Resection of hepatic caudate lobe hemangioma: experience with 11 patients
2010-06-29LiNingXuandZhiQiangHuang
Li-Ning Xu and Zhi-Qiang Huang
Beijing, China
Original Article / Liver
Resection of hepatic caudate lobe hemangioma: experience with 11 patients
Li-Ning Xu and Zhi-Qiang Huang
Beijing, China
BACKGROUND:Caudate lobectomy is now considered to be the most appropriate surgical treatment for benign tumors in the caudate lobe. But how to resect the caudate lobe safely is a major challenge to current liver surgery and requires further study. This research aimed to analyze the perioperative factors and explore the surgical technique associated with liver resection in hepatic caudate lobe hemangioma.
METHODS:Eleven consecutive patients with symptomatic hepatic hemangiomas undergoing caudate lobectomy from November 1990 to August 2009 at our hospital were investigated retrospectively. All patients were followed up to the present.
RESULTS:In this series, 9 were subjected to isolated caudate lobectomy and 2 to additional caudate lobectomy (in addition to left lobe and right lobe resection, respectively). The average maximum diameter of tumors was 9.65±4.11 cm. The average operative time was 232.73±72.16 minutes. Five of the 11 patients required transfusion of blood or blood products during surgery. Ascites occurred inlpatient, pleural effusion in the perioperative period in 1, and multiple organ failure inlon the 6th day after operation as a result of massive intraoperative blood loss, who had received multiple transcatheter hepatic arterial embolization preoperatively. The alternating left-right-left approach produced the best results for caudate lobe surgery in most of our cases. All patients who recovered from the operation are living well and asymptomatic.
CONCLUSIONS:For large hemangioma of the caudate lobe, surgery is only recommended for symptomatic cases. Caudate lobectomy of hepatic hemangioma can be performed safely, provided it is carried out with optimized perioperative management and innovative surgical technique.
(Hepatobiliary Pancreat Dis Int 2010; 9: 487-491)
caudate lobe; hemangioma; hepatectomy; perioperative; surgical technique
Introduction
The caudate lobe is considered to be a separate and distinct liver lobe, with its own vascularization and biliary drainage. It is generally divided into 3 portions: the left Spiegel lobe (Couinaud's segment 1), the process portion, and the paracaval portion (Couinaud's segment 9).[1,2]The caudate lobe is an autonomous segment of the liver and is surgically difficult to approach because of its location deep in the hepatic parenchyma beneath the confluence of the main hepatic (left and middle) veins and its adjacency to the porta hepatis, the ligamentum venosum, and the inferior vena cava. Caudate lobectomy was first described by Lerut in 1990,[3]and is often challenging, even to accomplished hepatic surgeons. Caudate lobectomy for localized tumors was a controversial topic in the 1990s. It is now considered to be the most appropriate surgical treatment for benign tumors in the caudate lobe. Caudate lobectomy is increasingly performed. But how to resect the caudate lobe safely is still a major challenge to liver surgery and requires further investigation. Currently, hepatic hemangioma is the most frequently diagnosed benign liver tumor and is the most frequently resected non-malignant liver tumor.[4]From November 1990 to August 2009, a total of 11 patients underwent caudate lobe resection for hemangiomas at our hospital. The "alternating left-right-left approach" was adopted, and produced the best results in most of the cases.
Methods
Patients
From November 1990 to August 2009, 11 consecutive patients (3 men and 8 women) underwent hepaticcaudate lobectomy for symptomatic hemangiomas; their median age was 41 years (range 32-59). As a rule, operation was only recommended for symptomatic cases, and the size of the lesion was not the criterion for excision. Diagnoses and features of the hemangioma (including number of tumors and size of the largest tumor) were obtained from the pathology records. The postoperative variables taken into consideration included complications and mortality. Death of any patient within 30 days of hepatectomy was considered as a surgical death. General data of the 11 patients with caudate lobe hemangioma are listed in Table 1. Longterm outcomes of the patients were recorded at followup visits; family members were included in some cases.
Operative techniques
Most frequently, a right subcostal incision (10 patients) was made and in 1 patient, an inverted "Y" incision was made because of additional tumors in the left and right liver lobes. The "alternating left-rightleft approach" as previously reported[5]for caudate lobectomy was used. Briefly, at first the hepatic artery along the left lateral border of the hepatoduodenal ligament was isolated, and then the downward and backward branches supplying the caudate lobe were divided. A caudate lobe hemangioma may be softer and compressible as a result of blockade of its arterial blood supply. Then, a procedure was carried out on the right side to divide the multiple veins draining from the caudate lobe to the inferior vena cava, and the process portion of the lobe was separated from the right liver and pushed toward the left side to the hepatoduodenal ligament for further manipulation. Lastly, as left to the hepatoduodenal ligament, the tumor was retracted upward to expose the inferior vena cava and the main caudate vein, which may be short and large; the inferior vena cava may be partially occluded by an atraumatic clamp when dividing the short caudate vein seems to be risky. After the caudate hemangioma has been separated from the inferior vena cava, the upper pole of the caudate lobe was carefully dissected from the undersurface of the middle and the lateral hepatic veins; this is one of the critical steps in isolated caudate lobectomy.
Results
Size of tumor
Categorization of hepatic cavernous hemangioma is made on account of its clinical symptoms and tumor volume; accordingly, each tumor is classified into 3 categories according to its longest diameter as measured from the CT scan: small: ≤5 cm in diameter; large, 5-10 cm; and giant hemangioma: ≥10 cm).[6]However, in our series, the size of a hemangioma was determined by measurement of the surgical specimen sent to the pathological laboratory, which was inevitably smaller than that appearing on CT imaging on account of emptying of blood and tissue fixation. The largest tumor was 20 cm in diameter, the average was 9.65±4.11 cm, and most of the cases were large (4 patients) or giant hemangiomas (6).
Perioperative results
The average operative time was 232.73±72.16 minutes (range 95-325; median 240). Five patients required transfusion of blood or blood products during surgery. In one patient, who received multiple sessions of transcatheter hepatic arterial embolization treatment for hepatic hemangioma preoperatively, the estimated blood loss from the cut surface of the liver was about1000 ml. Blood lost during surgery was collected and retransfused in 4 patients.

Table 1. General data from the 11 patients with caudate lobe hemangioma
Complications and mortality
There were one patient with ascites and one with pleural effusion in the perioperative period; these patients were managed successfully by general treatment such as concentrated human albumin transfusion, adjustment of water and electrolyte balance, or diuretics.
There was one death in our group. She was a 53-year-old female diagnosed with right-sided hepatic hemangioma in 1992, which was treated with two sessions of transcatheter hepatic arterial embolization on the advice of her doctor, but the result was unsatisfactory as neither the volume of the tumor nor the clinical symptoms showed any improvement. She was admitted to PLA General Hospital in October 1999 on the diagnosis of multiple giant hepatic hemangiomas (10 cm in diameter, right lobe and caudate lobe, and two 5 cm tumors in the left lateral lobe). The hemangiomas of the left lateral lobe were successfully resected, but resection of the huge hemangiomas of the right lobe and caudate lobe was difficult because of massive blood loss and difficult hemostasis. Re-operation was performed on account of intra-abdominal bleeding, and eventually, the patient died of multiple organ failure on the sixth postoperative day.
Postoperative course
No adjuvant treatment was given after surgery. Follow-up was done in the 10 surviving cases. Median follow-up was 120 months (range 46-225; mean 102). These patients underwent an uneventful course of recovery and are living well without symptoms.
Discussion
Caudate lobectomy is a technically-demanding procedure that entails the surgeon's judgement and precise knowledge of liver anatomy. Therefore, it has long been considered a difficult and dangerous operation.[7]The caudate lobe is not only deeply embedded between the hilar structures of the liver and the inferior vena cava but also has its own independent vascular supply and biliary drainage. Eleven cases of caudate lobe resection are reported with a review of the literature and discussion of the indications for surgery, surgical technique, and our experience of caudate lobectomy for huge hemangiomas.
Caudate lobe hemangioma, a not infrequent clinical entity
Cavernous hemangioma, as for other locations in the liver, is the most frequent benign lesion of the caudate lobe.[8]Perhaps caudate hemangioma causes more clinical symptoms than other benign liver tumors owing to its distensibility and intimate relationship with other intra-abdominal viscera such as the stomach.
Clinical significance of caudate lobe hemangioma: 1) symptoms are often obvious, causing epigastric discomfort, gas pains, and eating disorder on account of oppression of the lesser curvature of the stomach, and 2) caudate lobe resection is highly risky, and only a few reports were found in the world literature. With the key words "caudate lobe" and "hemangioma", we searched in PubMed up to November 2009 and found only 6 papers describing 19 cases of caudate lobectomy; the maximum diameter of the resected tumor ranged from 5 to 30 cm, including 5 cases of complete caudate lobectomy and 11 cases of local excision and enucleation (Table 2).[9-14]Popescu et al[13]reported 2 cases of giant hemangioma enucleation under total hepatic blood flow blockade. Therefore, isolated caudate lobectomy for caudate lobe hemangioma is infrequently performed.
Surgical approaches to caudate lobectomy
Resection of the caudate lobe with a large tumor is a technical challenge. It is difficult to perform because of its deep location and adjacency to the major hepatic vessels (i.e., the left and middle hepatic veins). Access to and resection of the caudate lobe should be made on the basis of tumor location and hepatic functional reserve.[15]The left or right approach to the caudate lobe can be recommended for local resection of a tumor located at Spiegel's portion or the process portion.[16]Resection of the caudate lobe using the anterior approach should be the first choice for treatment of giant tumors confined to the lobe alone,[17]and is especially recommended when tumors are located in the paracaval portion (segmentⅨ).[18]An anterior trans-parenchymal approach for isolated caudate lobectomy can provide a better operative field and overcome certain difficulties which may appear during resection.[19]The choice of approaches to caudate lobectomy is therefore largely dependent on the size and location of the lesion, and the type of resection. For isolated caudate lobectomy or lobectomy in addition to right or left hepatectomy, a bilateral subcostal incision may offer the best exposure.[20]
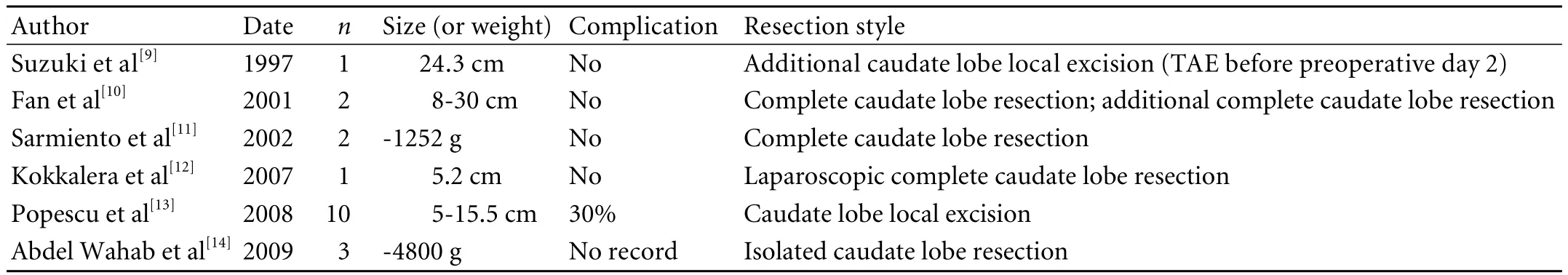
Table 2. Literature on caudate lobectomy in hepatic hemangioma
Morbidity and mortality
Hemangioma is a benign tumor, so safety of the operation should be the most important initial consideration. Presently, isolated caudate lobe resection is a safe procedure with good outcome in well-selected patients. However, it may be associated with increased perioperative risks when combined with other major hepatectomy in the same setting.[14]In our series, 1 case of ascites and 1 case of pleural fluid occurred in the postoperative period. The one death was the result of resection of multiple huge tumors (a combined resection of the liver in the caudate lobe, right lobe, and left lobe).
Surgical experience
Local excision and enucleation of small hemangiomas of the caudate lobe may proceed with no difficulty,[21]but with giant hemangiomas the situation is more complicated, and isolation and excision of the lobe may be hazardous. Hemorrhage from the undersurface of the liver may be profuse and hard to control. And there is no definite limit between the right caudate lobe and right posterior lobe, which often needs to be resected (Fig. 1).
In cases of giant caudate lobe hemangioma, the tumor fully occupies the epigastric region so as to cause a sensation of fullness clinically and, at first, to leave little space for surgical manipulation. But another feature of hemangioma is its compressibility; the tumor may shrink in size and become softer when its blood supply is occluded. In our experience, resection of giant hemangioma was made easier when the arterial branches to the caudate lobe were divided along the left border of the hepatoduodenal ligament (Fig. 2). Therefore, the operation was carried out by initial isolation and division of the downward and backward branches from the hepatic artery (feeding the caudate lobe), then the hemangioma became softer and more compressible.

Fig. 1. Right caudate lobe hemangioma, no definite limit between the tumor and right posterior lobe.

Fig. 2. Resection of giant hemangioma made easier when arterial branches to the caudate lobe were divided along the left border of the hepatoduodenal ligament.
Treatment of the caudate veins is another critical step in resection. The venous return from a giant caudate lobe hemangioma is often short and have a large-caliber. Many caudate veins should be approached from the right side because of better exposure when the tumor is retracted medially, but the main caudate vein should be approached from the left when the tumor is retracted upward. In our experience, the caudate veins was divided more conveniently and safely when the inferior vena cava was partially clamped (Fig. 3).
As the caudate lobe is situated directly behind the left and middle hepatic vein junction, injury to these veins may cause profuse bleeding and the danger of air embolism. Therefore, a controlling catheter encircling the suprahepatic inferior vena cava was regularly placed at the beginning of the operation to control hemorrhage, although it was not necessary in any of our cases. Ordinarily, there was an anatomic interspace between the upper pole of the left caudate lobe and the middle hepatic vein (Fig. 4), which was a safe passage in freeing of the upper pole of the caudate lobe, a critical step in isolated caudate lobe resection. At this time, completemobilization of the left liver was essential.

Fig. 3. The caudate was divided more conveniently and safely when the inferior vena cava was partially clamped.

Fig. 4. There was an anatomic interspace between the upper pole of the left caudate lobe and the middle hepatic vein.
In summary, for large hemangiomas of the caudate lobe, surgery is only recommended for symptomatic cases. Caudate lobectomy for hepatic hemangioma can be performed safely, provided it is carried out with optimized perioperative management and innovative surgical technique.
Funding:None.
Ethical approval:Not needed.
Contributors:XLN and HZQ proposed the study and wrote the first draft. XLN analyzed the data. Both authors contributed to the design and interpretation of the study and to further drafts. XLN is the guarantor.
Competing interest:No benefits in any form have been received or will be received from a commercial party related directly or indirectly to the subject of this article.
1 López-Andújar R, Montalvá E, Bruna M, Jiménez-Fuertes M, Moya A, Pareja E, et al. Step-by-step isolated resection of segment 1 of the liver using the hanging maneuver. Am J Surg 2009;198:e42-48.
2 Murakami G, Hata F. Human liver caudate lobe and liver segment. Anat Sci Int 2002;77:211-224.
3 Lerut J, Gruwez JA, Blumgart LH. Resection of the caudate lobe of the liver. Surg Gynecol Obstet 1990;171:160-162.
4 Charny CK, Jarnagin WR, Schwartz LH, Frommeyer HS, DeMatteo RP, Fong Y, et al. Management of 155 patients with benign liver tumours.Br J Surg 2001;88:808-813.
5 Huang ZQ. Isolated hepatic caudate lobectomy. Xiao Hua Wai Ke 2002;1:62-65.
6 Huang ZQ. Focus on hepatobiliary and pancreatic surgery. 1st ed. Beijing: People's military medical press; 2005:70.
7 Zuo HQ, Yan LN, Zeng Y, Yang JY, Luo HZ, Liu JW, et al. Caudate lobectomy by the third porta hepatis anatomical method: a study of 16 cases. Hepatobiliary Pancreat Dis Int 2006;5:387-390.
8 Huang ZQ, Xu LN, Yang T, Zhang WZ, Huang XQ, Liu R, et al. Liver resection: single center experiences of 2008 consecutive resections in 20 years. Zhonghua Wai Ke Za Zhi 2008;46:1314-1321.
9 Suzuki H, Nimura Y, Kamiya J, Kondo S, Nagino M, Kanai M, et al. Preoperative transcatheter arterial embolization for giant cavernous hemangioma of the liver with consumption coagulopathy. Am J Gastroenterol 1997;92:688-691.
10 Fan J, Wu ZQ, Tang ZY, Zhou J, Qiu SJ, Ma ZC, et al. Complete resection of the caudate lobe of the liver with tumor: technique and experience. Hepatogastroenterology 2001;48:808-811.
11 Sarmiento JM, Que FG, Nagorney DM. Surgical outcomes of isolated caudate lobe resection: a single series of 19 patients. Surgery 2002;132:697-709.
12 Kokkalera U, Ghellai A, Vandermeer TJ. Laparoscopic hepatic caudate lobectomy. J Laparoendosc Adv Surg Tech A 2007;17: 36-38.
13 Popescu I, Ciurea S, Romanescu D, Boros M. Isolated resection of the caudate lobe: indications, technique and results. Hepatogastroenterology 2008;55:831-835.
14 Abdel Wahab M, Lawal AR, EL Hanafy E, Salah T, Hamdy E, Sultan AM. Caudate lobe resection: an Egyptian center experience. Langenbecks Arch Surg 2009;394:1057-1063.
15 Chaib E, Ribeiro MA Jr, Silva Fde S, Saad WA, Cecconello I. Surgical approach for hepatic caudate lobectomy: Review of 401 cases. J Am Coll Surg 2007;204:118-127.
16 Chaib E, Ribeiro MA Jr, Silva Fde S, Saad WA, Cecconello I. Caudate lobectomy: tumor location, topographic classification, and technique using right- and left-sided approaches to the liver. Am J Surg 2008;196:245-251.
17 Hu JX, Miao XY, Zhong DW, Dai WD, Liu W. Anterior approach for complete isolated caudate lobectomy. Hepatogastroenterology 2005;52:1641-1644.
18 Chaib E, Ribeiro MA Jr, de Souza YE, D'Albuquerque LA. Anterior hepatic transection for caudate lobectomy. Clinics (Sao Paulo) 2009;64:1121-1125.
19 Peng SY, Hong DF, Xu B, Wang JW, Liu YB, Qian HR, et al. The strategy of isolated complete resection of the caudate lobe of the liver through the anterior liver-splitting approach: a report of 19 cases. Zhonghua Wai Ke Za Zhi 2007;45:1321-1324.
20 Sasada A, Ataka K, Tsuchiya K, Yamagishi H, Maeda H, Okada M. Complete caudate lobectomy: its definition, indications, and surgical approaches. HPB Surg 1998;11:87-95.
21 Huang ZQ. Huang Zhiqiang hepatic surgery operation. 1st ed. Beijing: People's military medical press; 2005:275-278.
December 10, 2009
Accepted after revision April 28, 2010
Author Affiliations: Department of General Surgery and Intensive Care Unit, Clinical Division of South Building (Xu LN), and Institute of Hepatobiliary Surgery, Clinical Division of Surgery (Huang ZQ), Chinese PLA General Hospital, Beijing 100853, China
Zhi-Qiang Huang, Professor, Institute of Hepatobiliary Surgery, Clinical Division of Surgery, Chinese PLA General Hospital, Beijing 100853, China (Tel: 86-10-66936609; Fax: 86-10-66936609; Email: chaoyue528@sohu.com)
© 2010, Hepatobiliary Pancreat Dis Int. All rights reserved.
杂志排行
Hepatobiliary & Pancreatic Diseases International的其它文章
- News
- Advances in prognostic factors in acute pancreatitis: a mini-review
- Hepatocellular carcinoma metastatic to the kidney mimicking renal oncocytoma
- Simultaneous breast and ovarian metastasis from gallbladder carcinoma
- An eight-year journey of Hepatobiliary & Pancreatic Diseases International
- Interferon and lamivudine combination therapy versus lamivudine monotherapy for hepatitis B e antigen-negative hepatitis B treatment: a meta-analysis of randomized controlled trials
