The emerging role of sentinel lymph node biopsy in oral cavity and oropharyngeal carcinomas
2024-05-18KimberlyChanMohamadSaltagiKarenChoi
Kimberly Chan, Mohamad Saltagi, Karen Y.Choi
1Department of Otolaryngology - Head and Neck Surgery, The Pennsylvania State University College of Medicine, Hershey, PA 17033, USA
2Department of Otolaryngology - Head and Neck Surgery, University of Texas MD Anderson Cancer Center, Houston, TX 77030, USA.
Abstract Management of clinically negative necks (cN0) in oral cavity (OCSCC) and oropharyngeal (OPSCC) squamous cell carcinoma (SCC) has evolved over time.Historically, the clinically negative neck has been managed with elective neck dissection (END) or observation, but more recently sentinel lymph node biopsy (SLNB) has emerged as a technique to detect occult metastases.In this review, we will discuss the role of SLNB in early-stage OCSCC and in the management of OPSCC.
Keywords: Sentinel lymph node biopsy, oral cavity cancer, oropharyngeal cancer, neck dissection, occult metastasis, false negative rate
INTRODUCTION
Oral cavity and oropharyngeal carcinomas account for about 3% of cancers in the United States and slightly less than half of head and neck cancers[1,2].These tumors often spread to regional lymph nodes in the neck and are the most important prognosticator for survival, decreasing survival by 50%[3].As such, management of regional metastasis is crucial and often involves multimodality treatment[3-5].When there is clinically evident nodal disease in the neck, guidelines for management are well-defined with treatment options including surgery (if deemed resectable) followed by adjuvant treatment, or definitive nonsurgical management[6].However, there is some debate surrounding the optimal management of the clinically negative neck (cN0), i.e., when there is no evidence of nodal metastases on physical exam or radiographic imaging.This is an important consideration, as the rate of occult metastasis in oral cavity and oropharyngeal squamous cell carcinoma (SCC) is 20%-30% in the ipsilateral neck[3,6-9].In the contralateral neck, the rate of occult metastases ranges from 0.9%-36% for oral cavity squamous cell carcinoma (OCSCC)and 16%-21% for oropharyngeal squamous cell carcinoma (OPSCC)[7-11].In the last several decades, the implementation of sentinel lymph node biopsy (SLNB) as a technique to evaluate the cN0 neck in oral cavity and oropharyngeal carcinoma has been studied.This chapter will review the history and technique of SLNB in oral cavity and oropharyngeal SCC.
Oral cavity SCC and management of the cN0 neck: history
Historically, the cN0 neck in early-stage OCSCC (cT1-T2) was managed with watchful waiting, and therapeutic neck dissection was reserved for nodal relapse[6,12].Proponents of this approach argued that an elective neck dissection (END) led to high rates of overtreatment and conferred additional morbidity to patients, especially if a radical or modified radical neck dissection was performed[6,12].However, numerous studies have shown a survival benefit and improved disease control in patients who undergo END as opposed to watchful waiting for early-stage OCSCC [Table 1][6,12,13].
A randomized, prospective study by D’Cruzet al.was the first to show the prognostic benefit of END for early-stage OCSCC[6].Patients with cT1-2, N0 OCSCC were randomized to undergo END or watchful waiting with a therapeutic neck dissection if nodal recurrence occurred[6].At 3-year follow-up, there was improved DFS and overall survival (OS) in the END cohort [Table 1][6].Thus, the management of cN0 disease in early-stage OCSCC shifted towards END for tumors with a depth of invasion (DOI) ≥ 4 mm instead of watchful waiting[6,13,14].However, it is important to note that several studies suggested that thinner tumors (2 to 4 mm) in oral tongue and floor of mouth (FOM) subsites showed high rates of nodal metastases (41.7% and 42.1%, respectively) and may also warrant elective neck management[15,16].
Nonetheless, it is well-established that rates of occult nodal disease for early-stage oral cancer range between 20%-30%, meaning 70%-80% of patients may be overtreated by an END[3,4].Studies have demonstrated that patients who undergo SLNB report better neck function compared to patients who undergo END[3,17-21].This has led to efforts to develop a better way to evaluate and identify patients who are at higher risk of occult disease without subjecting them to more morbidity than needed.As a result, SLNB has been of immense interest in this patient cohort.
SENTINEL LYMPH NODE BIOPSY
Background, terminology & important concepts
SLNB relies on the natural, predictable step-wise progression of cancer from a primary site to nearby lymph nodes[22].A sentinel node (SN) is the first echelon lymph node that drains from the site of the primary tumor and is most likely to harbor metastasis; this may or may not be the closest node to the tumor, and there may be multiple SNs[22].Thus, excising and evaluating these SN(s) can provide important diagnostic information[22].Unlike END, SLNB is used for diagnostic purposes to evaluate the nodal status and is not considered a therapeutic intervention.
Brief history
The concept of SLNB was described as early as the 1970s in penile cancer to guide whether inguinal-femoral lymph node dissection was indicated[23,24].SLNB gained further popularity after Mortonet al.described SLNB techniques for evaluating early-stage cutaneous melanomas[25].In 1996, Alex and Krag establishedSLNB as a safe, accurate, minimally invasive, and feasible procedure[26].Today, SLNB is part of the standard of care for breast cancer and cutaneous malignant melanoma, and its use continues to expand[23,25].
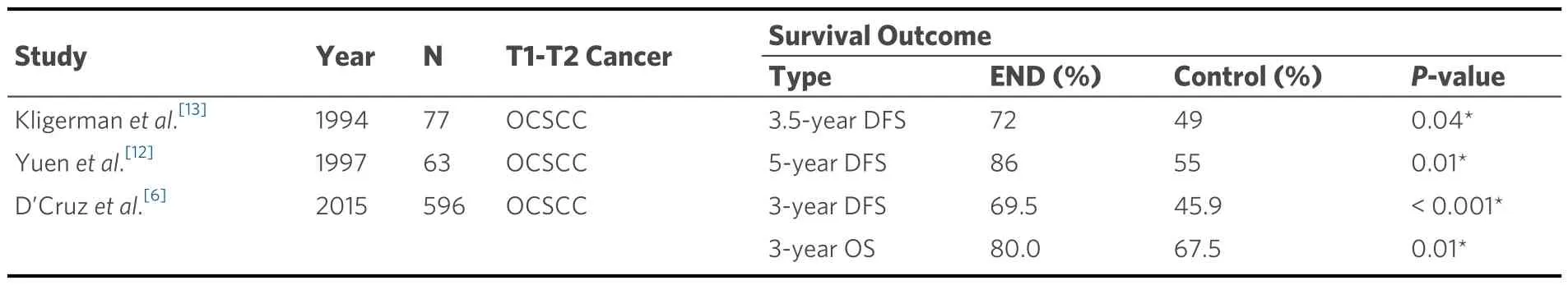
Table 1.Survival outcomes in patients with T1-T2 OCSCC who underwent END compared to patients in the control group of each study
The Multicenter Selective Lymphadenectomy Trial 1 (MSLT-1) was a multi-institutional randomized controlled trial that showed the survival benefit of SLNB in primary cutaneous malignant melanoma[27].They reported a significantly higher 5-year DFS among patients who underwent wide excision followed by SLNB compared to patients who underwent wide excision followed by observation[27].Patients with negative SNs had significantly higher 5-year DFS and melanoma-specific survival compared to patients with positive SNs[27].In their subsequent phase III randomized control trial, Multicenter Selective Lymphadenectomy Trial II (MSLT-II), patients with positive SNs who had an immediate completion lymphadenectomy had improved regional disease control but not melanoma-specific OS[28].Therefore, the treatment of cutaneous malignant melanoma shifted away from proceeding with a completion lymphadenectomy.Much of the treatment paradigm implemented for SLNB in OCSCC is adopted from our experience with cutaneous malignant melanoma.
Feasibility & reliability of SLNB in early-stage OCSCC
Over the last several decades, SLNB has emerged as a technique to help evaluate the neck for occult disease in oral SCC.Early studies established the feasibility, reliability, and reproducibility of SLNB in oral SCC.Paleriet al.published a meta-analysis in 2005 on SLNB for OCSCC and OPSCC and calculated a pooled sensitivity of 92.6% for detecting occult neck disease[29].A similar study by Thompsonet al.in 2012 found a pooled negative predictive value (NPV) of 96%, with an even more favorable NPV of 98% among a subset of patients with early-stage OCSCC[30].These studies paved the way for further investigations evaluating the use of SLNB in OCSCC.
Subsequently, several trials have investigated the sensitivity, NPV, and false negative rate (FNR) of SLNB in early-stage oral cancers.Rosset al.were the first to conduct a multicenter trial in the United Kingdom evaluating SLNB for T1-T2 OCSCC and OPSCC, comparing patients who had SLNB alone to patients who had SLNB followed by an immediate END[31].They reported a sentinel node identification rate of 93%(125/134), with 34% (41/125) of these patients showing occult disease[31].They also reported an overall sensitivity after a 24-month follow-up of 93% with a false negative rate (FNR) of 7.1%[31,32].Civantoset al.evaluated whether a negative SN would accurately predict the negativity of the other at-risk cervical lymph nodes[32].The overall FNR was 9.8%, but notably, it was as high as 25% in the FOM subsite alone[32].The authors highlighted technical challenges associated with performing a SLNB in FOM primary tumors,noting that the primary tumor radioactivity may obscure nearby level 1 radioactive SNs, making it difficult to accurately identify a SN in that nodal basin[32].The Sentinel European Node Trial (SENT) was one of the largest multicenter prospective trials on SLNB for OCSCC and OPSCC[33].They reported a FNR of 14%, a rate similar to that reported for cutaneous malignant melanoma[33,34].Of note, when comparing this to rates of regional recurrence after END (9%-20%)[27,35,36], a FNR of 14% seems comparable and within the accepted range.Sundaramet al.compared patients with T1-T3 OCSCC who underwent SLNB, with one cohort proceeding with completion neck dissection for positive SNs and the other cohort proceeding to neck dissection regardless of SLNB results[17].They found that 22 of 30 patients who underwent a neck dissection,regardless of SLNB results, had no positive lymph nodes on surgical pathology, concluding that neck dissection had been unnecessary in these patients[17].More recent randomized controlled trials by Garrelet al.and Hasegawaet al.reported FNRs of 9.1% and 15.1%, respectively[18,21][Table 2].
Survival outcomes in SLNB in early-stage OCSCC
Up to this point, many studies established the feasibility, reliability, and reproducibility of SLNB in OCSCC.However, much of the published data evaluating outcomes were from small single-institution retrospective studies, all of which did not find a significant difference in survival outcomes between SLNB and END[Fanet al., Alvarezet al., Crameret al., Moya-Planaet al., Table 3][39-42].
29. Pigeon: Pigeons are birds having a heavy body and short legs. They can be wild or domesticated86 (WordNet). Since pigeons are often domesticated birds, they are associated with the desire to return home in dream interpretations88.
More recently, several multi-institutional prospective randomized controlled trials have directly evaluated and compared outcomes of SLNB to END [Garrelet al., Hasegawaet al., Table 3][18,21].A multicenter phase III randomized controlled trial by Garrelet al.randomized early-stage OC/OPSCC patients to undergo END or SLNB followed by an END based on SN positivity[18].The study utilized a non-inferiority margin of 10% with a primary endpoint of 2-year neck node recurrence-free survival (RFS)[18].The authors concluded that SLNB was oncologically equivalent to END and suggested that SLNB should be established as the standard of care approach for cN0 early oral cancers [Table 3][18].One note of important significance is that 12.5% of patients had oropharyngeal disease [Table 2].Understanding the significant difference in prognosis between HPV-associated OPSCC and OCSCC, the inclusion of this mixed cohort in the analysis makes it more challenging to discern definitive conclusions.
Another multi-institutional prospective randomized trial by Hasegawaet al.compared the equivalence of SLNB to END in patients with early-stage OCSCC.Patients were randomized to undergo END or SLNB followed by supraomohyoid neck dissection if SNs were positive[21].The study used a non-inferiority margin of 12% with a primary endpoint of 3-year OS.In addition to no difference in 3-year DFS or OS [Table 3],they demonstrated better neck functionality scores in the SLNB group relative to the END group[21].
Although these prospective randomized trials provided significant results in an area with a paucity of highlevel clinical data, there are notable questions to the study design and statistical analyses that prompt additional investigation to evaluate the true oncologic equivalence or non-inferiority of SLNB compared to END[39,43].This led to the design of an international cooperative group multi-institutional phase II/III prospective, randomized controlled trial comparing SLNB versus END in early-stage oral cavity cancer(ClinicalTrials.gov Identifier: NCT04333537).The phase II objective is to determine whether patientreported neck and shoulder function is superior with SLNB compared to END at 6 months after surgery.The phase III primary objective is to determine whether DFS is non-inferior with SLNB compared to END using a non-inferiority margin of 5%.All patients in this study will undergo initial staging with a positron emission tomography/computed tomography (PET/CT) scan and will be excluded if this test is positive.However, these excluded patients will remain in a registry in order to compare the images with final neck pathology findings.This will provide valuable information on the sensitivity and specificity of PET/CT as a staging imaging modality for early-stage OCSCC.
Sentinel lymph node biopsy: technique
SLNB begins either the day before surgery or the day of surgery with injection of a radiotracer peritumorally at 2-4 quadrants [Figure 1].The tracer contains technetium-99 (99mTc) and comes in different formulations,such as sulfur colloid (99mTc-sulfur colloid), albumin colloid (99mTc-albumin), tilmanocept (99mTctilmanocept), and nanocolloid (99mTc-nanocolloid).The use of the different tracers can depend on the availability of the formulation in different parts of the world.Each formulation travels via passive diffusion and has different transit properties[44,45].Compared to99mTc-tilmanocept,99mTc-sulfur colloid and99mTcalbumin travel slower due to their larger particle size, which can affect the visualization of SNs near the injection site[45].99mTc-tilmanocept is emerging as a promising radiotracer due to its high sensitivity and specificity[46].99mTc-tilmanocept clears from the injection site more quickly and has more effective uptake since it binds to CD206 receptors on antigen-presenting cells within the lymph nodes[45,47,48].99mTctilmanocept has shown lower FNR (2.56%) compared to99mTc-sulfur colloid (9.8%) when utilized in oral cavity cancer and has similar accuracy in detecting SNs compared to99mTc-nanocolloid[32,49,50].However, one limitation of99mTc-tilmanocept is its low radioactive uptake compared to99mTc-nanocolloid may require injection of a higher dose to accurately identify SNs[51].
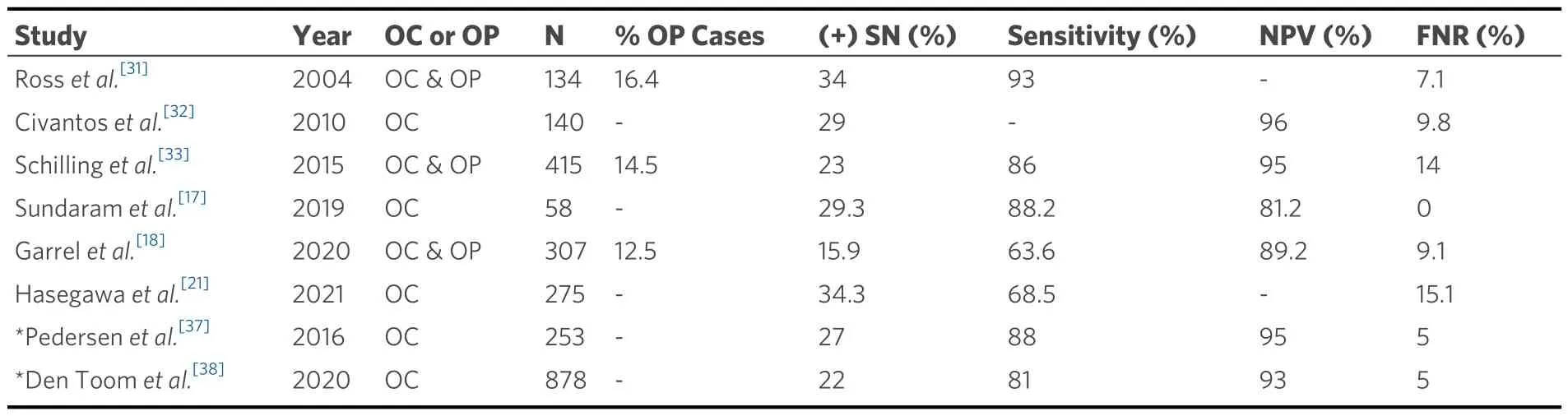
Table 2.Feasibility and reliability of SLNB in early oral cavity and oropharyngeal squamous cell carcinoma
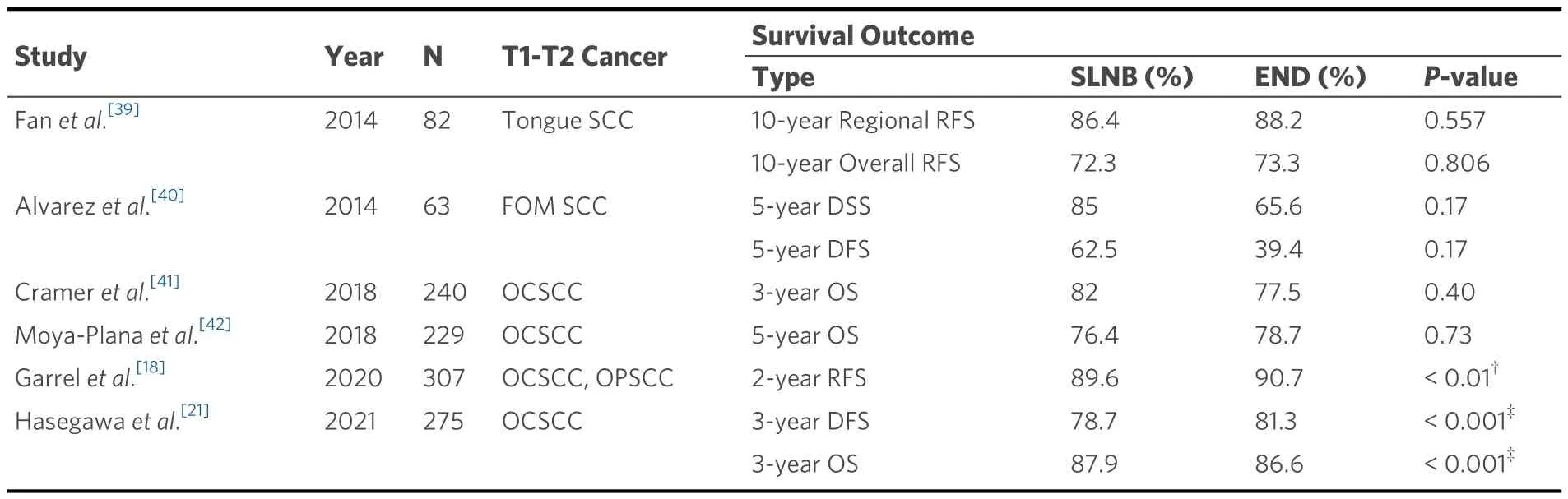
Table 3.Survival Outcomes in SLNB in early-stage (T1-T2) oral cavity (OCSCC) and oropharyngeal (OPSCC) squamous cell carcinoma (SCC)
It can take at least 10 to 30 min for the SN to adequately uptake the tracer.Due to the half-life of99mTc (~6 h)[22,52-54], timing of the tracer injection is important to allow sufficient time for uptake in SNs and for the tracer to remain radioactive for detection during surgery.Some studies suggest performing surgery within 10 to 16 hours of the injection[22,54].Other studies have shown no difference in FNR or ability to detect SNs when the tracer was injected more than 12 to 30 h before surgery[32,49].
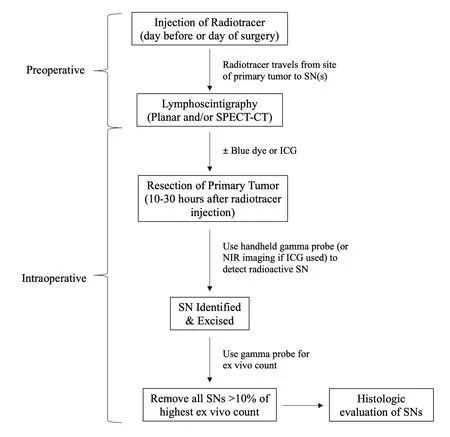
Figure 1.Flow diagram of standard SLNB technique.If a hybrid tracer is used, the ICG is injected together with the radiotracer.SN:sentinel node; SPECT/CT: single photon electron computed tomography with computed tomography scan; NIR: near-infrared; ICG:indocyanine green.
SNs are mapped with planar lymphoscintigraphy with or without single-photon emission computerized tomography (SPECT)[4,55,56].Planar lymphoscintigraphy provides two-dimensional images of the quantity,laterality, and location of the nodes.SPECT involves a three-dimensional image that can be fused with a CT scan (SPECT-CT) to provide more detailed visualization of lymph nodes in relation to anatomical structures that can aid in improved identification intraoperatively[52].In addition, SPECT-CT has been shown to identify more SNs compared to planar lymphoscintigraphy and can better guide the location and extent of the incision for the SLNB[52,57,58].
Blue dye (e.g., methylene blue, isosulfan blue) can be injected at the primary tumor site to aid in gross intraoperative visualization of lymphatic drainage to SNs, although it has not been shown to significantly increase the sensitivity of SLNB[59].However, the complex drainage patterns in the head and neck make staining of blue dye more difficult[60].While the rate of adverse reactions with blue dye is relatively low at 1%-3%, there remains a risk of anaphylactic reactions[61].Once a SN is identified with a handheld gamma probe and is excised, the gamma probe is used to check the count rate, measured as an instantaneous count andex vivo10 second target count.SLNB is considered complete when all nodes with > 10% radioactivity of the highest ex vivo count are removed[62-64].
A more recent development for SLNB is the utilization of indocyanine green (ICG), a near-infrared fluorophore that is injected peritumorally.The fluorescent ICG can be visualized up to 1cm transdermally with portable near-infrared imaging systems and can guide the site of incision and dissection for the biopsy[65,66].ICG reportedly has lower rates of severe allergic reactions compared to blue dye[65,67].Additionally, ICG can help detect SNs that may have been masked by radioactive shine-through due to their close proximity to the radiotracer injection site[68].
Indications for SLNB in early-stage OCSCC
In 2019, the NCCN guidelines included SLNB in the treatment algorithm for OCSCC[5].Table 4 is a summary of indications and contraindications of SLNB in OCSCC[5].
Utilization and indications of SLNB in OPSCC
Similar to OCSCC, OPSCC has a rate of occult nodal metastasis between 20%-30% for the ipsilateral neck and 16%-21% for the contralateral neck[7-9].
Over the last several decades, rates of human papillomavirus (HPV) associated with OPSCC have increased significantly.Numerous studies have demonstrated improved survival in patients with HPV-positive oropharyngeal cancer compared to those with HPV-negative oropharyngeal cancers[74-79].Anget al.evaluated a cohort of 206 HPV-positive and 117 HPV-negative stage III/IV OPSCC patients and demonstrated that patients with HPV-positive OPSCC had higher 3-year OS (82.4%vs.57.1%;P< 0.001)[74].HPV-positive patients also had a 58% reduction in risk of death after accounting for age, race, tumor and nodal stage, tobacco exposure, and treatment assignment (hazard ratio, 0.42; 95%CI: 0.27 to 0.66)[74].Depending on the stage at presentation and HPV status, the treatment for OPSCC can involve upfront surgical resection alone, upfront surgery followed by radiation ± chemotherapy, or definitive radiation with or without concomitant chemotherapy[5].
While some data exist regarding the utilization of SLNB for OPSCC, its use in this disease is still in its nascent stages.Several studies discussed earlier evaluating the role of SLNB in OCSCC also included patients with OPSCC, which has led to some early data on the feasibility and reproducibility of SLNB in OPSCC [Table 2][18,20,31,33].In a meta-analysis, Goverset al.reported a FNR (5%-30%) and NPV (88%-100%)for SLNB in all oral SCC (OCSCC and OPSCC)[20].However, none of these studies individually analyzed OPSCC patients when performing statistical analysis, thus limiting overall conclusions in the use of SLNB in this cohort.As such, while initial results are promising, this remains an area of active investigation.
Current radiotherapy management of OPSCC entails radiation of the primary tumor site and the bilateral necks, although unilateral radiation may be offered in well-lateralized tonsil cancers[80].One indication for SLNB currently under study involves evaluating the potential for contralateral neck drainage in welllateralized cN0 disease.One potential difference in utilizing SLNB in oropharyngeal versus oral cavity disease is patient tolerance of radiotracer injection.Thomaset al.performed awake injections of99mTc-sulfur colloid followed by SPECT-CT and reported successful radiotracer migration to the neck in 9 of 10 patients,one of which had bilateral drainage[81].Results from this study suggested that awake injection of radiotracer is feasible for oropharyngeal cancers; however, generalized conclusions cannot be made given the small sample size[81].The application of SLNB to guide elective radiotherapy management of OPSCC is the focus of a multicenter randomized controlled clinical trial, SPECT-CT Guided ELEctive Contralateral Neck Treatment for Patients with Lateralized Oropharyngeal Cancer (SELECT) (ClinicalTrials.gov Identifier:NCT05451004).This trial includes patients with cT1-3 lateralized OPSCC.Patients are randomized to undergo standard-of-care bilateral neck radiotherapy versus radiotherapy to the contralateral neck guided by lymphatic mapping.Patients with lymphatic drainage only to the ipsilateral neck would be spared radiation to the contralateral neck.The primary outcome of this study is 8-year DFS with secondary outcomes including 8-year OS, quality of life measures, and isolated contralateral neck failure.

Table 4.Indications and contraindications for SLNB in oral cavity squamous cell carcinoma
More recently, another trial (ClinicalTrials.gov Identifier: NCT05333523) has been designed to evaluate SLNB followed by neck irradiation for positive SNs versus bilateral elective neck irradiation in cN0 SCC of the oropharynx, larynx, and hypopharynx[82].The primary endpoints seek to determine 2-year regional lymph node recurrence and 6-month xerostomia-related quality of life[82].If the results show that the SLNB group is non-inferior to the elective neck irradiation group, then SLNB will become the standard of care[82].
Limitations of SLNB
While SLNB is feasible and has been adopted into NCCN guidelines for OCSCC, its utilization is still evolving and has several important limitations to consider, especially for use in OPSCC.For one, the reported FNR of 7%-14% has been a source of concern when considering SLNB over END, but this rate is similar to that reported for OCSCC after END (9%-20%)[35,36].Furthermore, studies have shown that there is a “learning curve” associated with SLNB, with NPV of 100% among experienced surgeons and 95% among less experienced surgeons[32].This factor may confound the reported FNR.Despite the reported FNR,studies have established SLNB to be a reliable method of evaluating the cN0 neck, with potential survival benefits[83].
Secondly, the complex lymphatic drainage system in the head and neck can present challenges in accurately identifying and detecting SNs for biopsy[23,30].This is especially true in the previously treated neck (prior surgery or radiation), as it can alter the lymphatic drainage and make it difficult to identify SNs.However,several studies have demonstrated the feasibility and reliability of identifying SNs in previously treated necks, reporting identification rates of SNs as high as 83%-100% with a NPV of 91%-100%[32,49,71,84-86].Additionally, Den Toomet al.observed unexpected lymphatic drainage patterns in 30% of patients with previously treated necks, highlighting the potential benefit of SLNB in identifying unexpected locations that can harbor metastases[84].
Another limitation is that SLNB requires more multi-disciplinary coordination than END.Coordination between the patient, nuclear medicine team, and the surgeon can be challenging to ensure proper timing of the lymphatic mapping with surgery.However, since the radiotracer can be injected the night before surgery with reliable results, there is more flexibility in the coordination[32,49].Additionally, SLNB has been part of the management algorithm for breast cancer and melanoma for many years, showing that providers can establish a workflow and coordinate the logistics needed to successfully incorporate SLNB into their practice.
Finally, a major limitation of SLNB in oral and oropharyngeal SCC is that long-term outcomes compared to standard-of-care treatment remain unknown, and this is an area of active investigation.
Future directions
Numerous novel applications/techniques to improve the utilization of SLNB are being developed.The use of a hybrid radiotracer, ICG-99mTc-nanocolloid, has been explored.With only one injection, the hybrid tracer can allow transdermal visualization using fluorescent light and radioactivity detection using a gamma probe[36,87].
The ability to perform frozen sections on SLNB specimens is appealing as a method to obtain immediate pathologic data to facilitate an immediate completion neck dissection in patients with positive SNs.This can avoid the challenges of coordinating a second surgery or subjecting patients to a second anesthetic.The way that SNs are reviewed by pathologists is also advantageous and can be an avenue for future research.Histologic evaluation of SNs typically utilizes thinner slices via serial sectioning and immunohistochemistry stains to identify micrometastasis and isolated tumor cells.This process is not routinely utilized, nor feasible, in the pathologic evaluation of complete lymph node packets from an END due to time and cost constraints[88,89].Vorburgeret al.established that frozen sections using the monoslice technique detect positive SNs in about half of the patients and the sensitivity of this method depends on the size of metastasis[88].While the multislice technique for frozen sections is more accurate, the monoslice technique is a single stage procedure that requires less time and is able to identify macrometastases with high accuracy[88].These detailed pathologic evaluations are important since studies have demonstrated a difference in OS between patients with isolated tumor cells, micrometastases, and macrometastases[33,37,90].
Real-time quantitative PCR on SNs is an area of exploration and shows potential for more accurate intraoperative identification of occult metastases[91,92].The application of machine learning is also being explored to help identify pathological features that predict the risk of metastasis prior to surgical treatment[93,94].The hope is to identify patients who are at higher risk and may benefit from SLNB or END versus observation.
CONCLUSION
SLNB has emerged as a promising technique to identify occult nodal metastasis in patients with oral cancer and can accurately map lymphatic drainage in OPSCC.Compared to END, SLNB portends reduced morbidity, potentially avoids overtreatment, and offers important staging and prognostic information.In addition to evaluating ipsilateral disease, SLNB has the ability to detect contralateral occult nodal disease even in well-lateralized tumors, which is useful in guiding radiotherapy of the contralateral neck in OPSCC.Ongoing clinical trials continue to investigate the outcomes of implementing SLNB in the management of oral and oropharyngeal SCC.
DECLARATIONS
Author Contributions
Made substantial contributions to the conception and design of the study: Chan K, Saltagi1 M, Choi KY
Availability of Data and Materials
Not applicable.
Financial Support and Sponsorship
None.
Conflicts of Interest
Dr.Karen Y.Choi is a consultant with Cardinal Health.Otherwise, all authors declared that there are no conflicts of interest.
Ethical Approval and Consent to Participate
Not applicable.
Consent for Publication
Not applicable.
Copyright
© The Author(s) 2024.
杂志排行
Plastic and Aesthetic Research的其它文章
- Early lymphaticovenous anastomosis in lymphedema management: a pilot study
- Therapeutic management of the painful nerve: a narrative review of common rehabilitation interventions
- Role of transoral robotic surgery in the salvage setting: pitfalls and challenges
- Systematic review on the centrocentral anastomosis technique for the surgical treatment of traumatic neuromas
- The mangled upper extremity: a principled approach to management