Effect of viral hepatitis on type 2 diabetes: A Mendelian randomization study
2024-03-08YunFengYuGangHuKeKeTongXinYuYangJingYiWuRongYu
Yun-Feng Yu,Gang Hu,Ke-Ke Tong,Xin-Yu Yang,Jing-Yi Wu,Rong Yu
Abstract BACKGROUND The effects of viral hepatitis (VH) on type 2 diabetes (T2D) remain controversial.AIM To analyze the causal correlation between different types of VH and T2D using Mendelian randomization (MR).METHODS Single nucleotide polymorphisms of VH,chronic hepatitis B (CHB),chronic hepatitis C (CHC) and T2D were obtained from the BioBank Japan Project,European Bioinformatics Institute,and FinnGen.Inverse variance weighted,MREgger,and weighted median were used to test exposure-outcome associations.The MR-Egger intercept analysis and Cochran’s Q test were used to assess horizontal pleiotropy and heterogeneity,respectively.Leave-one-out sensitivity analysis was used to evaluate the robustness of the MR analysis results.RESULTS The MR analysis showed no significant causal relationship between VH and T2D in Europeans [odds ratio (OR)=1.028;95% confidence interval (CI): 0.995-1.062,P=0.101].There was a negative causal association between CHB and T2D among East Asians (OR=0.949;95%CI: 0.931-0.968,P < 0.001),while there was no significant causal association between CHC and T2D among East Asians (OR=1.018;95%CI: 0.959-1.081,P=0.551).Intercept analysis and Cochran’s Q test showed no horizontal pleiotropy or heterogeneity (P > 0.05).Sensitivity analysis showed that the results were robust.CONCLUSION Among East Asians,CHB is associated with a reduced T2D risk,but this association is limited by HBV load and cirrhosis.Although VH among Europeans and CHC among East Asians are not associated with the risk of T2D,focusing on blood glucose in patients with CHC is still relevant for the early detection of T2D induced by CHCmediated pathways of hepatic steatosis,liver fibrosis,and cirrhosis.
Key Words: Viral hepatitis;Chronic hepatitis Β;Chronic hepatitis C;Type 2 diabetes;Mendelian randomization
lNTRODUCTlON
Type 2 diabetes (T2D) is a chronic metabolic disease characterized by relative insulin deficiency and abnormally elevated blood glucose[1].An epidemiological study has shown that as the prevalence of diabetes increases each year,approximately 1 in 10 adults globally now have diabetes,and it is projected that by 2045,the world will have 693 million individuals with diabetes[2,3].As an incurable disease,the hyperglycemic state in T2D increases the risk of macrovascular pathologies,such as cardiovascular disease,and microvascular pathologies,such as nephropathy,retinopathy,and peripheral neuropathy[4,5].T2D is a serious threat to the life and health of patients,especially the thrombotic events caused by cardiovascular and cerebrovascular lesions,which are the leading causes of death in patients with T2D[2,6].Obesity,high-fat diet,and physical inactivity are risk factors for T2D,and controlling these risk factors helps reduce the risk of developing T2D and improve its prognosis[7,8].Therefore,controlling the related risk factors,particularly highrisk factors,is essential for the prevention and treatment of T2D.In recent years,an increasing number of studies have reported an association between hepatitis viruses and diabetes mellitus[9],and evidence suggests that chronic viral hepatitis (VH) may be a potential risk factor for T2D[10,11].
VH,an inflammatory disease of the liver caused by infection with the hepatitis A virus (HAV),hepatitis B virus (HBV),hepatitis C virus (HCV),hepatitis D virus (HDV),or hepatitis E virus (HEV),is a major global health problem[12].These viruses cause acute hepatitis,and HBV,HCV,and HDV infections progress to chronic hepatitis[13,14].Globally,approximately 257 million individuals have been reported to be infected with HBV,and 71 million are infected with HCV[15].Chronic hepatitis B (CHB) from HBV infection and chronic hepatitis C (CHC) from HCV infection cause persistent damage to the liver,resulting in liver fibrosis,cirrhosis,liver cancer,and even death[13,16].Relevant studies have shown that hepatitis B cirrhosis and HCV infection increased the risk of T2D by 74% and 1058%,respectively[11,17],suggesting that CHB and CHC are potential risk factors for T2D.This effect may be related to the signaling pathway by which hepatitis viruses alter hepatic glucose homeostasis by mediating the overexpression of protein phosphatase 2A to inhibit Akt and FoxO1 dephosphorylation[18].However,some studies have reported that HBV and HCV infections do not increase the incidence of T2D[19,20],which indirectly negates the relationships of them.Whether different categories of VH,especially CHB and CHC,are associated with the risk of T2D remains controversial,and the causal relationship between them needs to be further explored.
Mendelian randomization (MR) is a method for assessing the causal relationship between exposure and outcome variables using genetic variants[21].Due to the randomized nature of allele classification,MR has properties similar to those of randomized controlled trials[22].Although MR cannot be used as a substitute for randomized controlled trials,it provides additional evidence for causality analysis[23].This MR analysis explored the causal relationship between T2D and VH,CHB,and CHC from a gene prediction perspective,with the aim of providing additional evidence for risk factor studies in diabetes.
MATERlALS AND METHODS
Study design
MR relies on three primary assumptions[24]: (1) Association assumption: Single nucleotide polymorphisms (SNPs) are strongly associated with exposure factors;(2) Independence assumption: SNPs are independent of confounding variables;and (3) Exclusivity assumption: SNPs do not act on outcome variables through pathways other than through exposure factors.The design is illustrated in Figure 1.
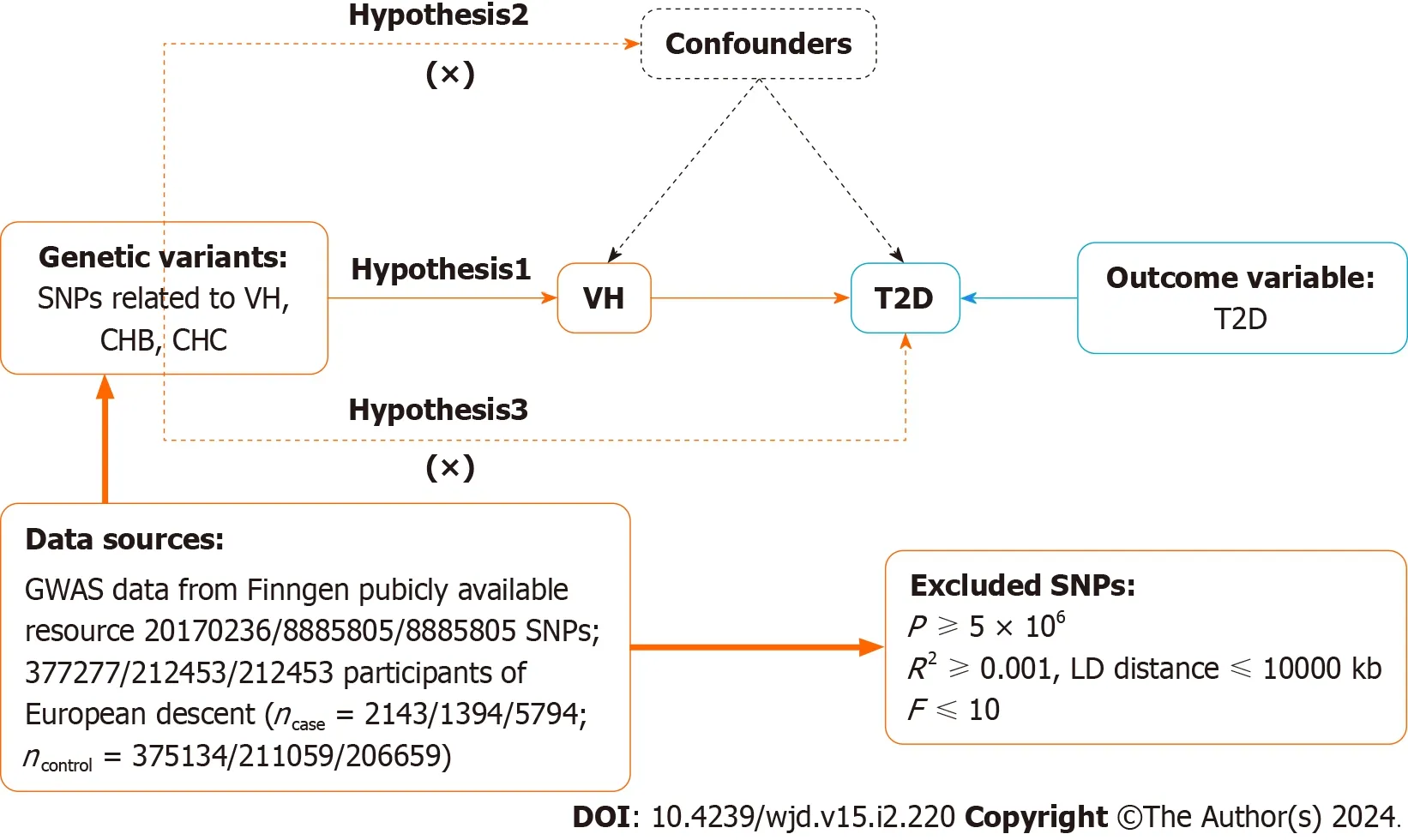
Figure 1 Mendelian randomization design for causal analysis of viral hepatitis,chronic hepatitis Β,chronic hepatitis C and type 2 diabetes. VH: Viral hepatitis;CHB: Chronic hepatitis B;CHC: Chronic hepatitis C;T2D: Type 2 diabetes;GWAS: Genome-wide association studies;SNP: Single nucleotide polymorphisms;LD: Linkage disequilibrium.
Data sources
Data on VH,CHB,CHC,and T2D were obtained from the BioBank Japan Project (https://biobankjp.org/en/),European Bioinformatics Institute (https://www.ebi.ac.uk),and FinnGen (www.finngen.fi/fi).All the data were sourced from publicly available databases;therefore,no additional ethical approval was required.
Selection of genetic instrument variables
First,SNPs strongly associated with exposure factors were screened in the genome-wide association studies (GWAS),according to a threshold ofP< 5 × 10-6to fulfill assumption 1.Second,independent SNPs were screened,according toR2< 0.001 and kb=10000,to avoid potential bias due to linkage disequilibrium.Third,theF-value of each SNP was calculated,and SNPs withF≤ 10 were excluded.F-value was calculated publicly asF=[R2/(1 -R2)] × [(N -K -1)/K],whereR2=2 × (1 -MAF) × MAF × β2.R2: The cumulative explained variance of the selected instrument variables on exposure;MAF: The effect of minor allele frequency;β: The estimated effect of SNP;and N: Sample size of the GWAS.Finally,we referred to PhenoScanner (www.phenoscanner.medschl.cam.ac.uk) and related literature to remove SNPs potentially associated with T2D to fulfill assumption 2.
Data analysis
This study followed the STROBE-MR guidelines[25].The “TwoSampleMR (0.5.7)” program package for R 4.3.1 was used to perform the two-sample MR analysis.Inverse variance weighting (IVW),MR-Egger,and weighted median were used as basic causality assessment methods.Among these methods,IVW was the primary analysis method[26] that achieved unbiased causal estimation without horizontal pleiotropy.MR-Egger and the weighted median are complementary methods to MR analysis,with the former providing valid causal estimation in some cases where pleiotropy exists,and the latter being less sensitive to outliers and measurement errors.
The MR results were corrected and analyzed using the MR-Pleiotropy Residual Sum and Outlier method (MRPRESSO),and the MR analysis was re-executed after removing outlier SNPs (P< 1).Horizontal pleiotropy was assessed using MR-Egger’s intercept analysis,andP≥ 0.05 suggested the absence of horizontal pleiotropy to fulfill assumption 3.Heterogeneity was assessed using Cochran’sQtest,andP≥ 0.05 suggested the absence of heterogeneity.Leave-one-out sensitivity analysis was used to assess the robustness of the results and clarify individual SNP that significantly affected the pooled results.
RESULTS
GWAS data for exposure factors
The VH data were obtained from FinnGen,which included 377277 European participants (dataset number: finngen_R9_AB1_VIRAL_HEPATITIS).Data on CHB were obtained from the BioBank Japan Project,which contains information on 212453 East Asians (dataset number: bbj-a-99).Data on CHC were obtained from the BioBank Japan Project,which contains information on 212453 East Asians (dataset number: bbj-a-101).Eighty-six SNPs closely related to VH were provided by FinnGen,8719 closely associated with CHB,and 1494 closely related to CHC were supplied by the BioBank Japan Project.Eleven SNPs for VH,14 for CHB,and 13 for CHC were included after excluding the effects of linkage disequilibrium and confounding variables (Supplementary Table 1).Duplicated and mismatched SNPs were excluded based on the EAF values when harmonizing the allelic orientations of the exposure and outcome SNPs.Outlier SNPs were excluded from MR-PRESSO correction analysis.Finally,11 SNPs for VH,nine for CHB,and six for CHC were included (Supplementary Table 2).

Table 1 Details of the Genome-wide association studies included in the Mendelian randomization
GWAS data for outcome variables
The T2D data for Europe were obtained from FinnGen,including 365950 European participants (dataset number: finngen_R9_T2D).Data on T2D for East Asia were obtained from the European Bioinformatics Institute,and it included 433540 East Asian individuals (dataset number: ebi-a-GCST010118) (Table 1).
MR analysis results of two samples
The causal effects between the exposure factors (VH,CHB,and CHC) and outcome variable (T2D) were analyzed using two-sample MR.A forest plot of the MR analysis is shown in Figure 2,and a scatter plot of the effect estimates for each SNP is shown in Figure 3.The results of the intercept analysis are shown in Supplementary Table 3.The results of the heterogeneity test are shown in Figure 4 and Supplementary Table 4.The sensitivity analysis is shown in Figure 5.
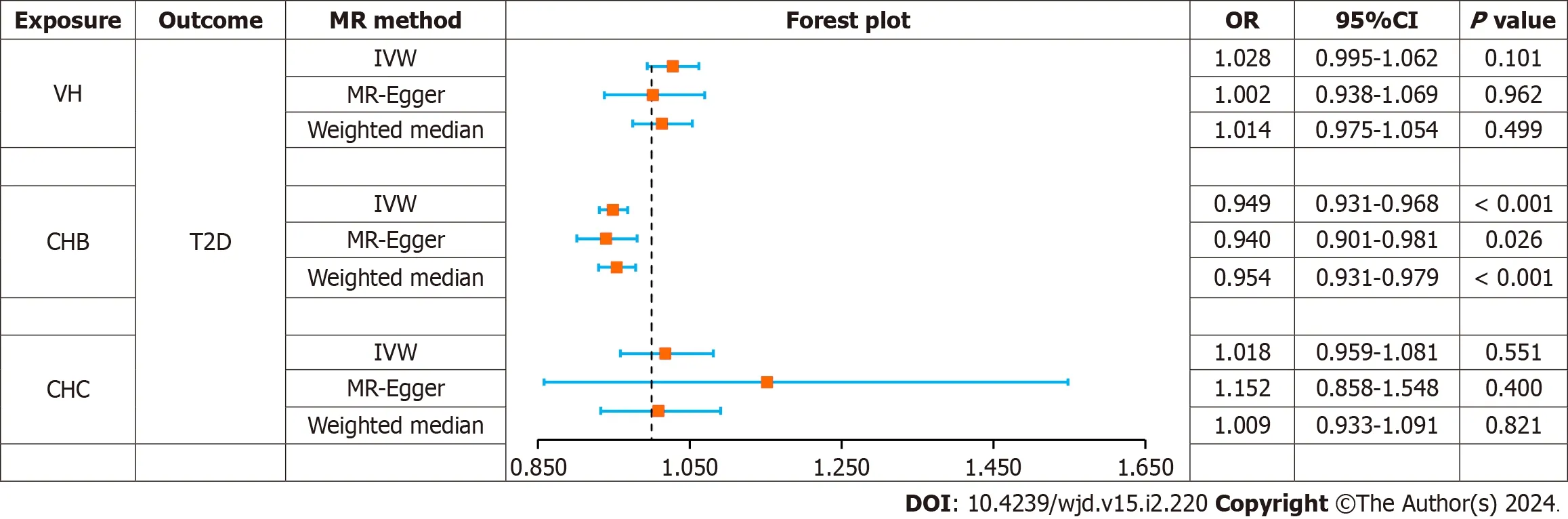
Figure 2 Forest plot of Mendelian randomization analysis on the causal relationship between viral hepatitis,chronic hepatitis Β,chronic hepatitis C and type 2 diabetes. VH: Viral hepatitis;CHB: Chronic hepatitis B;CHC: Chronic hepatitis C;T2D: Type 2 diabetes;OR: Odd ratio;SNP: Single nucleotide polymorphisms;MR: Mendelian randomization;CI: Confidence interval;IVW: Inverse variance weighting.
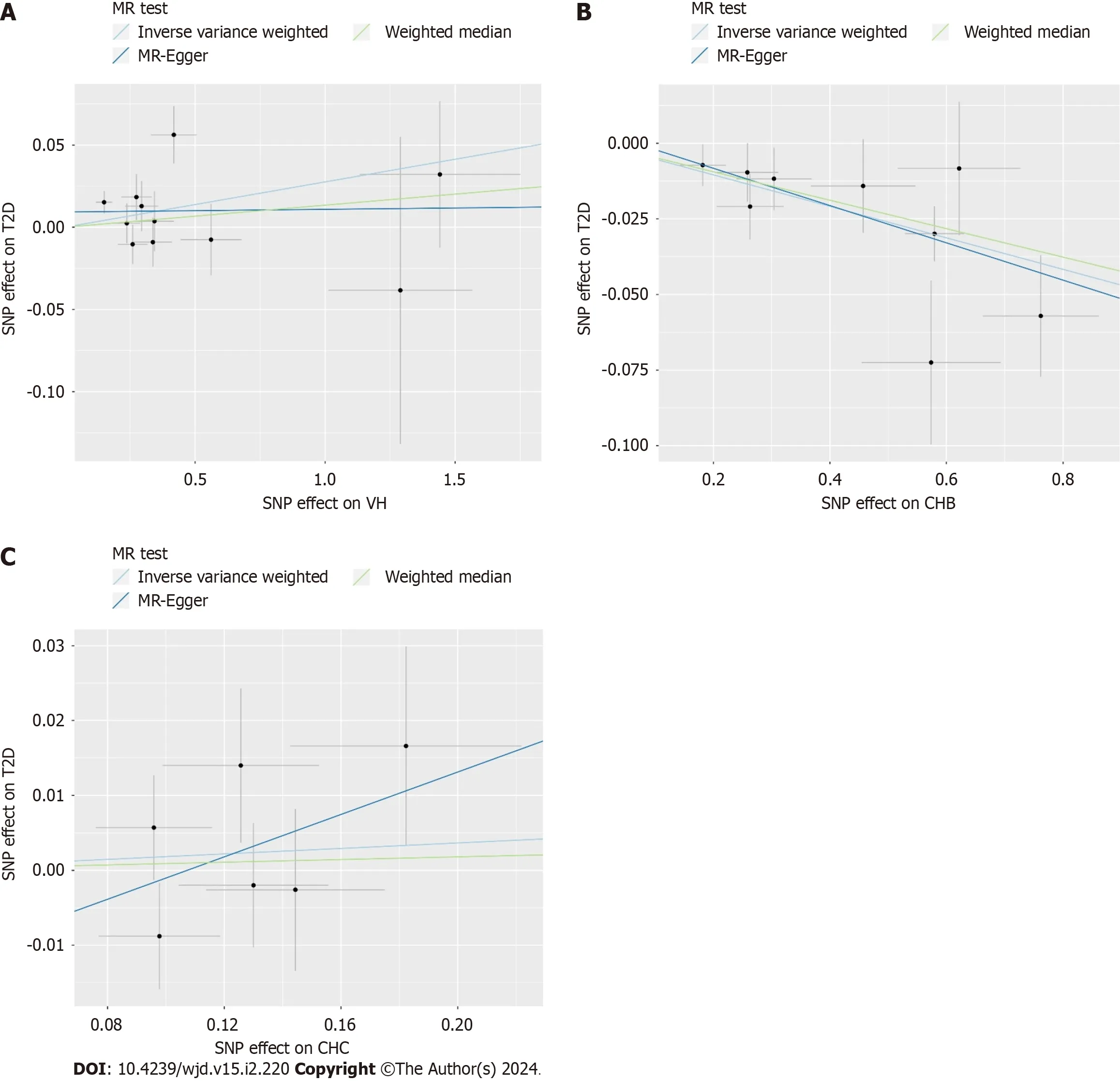
Figure 3 Scatter plot of Mendelian randomization analysis on the causal relationship between viral hepatitis,chronic hepatitis Β,chronic hepatitis C and type 2 diabetes. A: Viral hepatitis on type 2 diabetes;B: Chronic hepatitis B on type 2 diabetes;C: Chronic hepatitis C on type 2 diabetes.VH: Viral hepatitis;CHB: Chronic hepatitis B;CHC: Chronic hepatitis C;T2D: Type 2 diabetes;MR: Mendelian randomization.

Figure 4 Funnel plot of heterogeneity analysis on viral hepatitis,chronic hepatitis Β,chronic hepatitis C and type 2 diabetes. A: Viral hepatitis on type 2 diabetes;B: Chronic hepatitis B on type 2 diabetes;C: Chronic hepatitis C on type 2 diabetes.MR: Mendelian randomization.
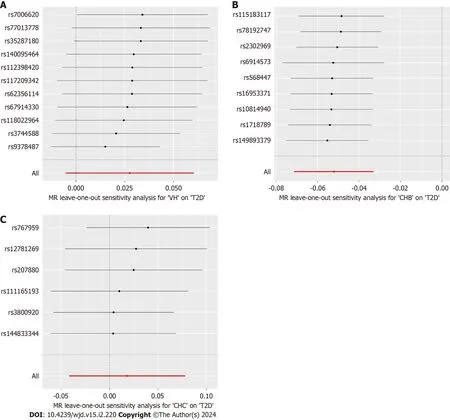
Figure 5 The results of leave-one-out sensitivity analysis on viral hepatitis,chronic hepatitis Β,chronic hepatitis C and type 2 diabetes. A: Viral hepatitis on type 2 diabetes;B: Chronic hepatitis B on type 2 diabetes;C: Chronic hepatitis C on type 2 diabetes.VH: Viral hepatitis;CHB: Chronic hepatitis B;CHC: Chronic hepatitis C;T2D: Type 2 diabetes.
VH:None of the three methods of analysis showed significant causal relationships between VH and T2D in Europeans: IVW [odds ratio (OR)=1.028;95% confidence interval (CI): 0.995-1.062;P=0.101],MR-Egger (OR=1.002;95%CI: 0.938-1.069;P=0.962),or weighted median (OR=1.014;95%CI: 0.975-1.054;P=0.499).Intercept analysis showed no horizontal pleiotropy (P=0.391).Cochran’sQtest showed no heterogeneity (P=0.119).Sensitivity analysis suggested that the results were robust.
CHB:All the three methods of analysis showed a negative causal association between CHB and T2D among East Asian individuals: IVW (OR=0.949;95%CI: 0.931-0.968;P< 0.001),MR-Egger (OR=0.940;95%CI: 0.901-0.981;P=0.026),and weighted median (OR=0.954;95%CI: 0.931-0.979;P< 0.001).Intercept analysis showed no horizontal pleiotropy (P=0.640).The Cochran’sQtest revealed no heterogeneity (P=0.685).Sensitivity analysis suggested that the results were robust.
CHC:None of the three analysis methods showed a significant causal relationship between CHC and T2D in East Asians: IVW (OR=1.018;95%CI: 0.959-1.081,P=0.551),MR-Egger (OR=1.152;95%CI: 0.858-1.548,P=0.400),and weighted median (OR=1.009;95%CI: 0.933-1.091,P=0.821).Intercept analysis showed no horizontal pleiotropy (P=0.640).The Cochran’sQtest showed no heterogeneity (P=0.376),and the sensitivity analysis suggested that the results were robust.
DlSCUSSlON
VH is an inflammatory liver disease caused by viruses,such as HAV,HBV,HCV,HDV,and HEV,and is one of the most common liver diseases[27].Some evidence suggests that HBV and HCV infection are associated with impaired glucose tolerance and increased incidence of diabetes mellitus[28,29],which are potential risk factors for T2D.However,other studies have found that neither HBV nor HCV infections are associated with T2D risk[20,30].The effects of HBV and HCV infections on T2D remain controversial,and their causal relationship remains unclear.To further understand the potential impact of different types of VH on T2D,MR was used to analyze the causal relationships of VH,CHB,and CHC with T2D.
This study found no significant causal association between VH and T2D risk in the European population.Among East Asians,CHB was associated with a lower risk of T2D,whereas CHC was not associated with a risk of T2D.The Cochrane’sQ-test and intercept analysis showed no heterogeneity or horizontal pleiotropy in these results,and the sensitivity analysis showed that the MR results were robust.As the GWAS did not include data on HAV,HDV,and HEV infections,this study did not assess the effect of these three types of VH on the risk of T2D.Additionally,the impact of CHB and CHC on T2D among Europeans is still being determined because GWAS do not contain available data on CHB and CHC in Europeans.
Our results showed that CHC was not associated with T2D risk,which is consistent with previous reports.A United States clinical trial,involving 15125 individuals found that neither the prevalence of prediabetes nor diabetes was associated with HCV infection,and the level of insulin resistance was not associated with HCV markers[20].Additionally,an Iranian case-control study noted that CHC was not a risk factor for insulin resistance or diabetes in the Iranian population[31].
However,studies supporting the notion that CHC is not associated with T2D are few,and to date,most clinical studies have pointed to a correlation between CHC and T2D.Mehtaetal[17] suggested that CHC is a potential risk factor for T2D,and they found a higher risk of T2D in patients with CHC than that in healthy individuals.An Italian single-arm trial noted that a significant effect of HCV on glucose load developed through increased insulin resistance in the liver and muscles[32].The impact of HCV on blood glucose levels and risk of diabetes was more pronounced in patients aged 35-49 years and in those with severe liver disease[33].The risk for T2D in patients with CHC has been reported to increase with increasing levels of liver fibrosis[34,35].Additionally,there is evidence that patients with CHC infected with HCV1b and HCV3 have a higher incidence of T2D[36,37],implying that the HCV genotype is an essential factor influencing the risk of T2D.These results suggest that HCV increases the risk of developing T2D by affecting insulin sensitivity,and that this association is related to the degree of liver fibrosis and HCV genotype.Therefore,HCV eradication may help reduce blood glucose levels and T2D risk.Giladetal[38] and Husseinetal[39] found that diabetic patients coinfected with HCV who were treated with direct-acting antiviral agents (DAAs) had significant improvements in glycosylated hemoglobin levels and insulin resistance,as well as a substantial reduction in diabetes-related microvascular complications[40].Two meta-analyses have shown that DAAs restore HCV-induced alterations in glucose homeostasis by inducing a sustained virological response,thereby reducing insulin resistance and T2D risk[41,42].These findings indicate that anti-HCV therapy benefits patients with T2D,and provide indirect evidence that CHC is a risk factor for T2D.
Although considerable evidence points to CHC as a potential risk factor for T2D,this MR analysis,based on genetic prediction,did not reveal a causal relationship between them.The MR analysis and clinical trial results differed,possibly because of intermediate factors between CHC and T2D.Ruhletal[20] stated that diabetes risk is associated with elevated alanine aminotransferase and gamma-glutamyltransferase activities rather than HCV infection status.The authors suggested that the association between HCV infection and T2D reported in previous studies was related to elevated liver enzyme[20].Related studies have shown that insulin resistance in individuals infected with HCV is associated with alterations in alanine transaminase,aspartate aminotransferase,and bilirubin levels[43].Papatheodoridisetal[44] found that the risk of T2D in HCV-infected individuals was associated with hepatic fibrosis,cirrhosis,hepatic steatosis,and increased serum triglyceride levels.
Additionally,researchers have observed that HCV infection increases the risk of obesity and metabolic syndrome (MS) by affecting the liver.In a clinical study in Virginia,Younossietal[45] found that HCV genotype three was associated with an increased risk of steatosis and fatty liver disease.A Taiwanese study has shown that HCV regulates host lipid metabolism and distribution to some extent[46].Another Taiwanese study showed that the prevalence of MS was higher in individuals infected with HCV than that in non-infected patients (24.7%vs13.2%)[47].The effects of HCV infection on obesity and MS may be mediated through the promotion of hepatic steatosis and fibrosis.Hepatitis C core viral proteins in patients with HCV,especially in genotype 3a-infected patients,induced sterol regulatory element-binding protein 1 and peroxisome proliferator-activated receptor γ gene expression and activity,thereby increasing the transcription of genes involved in hepatic fatty acid synthesis,and ultimately promoting steatosis[48].Hepatitis C core viral proteins,in turn,mediate oxidative stress,promote the expression of inflammatory factors,such as tumor necrosis factor-α,interleukin (IL)-6,and IL-8,and aggravate the degree of hepatic fibrosis,which exacerbates insulin resistance[49,50].Insulin resistance plays a vital role in MS[47].This evidence suggests that HCV may affect glucose metabolic homeostasis and increase the risk of T2D through intermediate pathways,such as hepatic steatosis,hepatic fibrosis,and cirrhosis.However,due to the assumption of the exclusivity of MR,SNPs associated with known risk factors for T2D,such as fatty liver,liver fibrosis,and cirrhosis,were excluded as confounding factors,which may be the main reason for the negative MR results.
This study suggests that CHB infection is associated with a reduced risk of T2D,which differs from the results of most clinical studies.Current studies support the notion that HBV infection is not an independent risk factor of T2D[19].A Taiwanese study involving 1233 individuals found no significant differences in the prevalence of diabetes and glucose intolerance between asymptomatic chronic HBV-infected individuals and a non-HBV control group[30].This is similar to the findings of another Taiwanese study that concluded that HBV itself does not confer a predisposition to diabetes[51].Liuetal[52] supported this view from a serological perspective as they found that the serological status of HBV antigen (HBsAg) and hepatitis B surface antibody (HBsAb) was not associated with diabetes.Moreover,HBV infection did not increase the risk of macrovascular complications in diabetes mellitus[53].
Although most of the current literature suggests that CHB is not associated with T2D risk,some studies support CHB as a potential protective factor against T2D.A study of retired Chinese women showed that a HBsAb-positive status was associated with better metabolic status and a lower incidence of diabetes mellitus[54].Another study found that a high HBV load is associated with a reduced risk of hepatic steatosis,a mechanism by which HBV reduces the risk of T2D[55].This implies that a high HBV load may be an element of the reduced risk of T2D in patients with CHB rather than HBsAb positivity alone.However,most patients with CHB are treated with antiviral drugs,including tenofovir or entecavir,which reduce the HBV load in the body.As the viral load decreases,the role of HBV in regulating fat metabolism and reducing the risk of diabetes is significantly diminished,which may be the main reason why the results of this MR analysis differ from those of clinical studies.
The potential protective effects of HBV infection against obesity and MS provide indirect evidence that supports our findings.A cross-sectional study in China showed that the prevalence of MS was significantly lower in patients infected with HBV than that in non-infected patients (11.64%vs12.66%)[56].A Taiwanese clinical study included 3587 patients with HBV infection without cirrhosis and found that high HBV viral load was associated with a reduced risk of extreme obesity (OR=0.30;95%CI: 0.13-0.68) and centripetal obesity (OR=0.53;95%CI: 0.34-0.82)[57].HBV infection may reduce the risk of hepatic steatosis by modulating lipid metabolism,which in turn reduces the risk of obesity and MS.A metaanalysis showed that the prevalence of steatosis was lower in CHB than that in the general population (OR=0.81;95%CI: 0.71-0.920)[58].Another study reported that the prevalence of non-alcoholic fatty liver disease was lower in patients with HBV infection than that in non-infected patients[59].A clinical study in Taiwan further showed that patients with positive HBsAg possessed lower hypertriglyceridemia (OR=0.59;95%CI: 0.52-0.66) and low-density lipoproteincholesterol levels (OR=0.86;95%CI: 0.79-0.93) than those with negative HBsAg[60].Considering that steatosis is an essential factor that leads to the progressive impairment of glucose metabolism[61],the role of HBV in regulating hepatic lipid metabolism also contributes to the regulation of glucose metabolic homeostasis.This evidence suggests that HBV infection is associated with a lower risk of obesity and MS,and that the primary mechanism may be the modulation of hepatic fat metabolism,which corroborates our view.
Notably,the risk of T2D increases when CHB progresses to cirrhosis.A meta-analysis of 15 clinical studies showed that the incidence of diabetes was comparable between patients with non-cirrhotic CHB and those with asymptomatic HBV carriers and non-HBV[11].In contrast,patients with hepatitis B cirrhosis had a significantly increased risk of T2D (OR=1.99;95%CI: 1.08-3.65)[11].Epidemiological studies showed that only 2%-4% of patients infected with HBV each year worldwide will develop compensated cirrhosis,and only 1.5%-4% of compensated cirrhosis will further develop into decompensated cirrhosis[62].Therefore,most patients with CHB do not have compensated or decompensated cirrhosis,which may explain why most clinical studies have not found an association between CHB and T2D.In summary,CHB is associated with a reduced risk of T2D;however,this association is limited by HBV load and cirrhosis.It weakens or disappears when patients with CHB receive antiviral therapy,and reverses when CHB progresses to cirrhosis.
Few studies have investigated the relationship between T2D and other VH,such as hepatitis A,D,and E.Linetal[63] found that HAV infection was associated with an increased risk of diabetes (OR=1.13;95%CI: 1.08-1.18).However,HAV vaccination and successful HAV immunization were not associated with the risk of diabetes;therefore,they concluded that HAV infection was unlikely to cause diabetes[63].Zitellietal[64] found that among patients with chronic HCV infection receiving antiviral therapy,the incidence of diabetes was 3.65 times higher in HEV-positive patients than that in HEV-negative patients,suggesting that HEV is a potential risk factor for diabetes mellitus in chronic HCV-infected individuals.In summary,there are insufficient studies elucidating the effects of hepatitis caused by HAV,HDV,and HEV infections on T2D,and this issue needs to be further explored in subsequent studies.
Our study has some limitations.First,the data on CHB and CHC were derived from East Asians;therefore,the results mainly illustrate the effect of CHB and CHC on T2D among East Asians,and it is not yet clear how they affect other races.Second,the GWAS only provided an overall dataset on VH among Europeans with availability;it did not include a dataset of different types of VH.Therefore,the results of this study can only infer that VH is not associated with T2D risk in Europeans,and cannot explain the effects of different types of VH on T2D risk among Europeans.Third,data on HAV,HDV,and HEV were unavailable in the GWAS;therefore,their effects on T2D risk were not assessed.Fourth,our data were derived from the GWAS;therefore,it was impossible to stratify the analysis for populations with different viral loads.Given these limitations,we expect future studies to improve.First,we recommend continuing to promote human genome studies worldwide,and provide more comprehensive data for MR analysis of different races.Second,we recommend conducting stratified randomized controlled trials to explore the specific effects of the different types,stages,and viral loads of VH on T2D.
CONCLUSlON
This MR analysis showed that neither VH among Europeans nor CHC among East Asians were associated with T2D risk,whereas CHB was associated with reduced T2D risk among East Asians.Although VH among Europeans and CHC among East Asians are not associated with T2D risk,focusing on blood glucose in patients with CHC is still relevant for the early detection of T2D induced by CHC-mediated pathways of hepatic steatosis,liver fibrosis,and cirrhosis.Further studies are needed to explore the causal relationships and mechanisms between different types of VH and T2D.
ARTlCLE HlGHLlGHTS
Research background
The causality between viral hepatitis (VH) and type 2 diabetes (T2D) remains unclear.
Research motivation
In this study,a Mendelian randomization (MR) analysis was applied to determine the causality between VH and T2D from genome-wide association study data.
Research objectives
We used a MR to identify the causality between VH,chronic hepatitis B (CHB),chronic hepatitis C (CHC) and T2D from genome-wide association study data.
Research methods
Two-sample MR was performed to obtain the causality between VH,CHB,CHC and T2D.Summary statistics from the FinnGen were used for VH,BioBank Japan Project was used for CHB and CHC,and the European Bioinformatics Institute and FinnGen were utilized for T2D.
Research results
The MR analysis showed no significant causal relationship between VH and T2D in Europeans [odds ratio (OR)=1.028;95% confidence interval (CI): 0.995-1.062,P=0.101] as well as between CHC and T2D in East Asians (OR=0.949;95%CI: 0.931-0.968,P< 0.001),while there was a negative causal association between CHB and T2D among East Asians (OR=0.949;95%CI: 0.931-0.968,P< 0.001).These MR analysis results showed no horizontal pleiotropy or heterogeneity (P> 0.05),and they were robust.
Research conclusions
Among East Asians,CHB is associated with a reduced T2D risk,but this association is limited by hepatitis B virus (HBV) load and cirrhosis.Although CHC among East Asians are not associated with the risk of T2D,focusing on blood glucose in patients with CHC is still relevant for the early detection of T2D induced by CHC-mediated pathways of hepatic steatosis,liver fibrosis,and cirrhosis.
Research perspectives
Whether different categories of VH,especially CHB and CHC,are associated with the risk of T2D remains controversial.CHB is associated with a reduced T2D risk among East Asians,but this association is limited by HBV load and cirrhosis.Although VH among Europeans and CHC among East Asians are not associated with T2D risk,focusing on blood glucose in patients with CHC is still relevant for the early detection of T2D induced by CHC-mediated pathways of hepatic steatosis,liver fibrosis,and cirrhosis.
FOOTNOTES
Co-first authors:Yun-Feng Yu and Gang Hu.
Author contributions:Yu YF conceived and designed the study;Yu YF and Hu G participated in data processing and statistical analysis;Yu YF,Hu G,Yang XY,and Wu JY drafted the manuscript;Hu G,Yang XY,Wu JY,and Yu R contributed to data analysis and interpretation;Yu YF,Tong KK,Yang XY,and Yu R supervised the review of the study;and all authors seriously revised and approved the final manuscript.
Supported byNational Natural Science Foundation of China,No.U21A20411.
lnstitutional review board statement:Despite our study was an original research,this work just used genome-wide association studies statistics from public available databases for Mendelian randomization analysis,and we did not collect any new human data.As this study did not involve any human studies and/or animal experiments,the institutional review board approval was not required for our research.
lnformed consent statement:Despite our study was an original research,this work just used genome-wide association studies statistics from public available databases for Mendelian randomization analysis,and we did not collect any new human data.As this study did not involve any human studies and/or animal experiments,the informed consent form was not required for our research.
Conflict-of-interest statement:All the authors report no relevant conflicts of interest for this article.
Data sharing statement:All GWAS data that support the findings of this study are openly available in the BioBank Japan Project (https://biobankjp.org/en/),European Bioinformatics Institute (https://www.ebi.ac.uk),and FinnGen (www.finngen.fi/fi).
Open-Access:This article is an open-access article that was selected by an in-house editor and fully peer-reviewed by external reviewers.It is distributed in accordance with the Creative Commons Attribution NonCommercial (CC BY-NC 4.0) license,which permits others to distribute,remix,adapt,build upon this work non-commercially,and license their derivative works on different terms,provided the original work is properly cited and the use is non-commercial.See: https://creativecommons.org/Licenses/by-nc/4.0/
Country/Territory of origin:China
ORClD number:Yun-Feng Yu 0000-0002-7309-5608;Gang Hu 0000-0002-6252-0082;Ke-Ke Tong 0000-0001-6852-3914;Xin-Yu Yang 0000-0001-6124-9166;Jing-Yi Wu 0009-0000-1093-9327;Rong Yu 0009-0005-0840-2797.
S-Editor:Wang JJ
L-Editor:A
P-Editor:Zheng XM
杂志排行
World Journal of Diabetes的其它文章
- Elucidating the cardioprotective mechanisms of sodium-glucose cotransporter-2 inhibitors beyond glycemic control
- Genotype-based precision nutrition strategies for the prediction and clinical management of type 2 diabetes mellitus
- Emerging and multifaceted potential contributions of polyphenols in the management of type 2 diabetes mellitus
- ldentification of hub genes associated with Helicobacter pylori infection and type 2 diabetes mellitus: A pilot bioinformatics study
- Experience of humanistic nursing in hemodialysis nursing for patients with diabetic kidney disease
- Analysis of the influencing factors and clinical related characteristics of pulmonary tuberculosis in patients with type 2 diabetes mellitus
