运动控制训练对女大学生髌股关节痛的影响研究
2024-12-31王刚韩亚兵黄雄峰蔡宁宁赵小娟陈炜炜






【摘要】目的"评价运动控制训练(MCE)对女大学生髌股关节痛(PFP)的疗效。为PFP的治疗提供理论依据。方法 将36名受试者随机分配到MCE组和对照组,各18人。对照组进行假干预。实验组进行MCE。每周训练3次,共6周。分别在干预前和干预后记录单腿深蹲(SLS)时臀中肌和臀大肌肌电均方根(RNS)以及动态膝外翻角(DKV),评估膝关节Lysholm量表、视觉模拟评分(VAS)以及Y平衡。结果"干预6周后,对照组各项指标均无显著性变化(P>0.05),MCE组各项指标除Y平衡后外侧、后内侧最大伸展距离无统计学变化,其余各指标均有显著性改善( P<0.05),MCE组除Y平衡外各项指标均优于对照组( P<0.05)。结论"MCE可以增强PFP女大学生臀部肌肉激活、降低DKV角,改善下肢姿势控制、减轻疼痛和提高膝关节功能。
【关键词】运动控制训练 "髌股关节痛 "动态膝外翻 "单腿深蹲
The effect of Motor Control Exercise on patellofemoral pain in female college students
Wang Gang1""Han Yabing2""Huang Xiongfeng3""Cai Ningning*3"""Zhao Xiaojuan3""Chen Weiwei3
1.Xi’an Physical Education University, Xi’an,China 710068 "2.Ankang University, Ankang,China 725000
3.Fuzhou Medical College of Nanchang University, Fuzhou,China 344099
【Abstract】Objective"This study aims to evaluate the efficacy of motor control exercise (MCE) in alleviating patellofemoral pain (PFP) among female college students and to provide a theoretical foundation."Methods"Thirty-six participants were randomly assigned to either the MCE group (n=18) or the control group (n=18)."The control group underwent a sham intervention, while"the experimental group engaged in Motor Control Exercises (MCE). Training sessions were conducted three times per week over a period of six weeks.The root mean square (RMS) of the gluteus medius and gluteus maximus electromyography (EMG) during single-leg squats (SLS), along with the dynamic knee valgus (DKV) angle, were measured both before and after the intervention."Furthermore, the Lysholm knee scoring scale, Visual Analog Scale (VAS), and Y-Balance test were assessed. Results"After six weeks of intervention, no significant changes were observed in the control group across any of the indicators (Pgt;0.05). In contrast, the MCE group demonstrated significant improvements in all outcome measures, except for the posterolateral and posteromedial maximum reach distances on the Y-balance test (Plt; 0.05). Additionally, all indicators in the MCE group, excluding the Y-balance test, showed significantly better results compared to the control group (Plt;0.05). Conclusion"MCE"can enhance hip muscle activation, reduce the DKV, improve lower limb postural control, alleviate pain, and enhance knee joint function in female college students with PFP.
【Key words】Motor control exercise "Patellofemoral arthralgia""Dynamic Knee Valgus"single-leg squats
前言
髌股关节痛(patellofemoral pain,PFP)是一种常见的膝关节疾病,主要由髌股关节内的病理改变或异常生物力学引起[1]。其特征是膝前部疼痛,在上下楼梯、跑步等活动后会加重[2-3]。流行病学表明,PFP主要影响18至35岁的年轻人,发病率约为每1000人中22例。随访研究显示,45%最初诊断为PFP的患者持续经历疼痛[4]。Hansen[5]等人进行了一项随访发现,74%的PFP患者尽管接受了治疗,但在体育活动和日常生活中仍有不同程度的限制。这种持续的症状影响了运动员的运动表现、心理健康和整体生活质量。PFP被也广泛认为是髌股关节炎发生的危险因素[6]。女性患PFP的风险更高[4]。性别差异可能与女性解剖特征、激素波动和神经肌肉控制有关[7]。女性股骨前倾角、Q角和膝关节外翻角较大,易在功能活动中形成异常的运动模式[8]。此外,女性还表现出神经肌肉控制不足,这与臀部肌肉激活和力量的减少有关[4]。臀肌力量下降的个体在单腿着陆和单腿下蹲动作时容易发生动态膝关节外翻(Dynamic Knee Valgus, DKV)[9]。DKV以髋关节内收、膝关节外展和胫骨外旋为特征,与前交叉韧带撕裂和PFP的形成具有相关性[10]。
运动疗法,特别是股四头肌力量训练,常用于治疗PFP。该方法旨在增强股四头肌的肌力,从而纠正髌骨的异常运动轨迹,增强髌股关节的稳定性[11,12]。通常推荐高强度的股四头肌抗阻训练,但这种高强度的阻力可能会增加髌股关节压力,加剧髌股关节疼痛[13]。运动控制训练(Motor Control Exercise, MCE),也称神经肌肉控制训练、动态肌肉稳定训练,是一个全面的训练计划。重点强调特定肌肉激活,促进关节动态稳定,改善肢体神经肌肉运动控制[14]。尽管MCE作为一种治疗手段的潜在优势已被证实,但使用MCE作为PFP治疗的研究有限。此外,目前还缺乏强有力的证据来证实MCE对PFP患者的疗效和下肢生物力学影响。本研究旨在探究MCE对女大学生PFP患者的临床疗效和下肢生物力学影响,以期为治疗PFP提供证据支持。
1.研究资料与方法
1.1研究对象
本研究选取的受试对象为西安体育学院在校女大学生,共招募52例,筛选后最终纳入36名,按招募顺序进行编号。利用Excel生成随机数,并按照升序排列这些随机数,与受试者编号对应,1-18为MCE组,19-36为对照组。
1.1.1纳入标准[15-16]
符合2016年髌股疼痛国际研讨会制定的PFP诊断标准:1)长时间坐、上楼梯、蹲、跑、跪、跳跃时出现膝盖周围或后面的疼痛;2)日常生活中或前一周训练时VAS≥3cm;3)单侧受累,病情持续时间>3个月;4)无既往治疗;5)年龄在18-25岁之间的女性患者。
1.1.2排除标准[17]
1)接受其他治疗;2)有膝关节手术史、髌骨脱位或踝关节/髋关节损伤史;3)有半月板或膝关节韧带损伤或膝关节任何其他损伤;4)骶髂关节疼痛;5)患有任何神经或心血管疾病。
本研究经西安体育学院伦理委员会审核批准 (No. XAIPE2024024)。所有受试者均自愿参与并签署知情同意书。
1.2干预措施
本研究在西安体育学院进行,干预时间为2023年12月-2024年1月,实验组干预方式为MCE;对照组进行假干预。
1.2.1假干预训练
假干预方案包括上肢和躯干练习,不影响下肢功能,参考Emamvirdi[18]等人方案。卷腹:仰卧,髋膝屈曲90度,肩抬离地面,每组10次,3组/周。俯卧伸展:俯卧,抬起躯干并缓慢返回,每组10次,3组/周。肱二头肌训练:屈肘握住毛巾卷,肘部靠在躯干上进行旋后,每组15次,3组/周。肱三头肌训练:伸肘握住毛巾卷进行旋前,每组15次,3组/周。胸肌牵伸:立位,肩部外展,前臂靠墙,身体前倾,每次保持15秒,3次/周。
1.2.2 MCE
MCE组参考Emamvirdi等人的研究[18-20]。1-2周,深蹲,侧向弹力带行走,立位髋外展,弹力带阻力深蹲,向前弓步。3-4周,深蹲,侧向弹力带行走,立位髋外展,弹力带阻力深蹲,向前弓步,BOSU球深蹲,BOSU球单腿平衡训练。5-6周,BOSU球深蹲,BOSU球单腿平衡训练,单腿屈曲30度平衡训练,BOSU球弹力带深蹲,改良弓箭步,罗马尼亚单腿硬拉,无跳跃侧向运动,髋关节侧向旋转。以上每个动作12~20次/组,重复2~3组,3次/周,每次40min。通过改变支撑面、变换训练动作或增加阻力等提高难度。训练时给予口头提示,保持膝关节朝向正前方,不要旋转。
1.3测量指标
1.3.1表面肌电图
使用无线遥感表面肌电图测试仪(NORAXON)收集单腿下蹲(single-leg squat,SLS)期间臀中肌和臀大肌的肌电数据。准备过程:去除毛发,清洁皮肤以提高导电性。电极放置:臀中肌电极位于髂骨和大转子中点。臀大肌电极位于骶椎和大转子中点。测试流程:受试者患腿进行SLS,双脚与肩同宽,手放臀部。按指令下蹲:“准备”,“1”达到最大髋关节屈曲,“2”蹲至60度,保持5秒,重复3次。选择振幅高、噪声小的2秒范围内均方根("Root Mean Square, RMS)值以进行分析。将臀大肌和臀中肌RMS值进行标准化,以臀中肌和臀大肌的最大等长收缩时(Maximal"Voluntary Isometric Contractions,MVIC)的RMS为标准[21]。臀中肌MVIC:健侧卧位,测试装置固定在外踝上方,最大外展力维持6秒。臀大肌MVIC:俯卧位,膝关节90度,测试装置连接大腿后端,最大臀部伸展力维持6s[22,23]。取6s收缩过程中,中间2s信号值,共测3次,取平均值作为肌电标准化基准。
1.3.2 DKV
使用两台摄像机记录SLS的动作。相机1和相机2分别放置于拍摄对象前方和侧方3 m处膝盖高度。标记物分别放置于患侧膝关节和踝关节中心、髂前上棘至膝关节标记点连线中点,由同一测试人员完成,三个点形成的两条直线的夹角即为DKV角。受试者被要求进行SLS,躯干挺直,保持平衡,5秒内下蹲,膝关节屈曲60度,受试者下蹲到最低点时,测量受试者膝关节的DKV角[24],重复3次,取平均值。
1.3.3 VAS
VAS是一种测量疼痛的标准化工具。受试者在直尺上标出疼痛程度相应的位置,工作人员记录数值来量化疼痛水平。
1.3.4"Lysholm量表
Lysholm量表满分100分,分数越高功能越好。评估内容包括:疼痛、跛行、支持、下蹲、肿胀、上楼、绞索和稳定性。
1.3.5 Y平衡
Y平衡装置包括一个中央平台和三个定向游标尺,测试之前首先测量患肢长度(髂前上棘到内踝距离),受试者患腿支撑,健腿尽可能向三个方向最大距离伸展:即前侧(A)、后内侧(PM)和后外侧(PL),测3次,取平均值。以下肢长度的百分比表示。测试过程中失去平衡或非负重脚触地,视为无效[25]。
1.4统计分析
采用SPSS 27.0进行数据分析。计量资料满足正态性分布,组间比较使用独立样本t检验,组内比较采用配对样本t检验,以均数±标准差表示,Plt;0.05为显著性水平。
2.研究结果与分析
2.1受试者一般资料
本研究最终纳入36人,两组的年龄、体重、身高、BMI无统计学差异(P>0.05),具有可比性(见表一)。
2.1表面肌电
两组臀大肌肌电均方根比较:干预前,两组无显著性差异,干预6周后,MCE组臀大肌肌电均方根显著提高(P<0.001),且MCE组臀大肌肌电均方根显著高于对照组(P<0.001),对照组干预后无显著变化(见表2)。
两组臀中肌肌电均方根比较:干预前,两组无显著性差异,干预6周后,MCE组臀中肌肌电均方根显著提高(P<0.001),且MCE组臀中肌肌电均方根显著高于对照组(P=0.003),对照组干预后无显著性变化(见表3)。
2.2 DKV
干预前,两组无显著性差异,干预6周后,MCE组DKV角显著降低(P<0.001),且MCE组DKV角显著低于对照组(P<0.001),对照组干预后无显著性变化。(见表4)
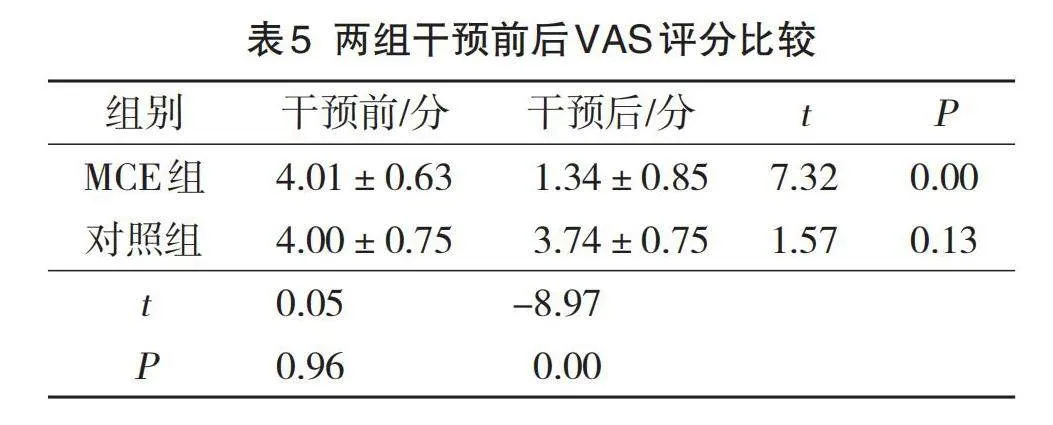
2.3 VAS
干预前,两组无显著性差异,干预6周后,MCE组VAS评分显著降低(P<0.001),且MCE组VAS评分显著低于对照组(P<0.001),对照组干预后无显著性变化。(见表5)
2.4 Lysholm
干预前,两组无显著性差异,干预6周后,MCE组Lysholm评分显著提高(P<0.001),且MCE组显著优于对照组(P<0.001),对照组干预后无显著性变化。(见表6)
2.5 Y平衡
前方比较:干预前和干预6周后,两组前方得分无显著性差异,干预6周后,MCE组的前方得分较干预前显著提高(P=0.006),对照组干预后无显著性变化。(见表7)
后内侧比较:干预前和干预6周后,两组无统计学差异,与干预前相比,干预6周后两组均无显著性变化。(见表7)
后外侧比较:干预前和干预6周后,两组无统计学差异,与干预前相比,干预6周后两组均无显著性变化。(见表7)
3.讨论
本研究结果表明,MCE可以增强PFP女大学生臀部肌肉激活、降低DKV角,改善下肢姿势控制、减轻疼痛和提高膝关节功能。
肌肉激活反映肌肉刚度变化和运动单位的募集水平。与无PFP者相比,PFP患者表现为臀肌激活时间延迟和缩短,这使髋、膝关节无法保持中立位置,从而导致髋关节内收、内旋以及膝关节外翻[26]。其他研究也表明,臀肌激活与DKV角之间存在相关性,在SLS时,臀肌激活程度越高,DKV角越低[27]。本研究与该研究结果一致。6周的MCE增加了PFP受试者臀中肌和臀大肌的激活水平,同时单腿下蹲时的DKV角也显著降低。在肢体进行运动时,肌肉激活通常先于动作,以对抗由反应引起的失稳。这种预先计划的激活,被称为前馈控制,由中枢神经系统支配[28]。在PFP患者中,前馈控制减弱,导致在动态运动中自发收缩肌肉的能力降低。因此,难以根据负荷的变化适当、及时地调整肌肉激活强度,导致下肢稳定性下降[29]。Goto等[26]对PFP受试者单腿着陆肌电图研究发现臀中肌和臀大肌的激活普遍降低,提示PFP患者前馈控制较差。Muyor[30]研究表明,单腿下蹲、向前弓步和侧向运动能有效地激活臀肌,单蹲下蹲的激活水平最高。单腿下蹲和向前弓步是本实验练习的关键,训练最初是在稳定的平面上进行,之后借助BOSU球、弹力带增加训练难度。这些动作可以有效地激活臀肌,改善前馈控制。因此,我们认为MCE提高了PFP患者前馈控制,增加了肌肉的激活效率,从而降低了DKV角。
Myer等[31]发现,如果在着陆阶段膝关节外展力矩超过15.4 N,则髌股疼痛发展的风险为6.8%,而低于此阈值的风险仅为2.9%。髌股疼痛可影响膝关节的日常功能,如上下楼梯、下蹲等。在上述讨论中,我们提到了臀肌的激活降低了DKV角。DKV角的降低能够减轻膝关节外展力矩。因此,本研究中MCE降低疼痛和提高膝关节Lysholm评分可能是由于增加了臀肌激活水平,降低DKV角,减少髌股关节的压力,因为缓解了疼痛,改善了膝关节功能。这与Emamvirdi
等人[18]的研究结果一致,他的研究表明以髋部为主的运动控制训练能够使PFP患者在功能活动时疼痛水平降低。
Y平衡是评估下肢动态姿势控制的一种可靠、有效的工具。Y平衡得分的下降与下肢损伤的发生有关,并已被用于检测PFP患者的姿势控制[32-34]。神经肌肉效率的下降,可能会影响下肢动态的控制[34]。Y平衡的触及距离反应神经肌肉控制,距离的增加反映了神经肌肉控制改善[35]。本研究结果显示,经MCE治疗后,PFP受试者的姿势控制得到改善。具体来说,前方触及距离显著增加,而后外侧和后内侧距离虽有改善,但无统计学差异。Robison[36]学者表明,测试中膝关节屈曲角度与前方伸展距离显著相关。因此,6周干预后前方距离的增加可能源于运动过程中膝关节屈曲角度的提高。膝关节屈曲角度与DKV角存在相关性。研究表明在SLS时膝关节屈曲角度降低将导致DKV角代偿性增加,以吸收地面反作用力。相反,在SLS中膝屈曲角增大,则DKV角降低[37]。Christine[38]的研究也证实,使用低屈曲着陆模式的女性表现出更大的膝关节外翻角度,相反,高屈曲着陆的女性表现出更有效的矢状面控制,和更小的膝外翻角度。也有研究称臀中肌激活程度和力量与前方伸展距离相关,臀中肌激活水平在前方伸展时最高[38,39]。在上述讨论中,我们提到了MCE可以显著提高PFP受试者臀肌的激活水平,降低DKV。因此,Y平衡测试中前伸距离的增加可能得益于臀肌激活以及DKV角度的降低。我们的研究证实了Robison[36]和Christine[38]等人得出的结论。虽然干预后两组间的前伸距离差异无统计学意义,但MCE组比对照组均值更大,MCE组为得分为73.90±6.99,对照组得分为69.86±8.16,实验组增加了9.5%,而对照组相比干预前有下降趋势。这说明以髋关节为核心的MCE能有效提高下肢动态平衡,增加前伸距离。在本研究中,虽然干预6周后实验组的后内侧和后外侧方向无统计学意义上的变化,但其变化量已超过后内侧和后外侧伸展距离的最小可检测变化值(minimal detectable change ,MDC),另外,后外侧最终得分相比干预前增加了5.28%,后内侧得分相比干预前增加了5.33%。研究表明,在Y平衡中,髋关节外展肌和膝关节屈肌强度与后内侧距离呈正相关,髋关节伸肌和膝关节屈肌强度与后外侧距离呈正相关[39]。更高水平的肌肉激活被认为会增强肌肉力量。有学者建议,在运动过程中肌肉激活应至少是40%到60%的MVIC,以达到力量的增加[40]。据研究表明,单腿下蹲时臀中肌激活为48%至82%的MVIC。臀大肌在单腿深蹲中也同样被最大程度地激活[41,42]。因此推断以髋关节为中心的MCE增加了臀肌的激活,促进了髋关节伸肌和外展肌力量的提高,从而进一步改善了Y平衡中后内侧和后外侧方向的距离。导致MCE组干预前后在后内侧和后外侧两个方向上缺乏统计学变化的原因可能是实验周期较短。此外,膝关节屈肌强度也是预测Y平衡中三个方向最大距离的关键因素,本实验旨在增强髋部肌肉激活,对膝关节屈肌激活和肌力的影响较小。这可能是缺乏统计学意义的另一因素。
本研究利用MCE 对PFP女大学生进行干预,验证了MCE治疗女性PFP的有效性,为临床治疗PFP提供了康复方案和理论依据。本试验也存在一些不足之处,首先本研究样本量相对较少,另外本研究周期较短,也缺乏长期的随访研究。因此未来还需要进一步扩大研究,完善试验设计。总的来说,MCE可有效激活PFP患者臀大肌和臀中肌,降低DKV角,改善疼痛,提高膝关节功能,增强下肢姿势控制。
参考文献
[1] NIE"Qi, YU"Yan, YUAN"Zhi, et al. Effects of adding neuromuscular electrical stimulation to functional training on muscle recruitment, pain reduction, and knee joint function in patellofemoral pain syndrome patients[J]. Medicine, 2024, 103(3): e36095.
[2]THOMEÉ R, AUGUSTSSON"J, KARLSSON"J. Patellofemoral pain syndrome: a review of current issues[J]. Sports medicine, 1999, 28: 245-262.
[3]WITVROUW"E, CALLAGHAN"M J, STEFANIK"J J, et al. Patellofemoral pain: consensus statement from the 3rd International Patellofemoral Pain Research Retreat held in Vancouver, September 2013[J]. British journal of sports medicine, 2014, 48(6): 411-414.
[4]BOLING M, PADUA D, MARSHALL S, et al. Gender differences in the incidence and prevalence of patellofemoral pain syndrome[J]. Scandinavian journal of medicine amp; science in sports, 2010, 20(5): 725-730.
[5]BLOND L, HANSEN L. Patellofemoral pain syndrome in athletes: a 5.7-year retrospective follow-up study of 250 athletes[J]. Acta Orthop Belg, 1998, 64(4): 393-400.
[6]CROSSLEY K M. Is patellofemoral osteoarthritis a common sequela of patellofemoral pain?[J]. British journal of sports medicine, 2014, 48(6): 409-410.
[7]SINCLAIR J, SELFE J. Sex differences in knee loading in recreational runners[J]. Journal of biomechanics, 2015, 48(10): 2171-2175.
[8]DUVIGNEAUD N, BERNARD E, STEVENS V, et al. Isokinetic assessment of patellofemoral pain syndrome: a prospective study in female recruits[J]. Isokinetics and Exercise Science, 2008, 16(4): 213-219.
[9]"NEAMATALLAH Z, HERRINGTON L, JONES R. An investigation into the role of gluteal muscle strength and EMG activity in controlling HIP and knee motion during landing tasks[J]. Physical Therapy in Sport, 2020, 43: 230-235.
[10]POWERS C M. The influence of altered lower-extremity kinematics on patellofemoral joint dysfunction: a theoretical perspective[J]. Journal of Orthopaedic amp; Sports Physical Therapy, 2003, 33(11): 639-646.
[11]PAL S, DRAPER C E, FREDERICSON M, et al. Patellar maltracking correlates with vastus medialis activation delay in patellofemoral pain patients[J]. The American journal of sports medicine, 2011, 39(3): 590-598.
[12]PATTYN E, VERDONK P, STEYAERT A, et al. Vastus medialis obliquus atrophy: does it exist in patellofemoral pain syndrome?[J]. The American journal of sports medicine, 2011, 39(7): 1450-1455.
[13]HWANG P S, WILLOUGHBY"D S. Mechanisms behind blood flow–restricted training and its effect toward muscle growth[J]. The Journal of Strength amp; Conditioning Research, 2019, 33: S167-S179.
[14]LAFRANCE S, OUELLET P, ALAOUI R, et al. Motor control exercises compared to strengthening exercises for upper-and lower-extremity musculoskeletal disorders: a systematic review with meta-analyses of randomized controlled trials[J]. Physical Therapy, 2021, 101(7): pzab072.
[15]CROSSLEY K M, VAN MIDDELKOOP M, CALLAGHAN M J, et al. 2016 Patellofemoral pain consensus statement from the"4th International Patellofemoral Pain Research Retreat, Manchester. Part 2: recommended physical interventions (exercise, ta**, bracing, foot orthoses and combined interventions)[J]. British journal of sports medicine, 2016, 50(14): 844-852.
[16]MAGALHÃES E, FUKUDA T Y, SACRAMENTO S N, et al. A comparison of hip strength between sedentary females with and without patellofemoral pain syndrome[J]. journal of orthopaedic amp; sports physical therapy, 2010, 40(10): 641-647.
[17]FUKUDA T Y, MELO W P, ZAFFALON B M, et al. Hip posterolateral musculature strengthening in sedentary women with patellofemoral pain syndrome: a randomized controlled clinical trial with 1-year follow-up[J]. Journal of orthopaedic amp; sports physical therapy, 2012, 42(10): 823-830.
[18]EMAMVIRDI M, LETAFATKAR A, KHALEGHI TAZJI M. The effect of valgus control instruction exercises on pain, strength, and functionality in active females with patellofemoral pain syndrome[J]. Sports health, 2019, 11(3): 223-237.
[19]"FORD K R, NGUYEN A D, DISCHIAVI S L, et al. An evidence-based review of hip-focused neuromuscular exercise interventions to address dynamic lower extremity valgus[J]. Open access journal of sports medicine, 2015: 291-303.
[20]LETAFATKAR A, RABIEI P, AFSHARI M. Effect of neuromuscular training augmented with knee valgus control instructions on lower limb biomechanics of male runners[J]. Physical Therapy in Sport, 2020, 43: 89-99.
[21]HATEFI M, HADADNEZHAD M, SHOJAEDIN S, et al. The effects of the Posterior X Ta** versus augmented feedback on lower-extremity kinematic and muscle activity pattern during unilateral weight-bearing activities in men with tibiofemoral varus malalignment[J]. Journal of Experimental Orthopaedics, 2023, 10(1): 70.
[22]STASTNY P, GOŁAŚ A, BLAZEK D, et al. A systematic review of surface electromyography analyses of the bench press movement task[J]. PloS one, 2017, 12(2): e0171632.
[23]FOLEY R C A, BULBROOK B D, BUTTON D C, et al. Effects of a band loop on lower extremity muscle activity and kinematics during the barbell squat[J]. International journal of sports physical therapy, 2017, 12(4): 550.
[24] GWYNNE C R, CURRAN S A. Two-dimensional frontal plane projection angle can identify subgroups of patellofemoral pain patients who demonstrate dynamic knee valgus[J]. Clinical Biomechanics, 2018, 58: 44-48.
[25]韩征强,张金棒.Y平衡测试在评价CUBA女子篮球运动员神经肌肉训练效果中的应用[J].平顶山学院学报, 2023, 38(2):113-117.
[26]GOTO S, AMINAKA N, GRIBBLE P A. Lower-extremity muscle activity, kinematics, and dynamic postural control in individuals with patellofemoral pain[J]. Journal of sport rehabilitation, 2018, 27(6): 505-512.
[27]MEIRA E P, BRUMITT J. Influence of the hip on patients with patellofemoral pain syndrome: a systematic review[J]. Sports health, 2011, 3(5): 455-465.
[28]DAVERGNE T, GRELIER A, OSTERTAG A, et al. Capacity for extra-spinal muscular effort in chronic non-specific low back pain: A cross-sectional case-control study of 192 patients and 335 controls[J]. Joint bone spine, 2024, 91(2): 105663
[29]HOLLMAN J H, GALARDI C M, LIN I H, et al. Frontal and transverse plane hip kinematics and gluteus maximus recruitment correlate with frontal plane knee kinematics during single-leg squat tests in women[J]. Clinical biomechanics, 2014, 29(4): 468-474.
[30]MUYOR J M, MARTÍN-FUENTES I, RODRÍGUEZ-RIDAO D, et al. Electromyographic activity in the gluteus medius, gluteus maximus, biceps femoris, vastus lateralis, vastus medialis and rectus femoris during the Monopodal Squat, Forward Lunge and Lateral Step-Up exercises[J]. PLoS One, 2020, 15(4): e0230841.
[31]MYER G D, FORD K R, DI STASI S L, et al. High knee abduction moments are common risk factors for patellofemoral pain (PFP) and anterior cruciate ligament (ACL) injury in girls: is PFP itself a predictor for subsequent ACL injury?[J]. British journal of sports medicine, 2015, 49(2): 118-122.
[32]NILSTAD A, KROSSHAUG T, MOK K M, et al. Association between anatomical characteristics, knee laxity, muscle strength, and peak knee valgus during vertical drop-jump landings[J]. journal of orthopaedic amp; sports physical therapy, 2015, 45(12): 998-1005.
[33]HARTLEY E M, HOCH M C, BOLING M C. Y-balance test performance and BMI are associated with ankle sprain injury in collegiate male athletes[J]. Journal of science and medicine in sport, 2018, 21(7): 676-680.
[34]SMITH C A, CHIMERA N J, WARREN M. Association of y balance test reach asymmetry and injury in division I athletes[J]. Medicine and science in sports and exercise, 2015, 47(1): 136-141.
[35] NORRIS B, TRUDELLE-JACKSON E. Hip-and thigh-muscle activation during the star excursion balance test[J]. Journal of sport rehabilitation, 2011, 20(4): 428-441
[36]ROBINSON R , GRIBBLE P".Kinematic predictors of performance on the Star Excursion Balance Test.[J].Journal of Sport Rehabilitation, 2008, 17(4):347-357.
[37]NELSON S, WILSON C S, BECKER J. Kinematic and kinetic predictors of Y-balance test performance[J]. International journal of sports physical therapy, 2021, 16(2): 371.
[38]"POLLARD C D, SIGWARD S M, POWERS C M. Limited hip and knee flexion during landing is associated with increased frontal plane knee motion and moments[J]. Clinical biomechanics, 2010, 25(2): 142-146.
[39]LEE D K, KIM G M, HA S M, et al. Correlation of the Y-balance test with lower-limb strength of adult women[J]. Journal of physical therapy science, 2014, 26(5): 641-643.
[40]ANDERSEN L L, MAGNUSSON S P, NIELSEN M, et al. Neuromuscular activation in conventional therapeutic exercises and heavy resistance exercises: implications for rehabilitation[J]. Physical therapy, 2006, 86(5): 683-697.
[41]DISTEFANO L J, BLACKBURN J T, MARSHALL S W, et al. Gluteal muscle activation during common therapeutic exercises[J]. Journal of orthopaedic amp; sports physical therapy, 2009, 39(7): 532-540.
[42]BOLGLA L A, UHL T L. Electromyographic analysis of hip rehabilitation exercises in a group of healthy subjects[J]. Journal of Orthopaedic amp; Sports Physical Therapy, 2005, 35(8): 487-494.
