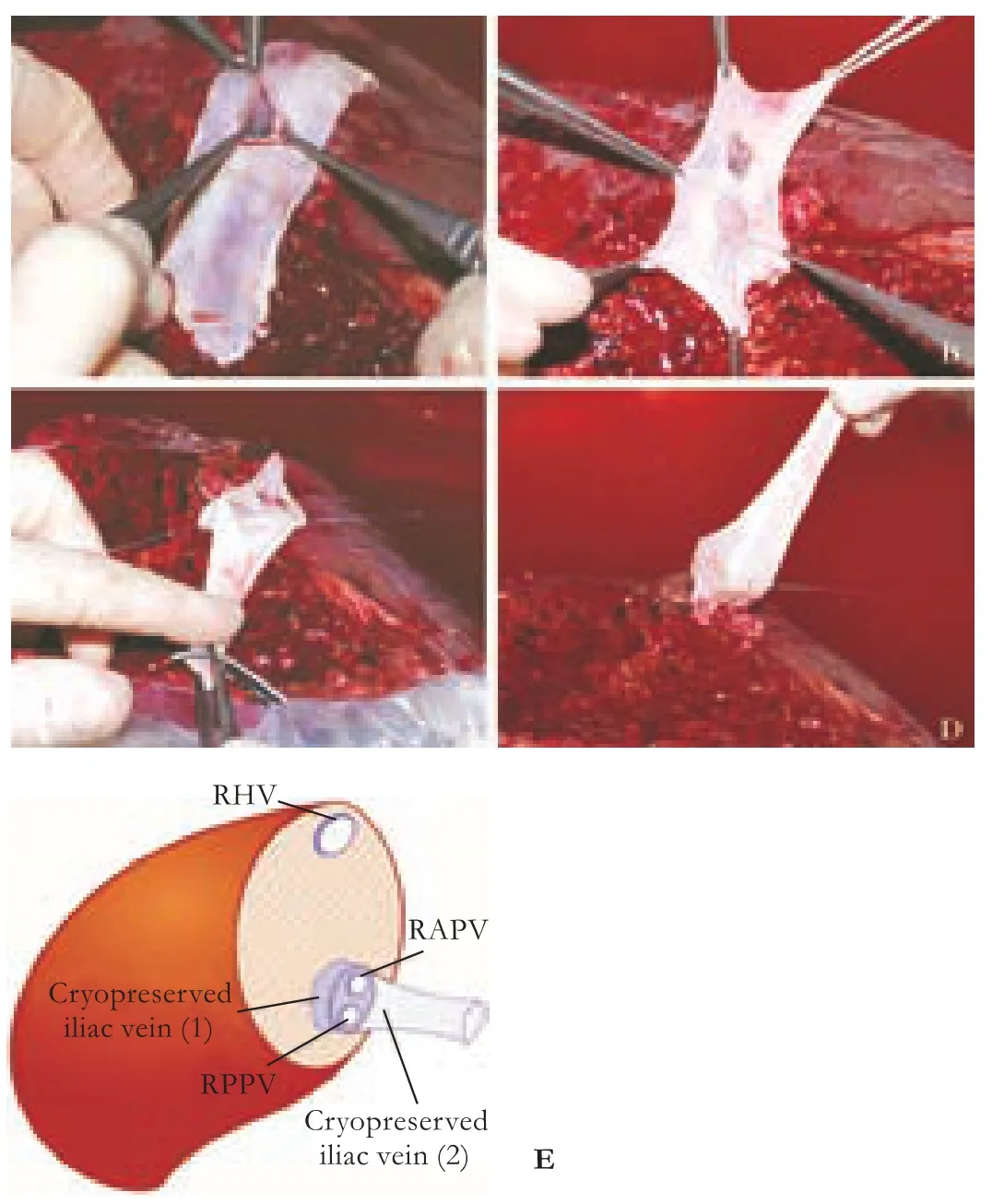
Fig. 3. Portoplasty technique at the back-table. A: Two oval holes are created on the patch to accommodate the corresponding portal vein orifices. B: The anterior and posterior portal vein orifices are anastomosed to the existing holes in the patch. C: Circumferential anastomosis is performed between the patch and another 5-cm iliac vein graft segment. D: The portoplasty is completed. E: The portoplasty technique is illustrated. RHV: right hepatic vein; RAPV: right anterior portal vein; RPPV: right posterior portal vein.

Fig. 4. A: End-to-end portal vein anastomosis between the reconstructed graft portal vein and the recipient portal vein is performed. B: After reperfusion, uneventful portal vein inflow.
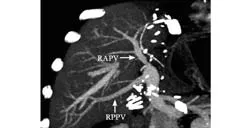
Fig. 5. CT angiography on postoperative day 15 shows normal intraluminal contrast enhancement of the sectorial right portal vein branches. RAPV: right anterior portal vein; RPPV: right posterior portal vein.
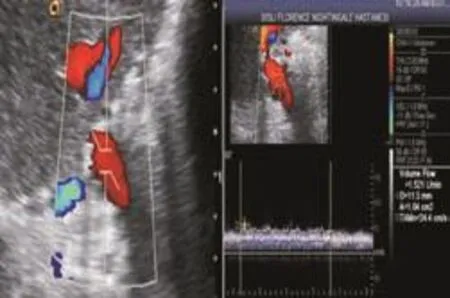
Fig. 6. Doppler ultrasound four months after transplantation reveals sufficient portal venous flow in right portal vein sectorial branches.
After completion of the anastomoses and reperfusion of the graft at the recipient (Fig. 4), intraoperative Doppler ultrasound was performed showing uninterrupted hepatopedal portal venous inflow in both sectorial branches. Daily Doppler ultrasonography and CT angiography on postoperative day 7 revealed patent portal venous inflow (Fig. 5). The patient was discharged uneventfully on postoperative day 15. Doppler ultrasound was performed four months after transplantation and revealed excellent portal inflow in the main portal vein and right portal vein sectorial branches with the following values: main portal vein volume, 1500 mL/min, and velocity 55 cm/sec; right anterior portal vein volume 834 mL/min and velocity 60.2 cm/sec; right posterior portal vein volume 720 mL/min and velocity 87 cm/sec (Fig. 6).
Discussion
Eligible donor availability is a crucial step in living donor liver transplantation. Blood group mismatch, age, insufficient graft and/or remnant liver lobe volumes, and hepatosteatosis of the graft, all require exclusion of the candidate from donation. Sometimes, a donor with anatomical variations is the only alternative to provide a graft, therefore, utilization of donors with anatomic variations should be considered if there is the shortage of more suitable donors. Considering the incidence of portal venous anomalies is as high as 25% in any population, new reconstruction techniques may help to recruit more donor candidates for the procedure.
Portal vein anomalies are classified into four categories: single left and right lobe division of the portal vein is type 1, trifurcation of the anteriorposterior segments of the right portal vein with the left portal vein is type 2, and early segmentation of the right posterior branch of the portal vein is type 3. If the anterior sectorial branch of the right portal vein arises from the left portal vein, the anomaly is type 4.[6]
In grafts with two portal vein orifices, both portal vein branches have to be anastomosed to the recipient. The risk of portal venous thrombosis increases if the orifices of the portal vein branches are anastomosed separately. Therefore, reconstruction of the portal vein segments with a graft to combine both sectorial branches becomes the method of choice.
Asan's group made a discoid excision on the anterior and posterior branches of the donor portal vein and repaired this vein by creating a venoplasty. However, this is an additional procedure, which may impact donor safety. Another technique has been described by the same group as end-to-end anastomosis of the donor portal vein after excision of the anterior and posterior sectorial branches.[6]In recent years, Y-graft portoplasty has been the preferred reconstruction technique and is derived either from the recipient portal vein or a cadaveric iliac vein.[6,7]However, the following drawbacks may be expected with this technique: 1) both native portal venous and cadaveric iliac vein grafts have the risk of size and angle mismatch between the donors segmental portal vein branches and the vascular graft; 2) if the Y-graft is derived from the native portal vein, additional risks may occur such as partial thrombus in the vascular graft, increased wall thickness of the portal vein secondary to cirrhosis, and challenging dissection due to previous surgical and interventional procedures in the native liver; and 3) if present, preexisting hepatocellular cancer in the native liver may threaten the vascular graft.
In patients with type 2 portal venous anatomic variation, the back-wall plasty reconstruction procedure is the most frequently used alternative. However, backwall plasty is created at the back-table, once the graft is reperfused, so the sectorial branch orifices can lose their original shape and may lead to hemodynamically impaired inflow. If the distance between anterior and posterior right portal venous branches is too long (type 3) to create a plasty, a U-graft can be used as described by Xu et al.[8]The U-graft has the disadvantage ofshort distance between the anastomosis and the inner wall of the loop, which may cause resistance to portal venous inflow. No technique has been described to reconstruct type 4 portal venous variations. The reconstruction technique we describe in this report can create uneventful graft perfusion by preserving the native physiological angles of the anterior and posterior portal sectorial branches. We believe this reconstruction technique may even be considered in type 4 portal venous anatomy.
In conclusion, we describe a new reconstruction technique for the anastomosis of the sectorial right portal vein branches in patients with complex right portal venous anomalies. This method may be used in challenging portal venous anatomic variations and may decrease the number of rejected donors.
Contributors:YO and YY proposed the study. GN, DM, DT, KR and TY collected the data. YO and BNC wrote the first draft. All authors contributed to the design and interpretation of the study and to further drafts. YY is the guarantor.
Funding:None.
Ethical approval:Not needed.
Competing interest:No benefits in any form have been received or will be received from a commercial party related directly or indirectly to the subject of this article.
1 Marcos A, Orloff M, Mieles L, Olzinski A, Sitzmann J. Reconstruction of double hepatic arterial and portal venous branches for right-lobe living donor liver transplantation. Liver Transpl 2001;7:673-679.
2 Cheng YF, Huang TL, Lee TY, Chen TY, Chen CL. Variation of the intrahepatic portal vein; angiographic demonstration and application in living-related hepatic transplantation. Transplant Proc 1996;28:1667-1668.
3 Akgul E, Inal M, Soyupak S, Binokay F, Aksungur E, Oguz M. Portal venous variations. Prevalence with contrast-enhanced helical CT. Acta Radiol 2002;43:315-319.
4 Hwang S, Lee SG, Ahn CS, Kim KH, Moon DB, Ha TY, et al. Technique and outcome of autologous portal Y-graft interposition for anomalous right portal veins in living donor liver transplantation. Liver Transpl 2009;15:427-434.
5 Sugawara Y, Makuuchi M, Tamura S, Matsui Y, Kaneko J, Hasegawa K, et al. Portal vein reconstruction in adult living donor liver transplantation using cryopreserved vein grafts. Liver Transpl 2006;12:1233-1236.
6 Lee SG, Hwang S, Kim KH, Ahn CS, Park KM, Lee YJ, et al. Approach to anatomic variations of the graft portal vein in right lobe living-donor liver transplantation. Transplantation 2003;75:S28-32.
7 Thayer WP, Claridge JA, Pelletier SJ, Oh CK, Sanfey HA, Sawyer RG, et al. Portal vein reconstruction in right lobe living-donor liver transplantation. J Am Coll Surg 2002;194: 96-98.
8 Xu M, Yan L, Zhao J, Li B, Wen T, Zeng Y, et al. U-graft anastomosis for anomalous portal venous branching reconstruction in right lobe living donor liver transplantation. Liver Transpl 2007;13:1062-1064.
(Hepatobiliary Pancreat Dis Int 2012;11:438-441)
October 28, 2011
Accepted after revision January 5, 2012
Author Affiliations: Hepatobiliary and Organ Transplant Center, Florence Nightingale Hospital, Istanbul, Turkey (Yaprak O, Guler N, Dayangac M, Demirbas T, Killi R, Tokat Y and Yuzer Y); Department of Radiology, Bilim University, Istanbul, Turkey (Balci NC)
Onur Yaprak, MD, Florence Nightingale Hastanesi, Organ Nakil Merkezi, Abide-i Hurriyet Cad. No: 164. 34381, Sisli/Istanbul, Turkey (Tel: 90-212-2258398; Fax: 90-212-2240356; Email: onuryaprak@ hotmail.com)
© 2012, Hepatobiliary Pancreat Dis Int. All rights reserved.
10.1016/S1499-3872(12)60205-7
杂志排行
Hepatobiliary & Pancreatic Diseases International的其它文章
- Gastric- and intestinal-type marker expression in invasive ductal adenocarcinoma of the pancreas
- Early changes of hepatic hemodynamics measured by functional CT perfusion in a rabbit model of liver tumor
- A common variant in the precursor miR-146a sequence does not predispose to cholangiocarcinoma in a large European cohort
- Muscarinic acetylcholine receptor M3 in proliferation and perineural invasion of cholangiocarcinoma cells
- Hepatocyte differentiation of mesenchymal stem cells
- Early control of short hepatic portal veins in isolated or combined hepatic caudate lobectomy
