Are treatment options used for adult-onset type 2 diabetes mellitus (equally) available and effective for children and adolescents?
2024-04-22NevenaKrnicViborSesaAnnaMrzljakMajaCigrovskiBerkovic
Nevena Krnic,Vibor Sesa,Anna Mrzljak,Maja Cigrovski Berkovic
Abstract Youth-onset type 2 diabetes mellitus (T2DM),influenced by an increase in obesity,is a rising problem worldwide.Pathophysiological mechanisms of this early-onset T2DM include both peripheral and hepatic insulin resistance,along with increased hepatic fasting glucose production accompanied by inadequate first and second-phase insulin secretion.Moreover,the incretin effect is reduced.The initial presentation of type 2 diabetes can be dramatic and symptoms may overlap with those of type 1 diabetes mellitus.Therefore,immediate therapy should address hyperglycemia and associated metabolic derangements irrespective of ultimate diabetes type,while further therapy adjustments are prone to patients’ phenotype.New agents with proven glycemic and beyond glycemia benefits,such as Glucagon-like polypeptide 1 receptor agonists and Sodium-glucose cotransporter-2 inhibitors,used in the adult population of T2DM patients,might become increasingly important in the treatment armamentarium.Moreover,metabolic surgery is an option for markedly obese (body mass index > 35 kg/m2) children and adolescents suffering from T2DM who have uncontrolled glycemia and/or serious comorbidities when lifestyle and pharmacologic interventions fail.In this mini-review,we will discuss the potential of treatment options considering new data available from randomized control trials,including individuals with adultonset type diabetes mellitus.
Key Words: Youth-onset type 2 diabetes mellitus;Treatment;Complications;Glucose lowering agents;Extra-glycemic benefit
INTRODUCTION
Youth-onset type 2 diabetes mellitus (T2DM) is increasing in incidence and prevalence.There is a strong predilection for its development in certain ethnic groups[1] and evermore so,the development of T2DM is related to the cumulative effect of early onset persistent obesity[2].Despite male predominance among adolescents with prediabetes[3],there is a higher prevalence of T2DM in females[4].Due to specific and unfavorable metabolic profiles encompassing insulin resistance and early β-cell decline,youth-onset T2DM is often accompanied by chronic end-stage complications,which become apparent much earlier in life[4,5].Especially important are cardiovascular complications,which are not only a consequence of early-onset hyperglycemia but also of accompanying comorbidities,making treatment decisions difficult[6].Currently,only a few therapeutic agents gained approval from the regulatory agencies for the treatment of youthonset T2DM.Decision on their use and combinations often depends on the presenting clinical features,hemoglobin A1c (HbA1c) and hyperglycemia level,and the presence of catabolism (diabetic ketoacidosis or hyperosmolar hyperglycemic state).Moreover,it also depends on the long-term efficacy and,in the newer time,due to the availability of agents with cardiovascular and renal benefits,on the patient’s risk stratification and presence of comorbidities.Although there is a female gender predilection for T2DM development and a tendency for resolution of dysglycemia in male patients following puberty[7],there are no recommendations for different treatment approaches in male and female patients.Most treatment practice for youth-onset T2DM is derived from adult patients.However,they do not necessarily have the same pathophysiological features and therapeutic effects might not be the same as in adults.The aim of treatment in youth with T2DM is agreed at HbA1c < 7.0%[8],but several studies demonstrated a more aggressive course of disease in younger patients,suggesting stricter metabolic control might be necessary[9].All available treatment modalities have comparable glucose-lowering effects[8] of HbA1c reduction by 1%-2%,but no data regarding favorable effects on other metabolic complications of T2DM and obesity.Furthermore,pharmacological and nonpharmacological therapy failure is more common in adolescents (first-line treatment with metformin and intensive lifestyle changes are suboptimal in more than 50% of youth within 2 years of diagnosis),necessitating the need for treatment intensification[10,11].
Metformin
Metformin remains the pharmacological cornerstone of T2DM treatment in children and adolescents with T2DM,according to international guidelines[8,12].It is advised as a first-line treatment in case of newly diagnosed T2DM in children and youth who present without ketoacidosis or hyperosmolar hyperglycemic state and if HbA1c < 8.5%.In contrast,it can be combined with basal insulin as a starting therapy when HbA1c exceeds 8.5%,with no signs of hypoinsulinemia[13].
Improvement in HbA1c ranges from 1 to 2%,but metabolic effects also include improved insulin sensitivity and potential beneficial effects on cardiovascular function,while the effects on reduction of body weight and waist circumference are limited[14].In adults,metformin increases insulin sensitivity and delays β-cell decline.Compared to adults,metformin therapy does not favor residual β-cell function in children and adolescents[15],presumably due to more apparent hepatic insulin resistance earlier in the disease course[16].Therefore,there is no current data to support the use of metformin in adolescents with prediabetes for the prevention of T2DM development[17].Moreover,expectations of its long-term effects on glucose lowering in youth-onset T2DM alone or in combination with lifestyle interventions or insulin are modest,while its modulation of the entero-insular axisviagut microbiome is of a neglectable size.In addition,up to date,there is no evidence of its effect on reducing visceral or hepatic fat or lipolysis in children and adolescents with T2DM[11] (Figure 1).
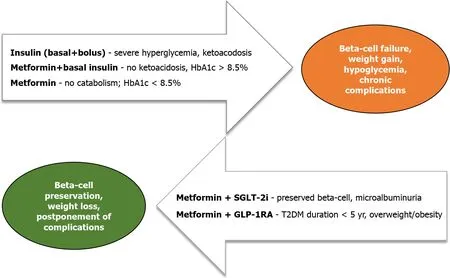
Figure 1 Paradigm shift in youth-onset type 2 diabetes mellitus treatment. T2DM: Type 2 diabetes mellitus;HbA1c: Hemoglobin A1c;SGLT-2i: Sodium-glucose cotransporter-2 inhibitors;GLP-1RA: Glucagon-like polypeptide 1 receptor agonists.
Thiazolidinediones
Rosiglitazone was evaluated in youth with T2DM as an add-on therapy to metformin[18],with superior improvement in insulin sensitivity and fewer adverse effects[19] as compared to metformin alone,but so far,it has not gained approval for T2DM treatment in children and adolescents.In addition,rosiglitazone has been strongly restricted or even withdrawn from the market in most countries due to concerns about its cardiovascular safety;therefore,its use in adult T2DM is limited[20].On the other hand,pioglitazone,yet another thiazolidinedione,has an important role in the treatment of adult T2DM patients with metabolic syndrome and cardiovascular risk,but its use in youth-onset T2DM is scarce and not approved[21].
Insulin
Several therapy modalities using different types of insulin are used in the treatment of youth-onset T2DM.Insulin can be used as initial therapy in severe presentation of T2DM (ketosis/ketoacidosis or HbA1c > 8.5%)[8] or additional therapy if other therapeutic options fail to achieve improvement in metabolic control.However,insulin can lead to weight gain,which can perpetuate obesity and subsequent metabolic complications.The addition of insulin to youth with T2DM already treated with different treatment modalities (metformin alone/metformin+rosiglitazone/metformin+lifestyle interventions) led to variable therapeutic effects (only 33.2% of participants had consistent HbA1c decrease of ≥ 0.5%)[22],in addition to the need of treatment intensification with more complex regimens (basal bolus)[13].Insulin is advised primarily in the form of multiple daily injections.At the same time,there are no studies done on youth-onset T2DM with insulin deliveredviapump therapy with hybrid closed-loop technology,although data from adult T2DM are promising[23].
Glucagon-like polypeptide 1 receptor agonists
Glucagon-like polypeptide 1 receptor agonists (GLP-1RA),liraglutide,exenatide and dulaglutide,once daily or once weekly,have recently been approved for the treatment of T2DM in children and adolescents.The therapeutic benefit includes glucose-lowering effect (HbA1c lowering by 0.85% to 1.4% after 24 to 26 wk of therapy),while effects on body mass index and waist circumference are less pronounced than that seen in the adult population with T2DM and potentially require more prolonged duration of treatment (more than 52 wk)[24-26].Moreover,a rebound is seen after discontinuation of treatment[27-29].Nonetheless,one might speculate that early introduction of GLP-1RAs,in combination with metformin,might be beneficial for youth-onset T2DM,especially in case of early-stage disease,lasting for less than 5 years,while it would improve β-cell function,in addition to targeting insulin resistance and obesity.
Sodium-glucose cotransporter-2 inhibitors
Sodium-glucose cotransporter-2 inhibitors (SGLT-2i),empagliflozin,has been approved for treating children and adolescents with T2DM since June 2023,alone or in combination with metformin[29].The reduction in HbA1c of 1.13% was demonstrated in clinical trials,and similar to GLP-1RAs,the weight-lowering effect is minimal compared to the one seen in adults with T2DM[30].Although no data is available in youth with T2DM,it could be assumed that beneficial effect on cardiovascular function and renal disease,as seen in adults,would also be demonstrated in youth with T2DM[31,32].SGLT-2i promote urinary glucose excretion with compensatory increases in rates of gluconeogenesis and ketosis.How this transcribes in glucose management of young-onset T2DM is to be seen,while there is a defect in gluconeogenesis regulation.Moreover,the problem of euglycemic ketosis must not be neglected.
Use of technological devices
As compared to the frequent use of different technological devices among children and adolescents with type 1 diabetes,there are no current recommendations for similar use among youth with T2DM.Some studies have proven that continuous or intermittent glucose monitoring devices (CGM) are beneficial for lifestyle modification interventions[33].Furthermore,it was demonstrated that greater fasting glucose variability during the first year following the diagnosis of T2DM is highly predictive of deterioration of β-cell function and development of comorbidities in following years[34].CGM might help to detect those patients and intensify their treatment in the early phase of T2DM.The indications for using devices for CGM with different types of treatment or cost-effectiveness have not yet been established,and health insurance policies do not cover expenses in most countries.
Metabolic surgery
Metabolic surgery is becoming an important tool in treating obesity in youth with type 2 diabetes,although numbers of treated patients are rather small and data on long-term safety and durability of treatment success still lacking[35].The most commonly used methods Roux-en-Y gastric bypass,and vertical sleeve gastrectomy are highly effective,and weight reduction up to 73% is reported,together with T2DM remission after 3-years of follow-up,which is similar to that observed in adult T2DM population[36].Timing of metabolic surgery is an important issue,and is still debatable,but many authorities argue that intervention earlier during adolescence,would be more beneficial in terms of offering comprehensive metabolic remission and fewer and/or postponed vascular complications in the future[37].Finally,meticulous surveillance and strong family support is necessary to prevent nutritional deficiencies and potential regain of weight after bariatric surgery[38,39].
CONCLUSlON
Although pharmacotherapy of adult-onset T2DM is diverse and efficient both in glucose management and offering cardiovascular and renovascular benefits,currently,there are only four medication classes for youth-onset T2DM: Historical agents such as metformin,insulin,and newer GLP-1RAs (liraglutide,exenatide and dulaglutide) and SGLT-2i empagliflozin.The poor long-term durability of metformin and insulin with the risk of hypoglycemia,weight gain and no potential for β-cell preservation might lead to a paradigm shift and more robust use of agents beyond glycemic effects.Whether their efficiency and long-term safety will be comparable to that seen in adult T2DM and the preferable timing and best combinations for youth-onset T2DM remain to be seen.
FOOTNOTES
Author contributions:Krnic N was involved in conceptualization of the study;Cigrovski Berkovic M was responsible for data curation;Krnic N and Mrzljak A drafted the original version of the manuscript;Mrzljak A and Sesa V reviewed and edited the manuscript.All authors have read and agreed to the published version of the manuscript.
Conflict-of-interest statement:All authors have no conflict of interest regarding this article.
Open-Access:This article is an open-access article that was selected by an in-house editor and fully peer-reviewed by external reviewers.It is distributed in accordance with the Creative Commons Attribution NonCommercial (CC BY-NC 4.0) license,which permits others to distribute,remix,adapt,build upon this work non-commercially,and license their derivative works on different terms,provided the original work is properly cited and the use is non-commercial.See: https://creativecommons.org/Licenses/by-nc/4.0/
Country/Territory of origin:Croatia
ORClD number:Vibor Sesa 0000-0002-4725-5727;Anna Mrzljak 0000-0001-6270-2305;Maja Cigrovski Berkovic 0000-0003-0750-9785.
S-Editor:Qu XL
L-Editor:A
P-Editor:Yuan YY
杂志排行
World Journal of Diabetes的其它文章
- Nε-carboxymethyl-lysine and inflammatory cytokines,markers and mediators of coronary artery disease progression in diabetes
- Non-pharmacological interventions for diabetic peripheral neuropathy: Are we winning the battle?
- Application and management of continuous glucose monitoring in diabetic kidney disease
- Role of renin-angiotensin system/angiotensin converting enzyme-2 mechanism and enhanced COVlD-19 susceptibility in type 2 diabetes mellitus
- Prevalence and risk factors of wound complications after transtibial amputation in patients with diabetic foot
- Prevalence and risk factors of diabetes mellitus among elderly patients in the Lugu community
