原发性小肠淋巴瘤的诊断和外科治疗
2009-05-06黄桂填徐波
黄桂填 徐 波
【摘要】 目的 探讨原发性小肠淋巴瘤(primary small intestine lymphoma,PSIL)的临床表现、CT特点,提出临床策略。方法 回顾性分析2003年1月至2007年7月收治的15例PSIL的患者临床资料。结果 15例患者中男9例,女6例,平均51.6岁。PSIL常见的临床表现为:腹痛、腹部肿物、肠梗阻、消化道出血及消瘦;血CEA、CA199均正常。术前15例均行CT检查,CT 初诊检出肿瘤15例,定性诊断准确12例;15例中,11例行消化道钡餐检查,4例检出病变,仅1例提示淋巴瘤可能。15例患者均行手术治疗,无围手术期死亡,术后病理结果为PSIL,术后1年生存率为85.7%。 结论 PSIL无特异性临床症状,消化道钡餐诊断率低,CT扫描具有一定的特征,结合临床具有较高的诊断价值。早期诊断对改善PSIL的预后十分重要,积极手术切除和辅助化疗可以获得良好效果。
【关键词】 淋巴瘤;小肠;诊断
Diagnosis and surgical treatment of primary small intestine lyphoma
HUANG Gui-tian,XU Bo.Emergency Department,Guangzhou City Ist Peoples Hospital,Guangdong 51000,China
【Abstract】 Objective To approach the diagnosis and treatment of primary lymphoma of the small intestine.Methods The clinical data of 15 patients with primary lymphoma of the small intestine from January 2003 to July 2007 were reviewed.Results Of the 15 cases,9 cases were male and 6 cases were female,the average age was 51.6 years.The commonest clinical manifestation were as follow:abdominal pain,abdominal lump,bowel obstruction,alimentary tract hemorrhage and athrepsy.CEA and CA199 values of blood serum were normal.All of these cases were under went CT scanning before operation.In 12 of 15 cases were final diagnosised by CT scanning.11 cases were subjected to Ba-meal examinations.Positive results were found in 4 cases,and only 1 case was considered to be PSIL.All of them received surgical operation.The postoperative pathology of all the patients were primary small intestine lymphoma.The 1year postoperative survival rate was 85.7%.Conclusion
PSIL had no specificity clinical manifestation.Barium study had hypo-diagnosis ratio,CT scan had specific diagnostic characteristics for PSIL.In combination with CT scan and clinical manifestation examinations are mutually beneficial in the diagnostic process.Most of the patients with primary lymphoma of the small intestine were in advanced stages when operated or diagnosed,so early diagnosis and comprehensive therapy were the key to ameliorate the patientsprognosis.
【Key words】 Lymphoma;Small intestine;Imaging diagnosis
原发性小肠淋巴瘤(primary small intestine lymphoma,PSIL)是较少见的消化道恶性肿瘤,起病隐匿,临床表现缺乏特征性,易于误诊。现收集本院2003年1月至2007年7月收治的PSIL 15例,本文将结合其临床表现特征和CT特点进行综合分析、诊断并提出临床对策。
1 资料与方法
1.1 一般资料 本组病例共15例,其中男9例,女6例,发病年龄18~73岁,平均51.6岁,40岁以上者11例,占73.3%。病程1周~1.5年。临床表现包括腹痛、腹部肿物、肠梗阻、消化道出血及消瘦,血肿瘤指标(CEA、CA199)均正常。所有病例均符合Dawson标准[1]:①无病理性浅表淋巴结肿大;②胸片无纵隔淋巴结肿大;③末梢血中无幼稚细胞或异常细胞;④肿瘤主要位于小肠或经淋巴管侵犯附近的淋巴结;⑤肝、脾无侵犯(邻近病变的直接扩散除外)。
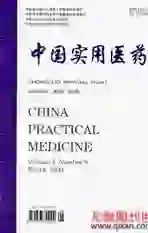
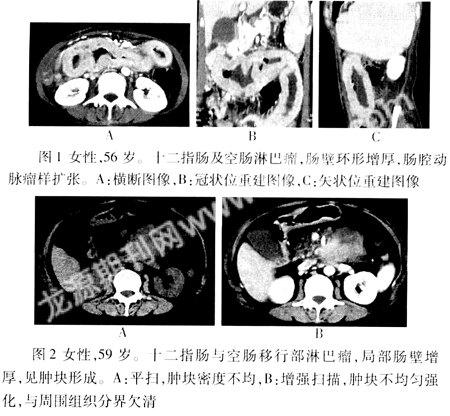
1.2 CT检查 本组15例全部行腹部CT检查,主要表现为肠壁增厚、肠腔内肿块和肠系膜淋巴结肿大,继发表现则有肠套叠、肠梗阻和少量腹水。根据其主要的异常CT征象,本组15 例淋巴瘤可分为浸润型和肿块型。其中浸润型10例,表现为肠壁广泛环形增厚(图1),增厚的肠壁厚度在1.0~3.3 cm间。病变处的肠腔见“动脉瘤样”扩张7例,最大的扩张肠腔内径为4.1 cm,3例肠腔变化不大,另1 例肠腔轻度狭窄伴不完全性肠梗阻。病变累及肠管总长度最短8.3 cm,最长达36 cm。肿块型5例,表现为肠壁局限性或环形增厚,肠腔内或肠壁肿块形成(图2),肿块直径2.7~8.1 cm,其中2例肠腔扩张,1例肠腔狭窄伴不全梗阻。15例病变平扫均表现为软组织密度,2例浸润型和5例肿块型病灶内可见不规则低密坏死区,增强扫描病灶轻度强化。7例病变段肠壁周围脂肪间隙消失。9例合并肠系膜淋巴结肿大。CT诊断结果:浸润型10例,9例定性正确,1例误诊肠腺癌;肿块型5例,3例定性正确,1例未定性,1例误诊为间质瘤;CT初诊检出肿瘤15例,定性诊断准确12例。
1.3 消化道钡餐检查 本组11例术前行消化道钡餐检查,1例肠壁黏膜皱襞消失,肠腔扩张,提示淋巴瘤可能;1例肠壁黏膜皱襞消失,见多发细小龛影,误诊为局限性肠炎;2例提示外压性改变,另7例未见明显异常。
[2] 黄文柱,张亚历,但汉雷.现代小肠病学.军事医学科学出版社,2002:412-415.
[3] Nakamura S,Matsumoto T,Iida M,et al.Primary gastroin-testinal lymphoma in Japan:a clinicopathologic an alysis of 455 patients with special reference to its time trends.Cancer,2003,97:2462-2473.
[4] 周康荣.腹部CT.上海医科大学出版社,1993:133.
[5] Levine MS,Rubesin SE,Pantongrag-Brown L,et al.Non-Hodgkins lymphoma of the gastrointestinal tract:Radiographic findings.AJR,1997,168(1):165-172.
[6] Buckley JA,Fishman EK.CT evaluation of small bowel neoplasms:spectrum of disease.Radiographics,1998,18:379-392.
[7] 徐宏刚,陈阿梅,江新青.胃肠管淋巴瘤的多层螺旋CT诊断.国际外科学杂志,2008,35:156-159.
[8] Nakamura S,Matsum0to T,Iida M,et al.Primary gastrointestinal lymphoma in Japan:a clinicopathologic an alysis of 455 patients with special reference to its time trends.Cancer,2003,97:2462-2473.
[9] Samel S,Wagner J,Hofheinz R,et al.M alignant intestinal non-HodgkinS lymphoma from the surgical point of view.Onkologie,2002,25:268.
[10] Zinzani PL.Autologous hematopoietie stem cell transplantation in Non-Hodgkin's lymlphomas.Acta Haematol,2005,114(4):255.