Characteristics of vascular lesions in patients with posterior circulation infarction according to age and region of infarct*☆
2012-01-04DaopeiZhangShulingZhangHongtaoZhangYumingXu
Daopei Zhang, Shuling Zhang, Hongtao Zhang, Yuming Xu
1 Third Department of Neurology, Zhengzhou People’s Hospital, Zhengzhou 450003, Henan Province, China
2 Third Department of Neurology, First Affiliated Hospital, Zhengzhou University, Zhengzhou 450052, Henan Province, China
Characteristics of vascular lesions in patients with posterior circulation infarction according to age and region of infarct*☆
Daopei Zhang1, Shuling Zhang1, Hongtao Zhang1, Yuming Xu2
1Third Department of Neurology, Zhengzhou People’s Hospital, Zhengzhou 450003, Henan Province, China
2Third Department of Neurology, First Affiliated Hospital, Zhengzhou University, Zhengzhou 450052, Henan Province, China
Patients with posterior circulation infarction underwent CT angiography and magnetic resonance angiography. Intracranial and extracranial vasculopathy was evaluated according to age group and location of stroke. Patients aged >60 years and <60 years had similar rates of vertebral artery dominance and vertebrobasilar artery developmental or origin anomalies. Vertebrobasilar artery stenosis or occlusion and tortuosity occurred more frequently in patients aged >60 years than <60 years. The rates of vertebrobasilar artery anomalies and tortuosity were high in patients with posterior circulation infarction. Vertebrobasilar artery tortuosity occurred more frequently in patients aged >60 years, whereas vertebrobasilar artery developmental anomalies occurred with similar frequency in patients aged <60 years and >60 years. Patients with infarction of the brainstem or cerebellum were more likely to have vertebral artery stenosis or occlusion, basilar artery stenosis or occlusion, vertebral artery dominance or tortuosity, and basilar artery tortuosity, and patients with infarction of the thalamus, medial temporal, or occipital lobes were more likely to have stenosis or occlusion of the vertebral or basilar arteries. Vertebrobasilar artery tortuosity, vertebral artery dominance (hypoplasia), and congenital variations of the vertebrobasilar system may lead to posterior circulation infarction at different locations in different age groups.
vertebrobasilar artery; vertebral artery; acute cerebral infarction; artery tortuosity; magnetic resonance angiography; CT angiography; neuroimaging; neural regeneration
Research Highlights
(1) Patients with posterior circulation infarction had high rates of vertebrobasilar artery developmental anomalies and tortuosity.
(2) Vertebrobasilar artery tortuosity occurred more frequently in patients aged >60 years whereas vertebrobasilar artery developmental anomalies occurred with similar frequency in patients aged <60 years and >60 years.
Abbreviations
PCI, posterior circulation infarction; MRA, magnetic resonance angiography; CTA, CT angiography; DWI, diffusion-weighted imaging.
INTRODUCTlON
Posterior circulation infarction (PCI) accounts for 15–20% of all ischemic stroke[1]. Vessels of the anterior and posterior circulations differ in congenital variations in blood vessel diameter and distribution are more common in the posterior circulation, including anomalies of the vertebrobasilar artery[2]. The diagnosis and management of PCI are complicated, because of the anatomical characteristics of the vertebrobasilar vessels and the complex clinical presentation[1]. Magnetic resonance angiography (MRA) and CT angiography (CTA) are reliable, convenient, and minimally invasive investigations which have been extensively used to diagnose PCI.
It is important to use of advances in imaging techniques to investigate etiological factors and pathogenesis in patients with cerebral infarction. This study therefore used current vessel imaging techniques to evaluate associations between developmental anomalies and tortuosity of the posterior circulation vessels, and PCI[3].
Clinical studies have shown that vascular stenosis and plaque formation are associated with cerebral infarction, but the high rates of vascular tortuosity and developmental anomalies in patients with infarction have not attracted much attention from physicians who perform imaging examinations[4]. Numerous studies have demonstrated that vertebrobasilar artery developmental anomalies and dolichoectasia may cause hemodynamic abnormalities in the posterior circulation, accelerate atherosclerosis, and contribute to the occurrence of PCI[4-6]. The prevalence of vascular tortuosity increases substantially with increasing age[7].
This study aimed to explore the associations between vascular tortuosity and developmental anomalies, and age and region of infarction, in patients with PCI, using high-field MRI and dual-source 64-slice CT.
RESULTS
Quantitative analysis of subjects
This study recruited 117 patients with acute PCI. Of these, 21 with incomplete imaging data were excluded. A total of 96 patients were included in the final analysis, including 51 males and 45 females aged 31–92 years, with a mean age of 71.6±10.4 years.
Thirty-one patients had hypertension, 24 had diabetes mellitus, 23 had coronary artery disease, 10 had a history of stroke, 16 had hypercholesterolemia, 11 had hypertriglyceridemia, 33 were smokers, and 18 were alcohol drinkers.
Diffusion-weighted MRI and MRA showed brainstem infarction in 51 patients (51/96, 53.1%), cerebellar infarction in 28 patients (28/96, 29.2%), thalamus, medial temporal lobe, or occipital lobe infarction in 11 patients (11/96, 11.5%), and combined infarction in 6 patients (6/96, 6.3%) (Figure 1).
Evaluation for intracranial and extracranial vasculopathy
Of the 96 patients, 54 underwent cranial MRA and cervical contrast enhancement MRA, and 42 underwent cranial and cervical CTA, to determine if there was intracranial or extracranial vasculopathy. Thirteen patients (13.5%) had basilar artery stenosis or occlusion, nine (9.4%) had ≥2-level basilar artery tortuosity, and six (6.3%) had other abnormalities including two cases of basilar artery dolichoectasia, two cases of basilar artery developmental anomalies, and two cases of basilar artery fenestration. Forty-one patients (42.7%) had unilateral vertebral artery stenosis or occlusion, 21(21.9%) had unilateral or bilateral vertebral artery tortuosity, 23 (23.9%) had vertebral artery dominance, and four (4.2%) had other abnormalities including one case of origin anomaly, one case of vertebral artery dissection, and two cases of bilateral vertebral artery developmental anomalies. Nine patients (9.4%) had unilateral posterior cerebral artery stenosis or occlusion and six (6.3%) had unilateral or bilateral posterior cerebral artery origin anomalies.
Five patients (5.2%) had unilateral or bilateral internal carotid artery stenosis or occlusion and four (4.2%) had severe unilateral or bilateral internal carotid artery tortuosity. No vascular lesion was found in 13 patients (13.5%).
Fifty-eight patients (60.4%) had at least two of the above-mentioned blood vessel abnormalities, including 18 patients (18.8%) with vertebral artery stenosis + vertebral artery occlusion, 14(14.6%) with abnormal distribution of the vertebral and basilar arteries, 12 (12.5%) with vertebral artery stenosis + basilar artery stenosis, seven (7.3%) with vertebral artery dominance + basilar artery tortuosity or dolichoectasia, and seven (7.3%) with other combined abnormalities (vertebrobasilar artery developmental anomalies, and vertebrobasilar system lesion + internal carotid system lesion).

Figure 1 Features of cranial MRI and magnetic resonance angiography (MRA) images in patients with acute posterior circulation infarction. R: Right.
Blood vessel imaging results according to age group
Patients aged >60 years (n=57) and <60 years (n=39) had similar rates of vertebral artery dominance and vertebrobasilar artery developmental or origin anomalies (P>0.05; Table 1).
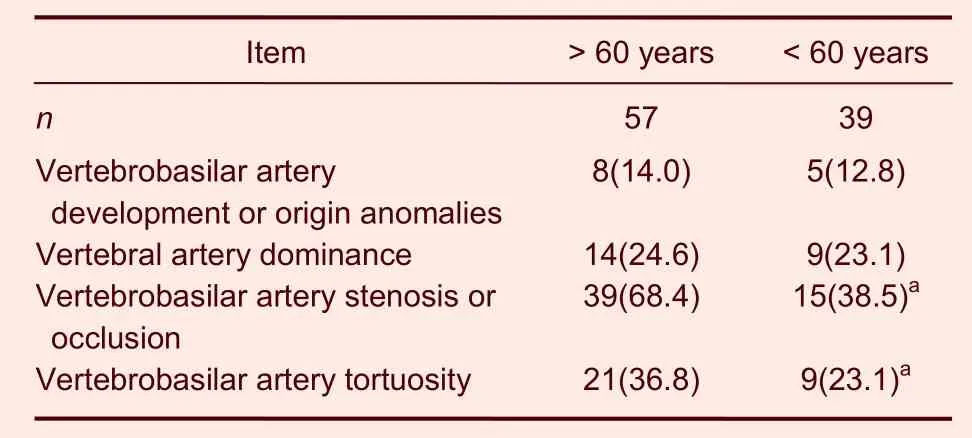
Table 1 Vertebrobasilar artery abnormalities [n (%)] according to age group
Vertebrobasilar artery stenosis or occlusion and tortuosity occurred more frequently in patients aged >60 years than <60 years (P<0.05; Table 1).
Blood vessel abnormalities according to infarct region
The rate of basilar artery abnormality was highest in patients with brainstem infarction, the rate of vertebral artery abnormality was highest in patients with cerebellar infarction, and the rate of posterior cerebral artery abnormality was highest in patients with thalamus, medial temporal lobe, or occipital lobe infarction. There were significant differences between patients with brainstem infarction and with cerebellar infarction in the rates of vertebral artery stenosis or occlusion, basilar artery stenosis or occlusion, vertebral artery dominance, vertebral artery tortuosity, and basilar artery tortuosity (P<0.05). There were significant differences between patients with thalamus, medial temporal lobe, or occipital lobe infarction and with combined infarction in the rates of vertebral artery stenosis or occlusion and basilar artery stenosis or occlusion (P<0.05). There were no significant differences between patients with thalamus, medial temporal lobe, or occipital lobe infarction and with combined infarction in the rates of vertebral artery dominance, vertebral artery tortuosity, or basilar artery tortuosity (P>0.05; Table 2).

Table 2 Vessel abnormalities [n (%)] according to the region of infarction
DISCUSSION
Vertebrobasilar artery stenosis or occlusion is considered to be the leading cause of PCI[1]. Results from this study confirm that vessel stenosis or occlusion is the major cause of PCI, accounting for 42.7% of vertebral artery disease and 13.5% of basilar artery disease. The prognosis of PCI resulting from vertebrobasilar artery stenosis or occlusion is poor. Moufarrijet al[8]reported a PCI rate of 18% within 6 years in patients with >50% vertebrobasilar artery stenosis, of which 37% were fatal. Advancements in vessel imaging techniques have shown that vertebral artery dominance or developmental anomalies, basilar artery developmental anomalies, and congenital variations of the vertebrobasilar system are important risk factors for PCI[7,9-10]. Compared with the results of various previous studies[7,9-10], the rate of vertebral artery abnormalities was high in the present study, which may be due to the broad criteria used for this group, including vertebral artery stenosis or occlusion, vertebral artery dominance (n=23), vertebral artery tortuosity (n=21), and vertebral artery developmental anomalies. These broad criteria were used to enable detailed evaluation. It is important to consider vertebral artery lesions other than stenosis and occlusion that cause hemodynamic changes and subsequent PCI[11].
Basilar artery dolichoectasia is a cerebrovascular disease with unclear pathogenesis and circulatory effects. This condition is characterized by significant prolongation, thickening, and tortuosity of the basilar artery. The etiological factors remain unclear (congenital, acquired, or both)[12]. This study explored the strong association between basilar artery tortuosity and PCI. Our results indicate that basilar artery fenestration and developmental anomalies are associated with PCI, especially brainstem and cerebellar infarction. Basilar artery dolichoectasia, tortuosity, and developmental anomalies cause hemodynamic abnormalities resulting in atherosclerotic plaque formation, aneurysm formation, and vascular occlusion. Atherosclerosis promotes vascular tortuosity, and tortuous blood vessels aggravate atherosclerotic lesion formation. Basilar artery dolichoectasia results in slowing of the blood flow and formation of mural thrombus, which may become detached and block the vessel. Basilar artery tortuosity causes compression of the artery and arterioles, resulting in small vessel occlusion[13].
The results of this study show that vertebrobasilar artery tortuosity was significantly more common in patients aged >60 years than <60 years, which is consistent with the results of a previous study[13]. Previous studies mainly focused on the association between vertebral artery dominance and development anomalies, and PCI[4-5]. The present study explored the strong association between vertebral artery tortuosity and PCI (brainstem and cerebellum). The recovery rate after these infarctions was high. A previous report indicated that congenital developmental anomalies of the arteries could result in multiple small infarctions. Developmental anomalies and vascular tortuosity affected blood flow and caused infarction[14]. The prognosis of vertebrobasilar artery tortuosity-induced infarction was good, but the retrospective study did not assess neurological deficit scores or activities of daily living. It is necessary to evaluate vascular tortuosity to detect the causative vessels in patients with PCI. The precise reason for the development of vertebral artery tortuosity remains unclear. Tortuosity often occurs in middle-aged and elderly patients, and is probably associated with decreased vascular elasticity and vascular degeneration[15]. These patients often also have carotid artery tortuosity, aortic tortuosity, and related aneurysm formation[16]. Folding and stenosis may occur in the initial portion of a tortuous vertebral artery[16]. Hemodynamic changes may occur in an excessively tortuous vertebral artery, resulting in PCI[16]. Hypertension contributes to atherosclerosis, vascular aging, and degeneration, and promotes vertebral and basilar artery tortuosity[9].
In summary, different patterns of blood vessel lesions were detected in PCI patients of different ages and with different infarct regions. Vertebrobasilar tortuosity occurred more frequently in elderly patients with cerebellar or brainstem infarction. Evaluation of the cervical vessels is very important in patients with PCI. Taken together, these results indicate that it is important to increase our understanding of the findings of blood vessel imaging examinations in PCI patients, to increase recognition of the corresponding vascular lesions.
SUBJECTS AND METHODS
Design
Retrospective case analysis.
Time and setting
Inpatients underwent cranial MRI and CTA at the Department of Neurology, Zhengzhou People’s Hospital, China from April 2009 to July 2011.
Subjects
We recruited 117 consecutive patients with acute PCI who were treated at the Department of Neurology, Zhengzhou People’s Hospital, China and underwent MRI using diffusion-weighted imaging. Patients were diagnosed according to the criteria for cerebrovascular disease developed by the Fourth China Cerebrovascular Conference in 1995[17].
Inclusion criteria
Patients who completed imaging examinations within 1 week following PCI, including cranial MRA and contrast enhanced MRA or CTA of the cranial and cervical arteries.
Exclusion criteria
Probable cardiac embolic source (atrial fibrillation, myocardial infarction within the previous 3 weeks, dilated cardiomyopathy, rheumatic heart disease, or ventricular aneurysm).
Methods
Evaluation for intracranial and extracranial vasculopathy in PCI patients using cranial imaging
MRI was performed using a GE Signa HDX 3.0 Tesla scanner (Fairfield, CT, USA). All patients were diagnosed with acute PCI. Cranial and cervical CTA were performed using dual-source 64-slice CT (Siemens, Munich, Germany). A total of 54 patients underwent cranial MRA and cervical contrast enhancement MRA, and 42 underwent CTA of the cranial and cervical arteries. Cervical contrast enhancement MRA used gadolinium contrast medium, and CTA of the cranial and cervical arteries used iodinated contrast medium. Imaging results were used to evaluate the degree of vertebrobasilar stenosis, grade of tortuosity, dolichoectasia, and other variations; vertebral artery dominance, stenosis, abnormal distribution, dissection, and other variations; posterior cerebral artery stenosis and other variations; and internal carotid artery disease.
Assessment criteria for abnormal blood vessels
(1) Grade of vertebrobasilar stenosis (judged by a physician from the Department of Imaging) as previously described[18]: ≤ 29% stenosis was defined as mild stenosis, 30–69% was defined as moderate stenosis, and ≥ 70% was defined as severe stenosis or occlusion. In accordance with North American Symptomatic Carotid Endarterectomy Trial method, stenosis was calculated as: (normal diameter at the distal end–narrowest diameter)/ normal diameter at the distal end×100%.
(2) Assessment of basilar artery dolichoectasia[19]: basilar artery length >29.5 mm was defined as dolichoectasia. If the transverse displacement from the origin of the basilar artery to the bifurcation was >10 mm, the basilar artery was considered to be abnormal.
(3) Tortuosity of the initial part of the vertebral artery[16]: tortuosity was defined when cervical contrast enhancement MRA or CTA showed vertebral artery tortuosity (helical, folding, or at least two curves).
(4) Criteria for vertebral artery dominance and tortuosity[4]: dominance was defined when there was a difference of ≥0.3 mm between the diameters of the right and left vertebral arteries, or when the vertebral arteries were the same diameter, the vertebral artery on one side tightly connected to the basilar artery, but one was narrow at the origin of the basilar artery. A line drawn from the confluence of the vertebral arteries to the bifurcation of the basilar artery determined the tortuosity and direction of the basilar artery. If there was no confluence of the vertebral arteries visible on MRA, an imaginary line was used to determine basilar artery tortuosity.
(5) Grade of basilar artery tortuosity using cranial MRA or CTA: in accordance with the criteria of Gianget al[20], basilar artery tortuosity was divided into three grades: grade 1, doubtful deviation; grade 2, significant deviation; or grade 3, basilar artery inclining to cerebellopontine angle.
Statistical analysis
Numerical data were expressed as rates. All data were analyzed using SPSS 13.0 software (SPSS, Chicago, IL, USA). Intergroup differences were compared using the chi-squared test. A value ofP<0.05 was considered statistically significant.
Funding:This study was supported by Bureau of Science and Technology of Zhengzhou City, No.12199TGG494-12.
Author contributions:Daopei Zhang and Hongtao Zhang provided the data, ensured the integrity of the data, and participated in study conception, design, data analysis, manuscript writing, and statistical analysis. Shuling Zhang and Yuming Xu were the principle investigators and approved the final manuscript.
Conflicts of interest:None declared.
Ethical approval:This study was approved by the Medical Ethics Committee, Zhengzhou People’s Hospital, China.
Author statements:The manuscript is original, has not been submitted to or is not under consideration by another publication, has not been previously published in any language or any form, including electronic, and contains no disclosure of confidential information or authorship/patent application disputations.
[1] Ishiyama G, Ishiyama A. Vertebrobasilar infarcts and ischemia. Otolaryngol Clin North Am. 2011;44(2):415-435.
[2] Savitz SI, Caplan LR. Vetebrobasilar disease. N Engl J Med. 2005;352(25):2618-2626.
[3] Qiao YN, Wang ML. Correlation between stenosis or occlusion of vertebral-basilar artery and the location of infarctions in pontine. Zhonghua Shenjingke Zazhi. 2011;44(4):229-233.
[4] Hong JM, Chung CS, Bang OY, et al. Vertebral artery dominance contributes to basilar artery curvature and peri-vertebrobasilar junctional infarcts. J Neurol Neurosurg Psychiatry. 2009;80(10):1087-1092.
[5] Perren F, Poglia D, Landis T, et al. Vertebral artery hypoplasia: a predisposing factor for posterior circulation stroke? Neurology. 2007;68(1):65-67.
[6] Wentland AL, Rowley HA, Vigen KK, et al. Fetal origin of the posterior cerebral artery produces left-right asymmetry on perfusion imaging. AJNR Am J Neuroradiol. 2010;31(3): 448-453.
[7] Zhao ZN, Wang XY, Zhu MJ, et al. Basilar artery tortuosity is related to age and cerebral basilar atery infarctions. Zhonghua Shenjingke Zazhi. 2010;43(7):505-508.
[8] Moufarrij NA, Little JR, Furlan AJ, et al. Basilar and distal vertebral artery stenosis: long-term follow-up. Stroke. 1986;17(5):938-942.
[9] Cosar M, Yaman M, Eser O, et al. Basilar artery angulation and vertigo due to the hemodynamic effect of dominant vertebral artery. Med Hypotheses. 2008;70(5): 941-943.
[10] Jellici E, Beltramello A, Vasori S, et al. Kinking of the vertebral artery. Eur Radiol. 2003;13(6):1469-1471.
[11] Park JH, Roh JK, Kwon HM. Ischemic stroke patterns and hemodynamic features in patients with small vertebrobasilar artery. J Neurol Sci. 2009;287(1-2): 227-235.
[12] Passero SG, Rossi S. Natural history of vertebrobasilar dolichoectasia. Neurology. 2008;70(1):66-72.
[13] Ikeda K, Nakamura Y, Hirayama T, et al. Cardiovascular risk and neuroradiological profiles in asymptomatic vertebrobasilar dolichoectasia. Cerebrovasc Dis. 2010;30(1):23-28.
[14] Olindo S, Khaddam S, Bocquet J, et al. Association between basilar artery hypoplasia and undetermined or lacunar posterior circulation ischemic stroke. Stroke. 2010;41(10):2371-2374.
[15] Dodevski A, Lazareska M, Tosovska-Lazarova D, et al. Morphological characteristics of the first part of the vertebral artery. Prilozi. 2011;32(1):173-188.
[16] Fang CQ, Li JC, Gao CY, et al. Clinical study of effect of vertebral artery kinking on cerebral hemodynamics. Zhonghua Laonianyixue Zazhi. 2010;29(9):712-714.
[17] Chinese Neuroscience Association. Various types of cerebrovascular disease diagnosis. Zhonghua Shenjingke Zazhi. 1996;29(6):379-380.
[18] Zarins CK. Carotid endarterectomy: the gold standard. J Endovasc Surg. 1996;3(1):10-15.
[19] Ubogu EE, Zaidat OO. Vertebrobasilar dolichoectasia diagnosed by magnetic resonance angiography and risk of stroke and death: a cohort study. J Neurol Neurosurg Psychiatry. 2004;75(1):22-26.
[20] Giang DW, Perlin SJ, Monajati A, et al. Vertebrobasilar dolichoectasia: Assessment using MR. Neuroradiology. 1988;30(6):518-523.
10.3969/j.issn.1673-5374.2012.32.008 [http://www.crter.org/nrr-2012-qkquanwen.html]
Zhang DP, Zhang SL, Zhang HT, Xu YM. Characteristics of vascular lesions in patients with posterior circulation infarction according to age and region of infarct. Neural Regen Res. 2012;7(32):2536-2541.
Daopei Zhang☆, Studying for doctorate, Attending physician, Third Department of Neurology, Zhengzhou People’s Hospital, Zhengzhou 450003, Henan Province, China
Shuling Zhang, Chief physician, Third Department of Neurology, Zhengzhou People’s Hospital, Zhengzhou 450003, Henan Province, China zhangshuling99@ yahoo.com.cn
2012-07-06
2012-09-24 (N20111004001/WJ)
We thank Yong Liu and Suo Yin from the Department of Imaging and Medical Science for providing imaging data. We are grateful to Shengqi Fu and Peng Ji for providing clinical data.
(Edited by Feng JC, Wang JF/Qiu Y/Song LP)
杂志排行
中国神经再生研究(英文版)的其它文章
- Morphological differences in skeletal muscle atrophy of rats with motor nerve and/or sensory nerve injury*★
- A standardized method to create peripheral nerve injury in dogs using an automatic non-serrated forceps***★
- Rapid genetic screening of Charcot-Marie-Tooth disease type 1A and hereditary neuropathy with liability to pressure palsies patients**★
- Ultrasound guided neural stem cell transplantation through the lateral ventricle for treatment of cerebral palsy in children☆
- Correlation between spina bifida manifesta in fetal rats and c-Jun N-terminal kinase signaling**★
- Tacrolimus reduces scar formation and promotes sciatic nerve regeneration*☆
