Competencies of the nurses in the limitation of therapeutic effort in the intensive care unit: An integrative review
2024-02-27ElviVnessPchecoRoysKellyDinElizbethVillrrelCntilloCesrAvilesGonzlez
Elvi R. ,Vness C.Pcheco-Roys ,Kelly J. ,Din C. , Y. ,Elizbeth Villrrel-Cntillo ,Cesr I.Aviles Gonzlez
aNursing Department,Universidad del Norte,Barranquilla,Colombia
b Nursing Program,Faculty of Health Sciences,Universidad Popular del Valledupar,Colombia
c Valledupar,Valledupar,Colombia
d Hospital Universidad del Norte,Soledad,Colombia
e Department of Medical Sciences and Public Health,University of Cagliari,Cittadella Universitaria di Monserrato,Cagliari,Italy
Keywords:
ABSTRACT Objective:Nurses inevitably encounter patients who require care aimed at limiting therapeutic effort (LTE),even though many of them are not prepared to provide support to individuals with terminal illnesses and their families.One of the contexts in which the LTE is considered is the intensive care unit (ICU).This review is to describe the competencies for the execution of a nursing professional role in the LTE in the ICU.Method: An integrative review of the literature published between the years 2010 and 2023.The search was carried out in five databases: Medline,Wiley Online Library,SciELO,ScienceDirect,and Web of Science.The Critical Appraisal Skills Programme in Spanish was used as the template for study evaluation.The methodology of the Oxford Center for Evidence-Based Medicine(CEBM)was used to assess the level of evidence and the degree of recommendation.Result:A total of 25 articles in a wide range of studies were included.The findings suggest that the competencies for LTE in the ICU are direct patient care,family-centered care,and the role of the nurse within the team.However,more high-quality studies are needed to confirm these conclusions.Three categories were identified: (a) competencies as defender agent between the patient,his family,and the interdisciplinary team;(b) competencies for decision-making in limiting the therapeutic effort;and (c)competencies for nursing therapeutic interventions at the end of life.Conclusion:The competencies of the nursing professionals who work in the adult ICU in the LTE are essential to the patient’s quality of life,dignity of their death,and comprehensive family support for coping with grief.
What is known?
· The study of competencies is a topic that is being explored,and in Colombia,the competencies for limiting therapeutic effort in adult intensive care units are not defined.
· In Colombia,the role of the nurse in limiting therapeutic effort is an unclear practice,since there are no protocols that guide the care of these patients and their families.
What is new?
· This article provides a description of the competencies for limiting therapeutic effort based on current evidence.
· The findings of this study indicate that defining competencies is essential to provide quality,humanized,and ethical care to the patient and their family at the end of life.
1.Introduction
Nursing professionals,regardless of the environment in which they work,will encounter people who require care aimed at limitation of therapeutic effort (LTE),although most of them are not prepared to provide support to people with illnesses in the terminal and their families [1].One of the contexts in which the LTE is considered is the Intensive Care Unit(ICU);this situation represents a dilemma for the professional,since it contradicts the curative objective for which these care units were designed,allowing them to be increasingly used by older persons with chronic diseases at high risk of decompensation,whose possibility of recovery is reduced [2].
The literature reports that the purposes of LTE are aimed at dignified and humanized care,at the patient’s physical comfort,including the relief of pain and other related symptoms,promoting the reduction in suffering and support for both the patient and the family [3].In addition,the role of the nursing professional is highlighted as one of the main actors in the provision of interventions in the practice of LTE [4].
Likewise,it is evident that the lack of education,regulations,and description of competencies in the practice of LTE can cause the nursing professional to find it difficult to face the inevitable death thus contributing to the suffering of terminal patients due to inappropriate communication,lack of compassion,or personal aspects facing it [5,6].
The literature review reports scarce studies on the research topic;it is even claimed that the nursing competencies in the LTE are not fully described [7].This coincides with the situation at the national level described by Aristizábal[6],which states that LTE in Colombia is an unclear practice,since its execution is independent in the different care units and is also influenced by moral aspects.In addition to this,there is a lack of regulations that regulate the practice,restricting it to isolated norms [8].
The current scenario in which palliative care has to be developed encounters the difficulty of a lack of alignment of specific training in nursing,and the lack in curricula and postgraduate training is evident.Training is required that covers the wide range of knowledge and skills necessary for nurses to be able to face the care situations generated by these end-of-life patients in the ICU [9].
In addition,professional practice in palliative care must be considered within the framework of a conceptual model,ethical principles,the application of the scientific method,and the development of care plans in the process of critical thinking,clinical judgment,decision-making,and problem-solving [10].It is necessary to advance in thoughtful practices based on the best available scientific evidence that allows nurses to provide the best possible care to patients and their families in LTE [9].
According to the ETHICUS Study [11] related to LTE practices in Europe,nursing professionals’ participation in decision-making is low,being carried out mostly by doctors and in nursing only in 2%of cases.Therefore,the professional role of the nurse supporting LTE within the care team should be clarified.For this,nursing competencies in Palliative Care and in ICU LTE must be defined,in particular,which makes it possible to provide an advanced quality practice that guarantees excellence in the care provided to patients and their families and that delimits the scope of action.Identifying competencies will have a direct effect on not only care but also training,management and research needs.
It is necessary for the nursing discipline to acquire competencies (skills,behaviors,knowledge,skills,and attitudes)aimed at care in the LTE in ICU,given the knowledge gaps evidenced in the literature review[12].This led to the formulation of the problem based on the question:What are the competencies of the nursing professional in the LTE in ICU?This research aimed to describe the necessary skills for the execution of the role in LTE in ICU.The results of this study seek to contribute to the quality of care and professional productivity during the care process as well as humanization and dignity at the end of life.
2.Methods
Mendes et al.[13] describe the general concepts and six stages for the development of the integrative review as well as relevant aspects of the applicability of this method for research in health and nursing [14-16].1) Identification of the topic and selection of the hypothesis or research question for the preparation of the integrative review.2)Establishment of inclusion and exclusion criteria for studies/sampling or literature search.3) Definition of the information to be extracted from the selected studies/categorization of the studies.4) Evaluation of the studies included in the integrative review.5) Results analysis.6) Presentation of the review/synthesis of knowledge.
(1) The study was identified based on the difficulties found in the literature in the area of competencies,palliative care and LTE in adults in the ICU in the Colombian context.In the literature,the description of the general competencies of nursing professionals in Colombia was found,but the specific competencies for LTE are not described.In addition,from the legal point of view,it does not define the framework of action of the nurse for the LTE.Likewise,in the contents of university training,the subject is not specifically addressed,which leads to little knowledge of the graduates and deficiencies in nursing care of terminally ill patients in the ICU.All of the above led the authors to carry out an integrative review of the literature published from 2010 to 2023 on the competencies of the nursing professional for LTE in the ICU.
(2) During the second stage,for the search and selection of the papers,the following databases were used: Medline,Wiley Online Library,SciELO,ScienceDirect and Web of Science.
The specific search equations were carried out using the combination of keywords corresponding to Health Sciences Descriptors(DeCS)and Boolean operators.The DeCS/MeSH terms used were as follows: palliative care,role of the nurse,stopping treatment,intensive care,advance directives,do not resuscitate,limitation of therapeutic effort,and nursing.Since the term Limitation of Therapeutic Effort is not available in the DeCS,the term Treatment Withholding (restriction or withdrawal of treatments to prolong the patient’s life) was used.According to the above,the following search equations will be determined:
· Withholding treatment AND nurse’s role AND Critical care.
· Limitation of therapeutic effort AND Nursing.
·Withholding treatment OR Nursing care AND Critical care.
·Palliative care AND nurse’s role.
The search process was adjusted using the following criteria:year,from 2010 to 2023;publication/document type,paper;access type,full text;journal category,nursing journals;search fields,title/abstract;species,humans;and language,English and Spanish.
The inclusion criteria were follows: original articles related to the concepts of competencies,nursing,adult ICUs,and LTE,with a qualitative,quantitative and/or mixed approach that provides empirical evidence,systematic reviews,or meta-analyses that report a good level of evidence.Incomplete articles,grey literature,abstracts,editorials that do not provide empirical evidence,duplicate papers,and papers by nurses working in neonatal and pediatric ICUs were excluded.
(3) In the third stage,the search process was carried out in the indexed databases and the selection of the studies.Initially,when using the entire search,a total of 92,328 papers were identified.When applying the criteria (year,type of publication,and type of access),92,098 were eliminated,and 230 articles remained.Of these,151 articles were eliminated after applying all the criteria,and 79 papers were selected.Subsequently,the full text of these papers was read,and a total of 48 papers were chosen.Once again,the complete and comprehensive text was read,eliminating 23 papers that did not show elements of the competencies for the LTE of nursing professionals who work in the ICU in their results.Finally,25 papers were included and distributed in the databases.(see Fig.1).Subsequently,the information from the publications was extracted and organized in a data table:database,journal,country and year of publication,title,author(s),aim,approach and methodological design and sample,results,and identified competencies.
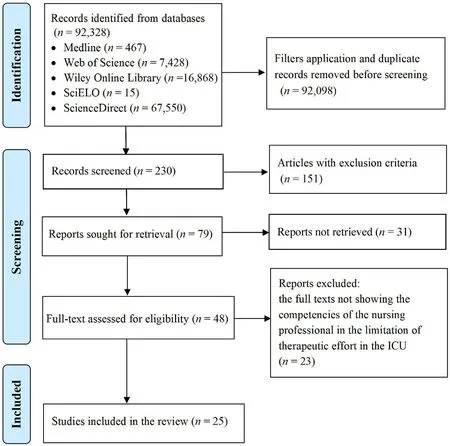
Fig.1. Process of search and selection of articles.
(4) In the fourth stage (analysis of the information),the organization and critical reading of the selected papers was carried out,taking into account the methodological approach of each of these.For the critical reading of the selected articles,the Critical Appraisal Skills Programme (CASP) checklists [17] in Spanish (CASPe) were used.To assess the level of evidence and the degree of recommendation of the articles,the methodology of the Oxford Center for Evidence-Based Medicine (CEBM) was used [18].
(5) During the fifth stage,the approaches and the grouping of common findings of the different theoretical referents identified in the scientific evidence were analyzed,as well as the concept of nursing professional competencies in LTE in ICU adopted by the author to the context of this research.
(6) Finally,in the sixth phase,the results were described,responding to each of the objectives set out in the research,final describing the limitations,conclusions,and recommendations.
For the study presented,the authors considered the Declaration of Helsinki [19];the endorsement of the ethics committee of the Universidad del Norte was obtained according to act No.208 of May 2020.
3.Results
3.1.Characterization of included articles
A total of 25 articles were selected and critically evaluated.The reported literature includes various countries,which is an aspect that allowed the enrichment of the review.Table 1 specifies the characteristics and main findings of each articles included.
3.2.Evaluation of the study quality
Overall,10 were classified at level 3a and a grade of recommendation B;8 have a level of evidence of 5 with a grade of recommendation D;and finally,the remaining 6 were classified at level 4 with a grade of recommendation C.This demonstrates that the findings do not allow the results to be generalized in the Colombian context,but they do represent a relevant contribution to the study phenomenon(Table 1).
3.3.Analysis and integration of findings
For the authors,the competencies of the nursing professional in the LTE in Adult ICUs integrate the skills,knowledge,attitudes,and values that are required to act as a defender of the patient and his family in front of the interdisciplinary team during the decisionmaking process and the execution of therapeutic interventions that favor the dignified death of the patient and provide family support for coping with grief (See Fig.2).
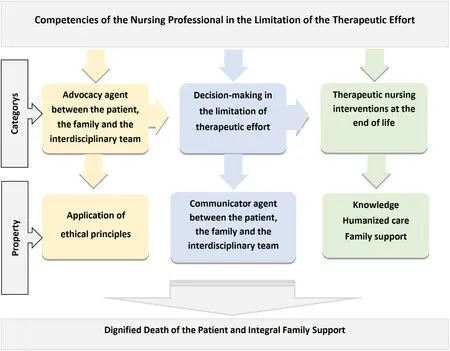
Fig.2.Nursing professional competencies in LTE,according to the authors.Source: López and Pacheco.Competencies of the Nursing Professional in the Limitation of Therapeutic Effort in the Intensive Care Unit (2020).
3.3.1.Category 1
3.3.1.1.Competencies as an advocate between the patient,the family,and the interdisciplinary team
The nurse is an“advocate of the wishes of the patient,defender of their state and responsible for ensuring their well-being,and that of their family.” [7,20,31].Likewise,she is a “defender and safeguard”;“The nursing professional is the one who accompanies the patient the longest and who interacts the most with the family,providing 24-h coverage to meet their needs.” [31].This competence involves “ensuring the quality and continuity of care,ensuring that the patient understands the information provided by the health team”[28].On the other hand,this competence implies “defending the rights and dignity of patients;and in case there is an opposition between the wishes of the patient and those of the family,the nursing professional must lead the management processes so that,depending on the need,interventions are carried out by the medical board and the Institutional Ethics Committee [43].In this order,the category property is defined below.
3.3.1.2.Application of ethical principles
The literature reports that “Decision making at the end of life,such as withdrawal and discontinuation of life-sustaining treatment,is difficult and can raise ethical issues.”[4].Within the ethical conflicts,it is highlighted that“the order to withdraw life support,on occasions,entails the non-application of care measures that could have maintained the patient’s comfort,such as analgesia,postural mobilizations and nutrition” [31].It is evident in the findings that “nurses feel relieved with the decision of LTE in situations of therapeutic uselessness;however,feelings of guilt may appear and some nurses may even feel like executioners when applying these measures” [31].This shows that currently “the practices in the LTE are sometimes permeated by the values,attitudes and beliefs of those who implement it.” [32].
For the application of LTE in the ICU,it is necessary that the professional has a plan that allows to provide the patient at the end of life,palliative care with the intention of providing death with the least discomfort and suffering for him and his family,which is developed in accordance with the patient’s wishes as well as clinical,ethical and cultural standards.In this way,such a plan “contributes to solving the dilemmas based on the principles of beneficence and non-maleficence,without involving personal sentiment” [43].Therefore,the importance of “adapting the ICU areas turning them into more humanized services,equipped with trained personnel,ensuring in this way the comprehensiveness of care,shared decision-making and the resolution of frequent ethical dilemmas” [29,43].
Starting from the ethical principles of the discipline,it is common to think of the nursing professional as a manager of ethical principles in clinical practice.For this reason,it should be noted that even when it is believed that one acts under the principle of beneficence,if this exercise is permeated by the feelings,values,and experiences of the professional about death,the mistake of not covering the needs of the person in a situation of LTE can be made.It was also identified that nursing professionals act as an intercessory agent between the patient,the family,and the interdisciplinary team to ensure and advocate for the rights of the patient,the dignity of his death,and the satisfaction of the needs of the family in a more objective way.
3.3.2.Category 2
3.3.2.1.Competencies for decision making in the limitation of therapeutic effort
In Colombia and some countries reported in the literature,decision-making for the establishment of LTE belongs to the medical domain.However,the nursing professional is “the main manager of multiple care interventions at the end of life for patients,which derive from decisions in the practice of LTE,such as analgesia,nutrition,and mechanical ventilation;in addition to providing support to the patient and his family,as well as staying by his side until his death”[4].This is why nursing plays“an important role in decision-making,because it occupies a privileged place in the health team that is related to the ability to interact with the team,family members and the patient.” The need for nursing professional participation in decision-making is evident within the findings.Some authors state that this “should be carried out after discussion among all team members” [21].As an important element,the property of the competence described is defined below.
3.3.2.2.Communicator agent between the patient,the family and the interdisciplinary team
Communication constitutes a fundamental axis when it comes to defining competencies for the nursing professional in LTE in the ICU.According to the findings obtained from the literature review,the nursing professional should “stand out as a facilitator of communication between the parties involved;coordinate the exchange of relevant information,so that families can understand the patient’s condition” [28].Therefore,it is necessary to develop the ability to “listen,facilitate communication and provide information” [28].In addition,it ought to include verbal and non-verbal actions that facilitate and ensure the effective communication of relevant patient information between the health team and the family,generating empathy,trust,respect,and adequate decisionmaking.
Regarding the competencies for decision-making in the establishment of the LTE,the literature reports a correlation with the Colombian context,where the doctor is described as the actor responsible for this important decision.
However,it highlights the importance of the nursing professional within this process,since they are responsible for providing care aimed at meeting the needs of the patient and his family at the end of life.In addition,he acts as an intermediary between all the actors involved;his communication skills contribute to the dignity of the patient’s death and provide support to the family.
3.3.3.Category 3
3.3.3.1.Competencies for therapeutic nursing interventions at the end of life
This nursing competence is related to“those direct interactions with patients and families at the end of life to promote health,wellbeing and/or improve quality of life,characterized by a holistic perspective from the management of advanced nursing,the state of health and disease”[2].Likewise,therapeutic nursing interventions in LTE“imply a change in the care approach,from highly aggressive critical care (intubation,mechanical ventilation,etc.),to comfort and end-of-life care,whose purpose is to dignify death.” [4].
That is why the articles report the need to carry out interventions in accordance with the patient’s situation,which refers to“physical care,hydration,comfort,prevention,control and relief of symptoms,adaptation of the environment,bathing,hair care,oral care,nutrition,passive limb exercises,pressure injury prevention and effective pain management,as well as the extraction of the orotracheal tube,sedation and aspiration according to the individual need of the person” [22,27,30].
Therapeutic interventions at the end of life require the nursing professional “to spend most of the time with the patients,to have frequent and regular contact that allows them to develop a special connection with them,facilitating individual attention that leads to the relief of suffering,to maintain dignity and provide comfort care.This psychosocial and spiritual care for patients goes hand in hand with direct physical care and practice” [31].Next,the properties that involve this competence are defined.
3.3.3.2.Humanized care,knowledge,and family support
(1) Humanized care:This becomes a philosophy of life applied in professional nursing practice,which can be defined as “an instrument to relate to and help others;It implies a responsibility towards the patient,favoring individualized attention,where the technical and the human complement each other to deliver comprehensive care that responds in a personalized way to their needs”[4].The foregoing involves the development of “empathy,respect for beliefs and the participation of humanistic and affectionate practices that promote overcoming dehumanization” [4,23,30].
(2) Knowledge for the implementation of the LTE: The nursing professional who provides LTE care“requires knowledge and clinical experience in all the fundamental areas of nursing”[28].In addition,they must have “clinical experience,humanization,technical qualification,ethical knowledge,bioethics (which favors the ability to solve conflict) and formal education in palliative care,thus favoring comprehensive care and shared decision-making”[25].In this sense,it is important that “the preparation of documentation (protocols and guides) provide evidence transferable to the ICU for end-of-life care and that are adapted to the Colombian cultural and regulatory context” [26].
(3) Family support: Nurses acquire a relevant role in caring for family members due to their permanence with patients,which is a situation that leads to “seeing the family as a resource for care and attention,in a therapeutic relationship that includes respect for practices and cultural rituals as an important form of family support” [26].It is the nursing professional“who is in charge of providing support,helping to understand the patient’s condition,providing clear and understandable information to the relative of the subject of care,facilitating the decision-making process decision and acceptance of death” [21].
Thus,therapeutic nursing interventions at the end of life contemplate the direct care of both the patient and their relatives.For this,the nursing professional requires skills that favor the holistic and human care of the subject of care.These interventions involve physical,functional,social,and spiritual aspects that allow the professional to address the different dimensions of the individual and their family based on specific knowledge that leads to providing care with the technical-scientific quality that they deserve.Furthermore,this leads to the transition from the curative to the palliative approach,which facilitates broadening the perspective of professional nursing care in the LTE in ICU.
4.Discussion
This integrative review identified,systematized,and synthesized a narrative summary of evidence on LTE in the ICU.The findings suggest that nurses in critical situations such as end-of-life care for patients in the ICU must carry out a comprehensive approach,which is why scientific knowledge,experiences,and specific skills for LTE are necessary[23].Among their competencies,they must serve as intermediaries for decision-making between the patient,their family,and the health work team with the aim of providing ethical and humanized care [20,24-26].
The nurse participates in decision making,in the family support relationship,and in patient-directed care [7,20].Other authors differ by reporting on the low representation of nursing in decisionmaking related to the limitation of treatment or life support [32,44,45].Although they are not the ones who make the decision to establish LTE,they contribute to seeking consensus and providing care aimed at comforting the patient [23,31,32].
Likewise,nurses perceive the need to respect the patient’s dignity,provide comfort-oriented care,and promote the inclusion of the family in care[32].Another key theme in this review was that nurses should respect religious and spiritual beliefs,support the patient and family,and allow unrestricted visits from family and friends[25].Nurses have direct involvement in the care of patients at the end of life [21].Our review identified several interventions that nurses carry out in the care of patients at the end of life [31-33].Planning care goals,good communication,pain relief,and a calm environment favor a dignified death.
From this perspective,nursing provides a humanizing and ethical vision of care.Challenges for nurses include being present,providing and interpreting information,and helping family members make end-of-life decisions aligned with patients’ wishes.Effective communication is key to resolving conflicts and differences to ensure that the family is satisfied with the care provided [34].
The health crisis caused by COVID-19 that began in 2020 reaffirmed the competencies of nurses for LTE that coincide with those described in the present study.In this sense,et al.[46] highlight the importance of adapting palliative care to emergency and pandemic situations due to the rapid deterioration of some patients.Therefore,the nurse must be on the front line to help in decision-making,care and accompany the patient and his family.
The COVID-19 pandemic led to the recognition of the need to provide high-quality critical care with the need to integrate palliative care into treatment strategies for patients with uncertain prognosis and their families,as it provides comfort,relief,and dignity.This integration made it possible to establish care objectives early;the nurse,through continuous evaluation,is able to detect those patients who are sensitive to LTE.This also made it easier to moderate communication with families and provide information about treatment expectations [45].Akgün et al.[47]highlight the importance of palliative care to improve communication with the family and reduce the feeling of abandonment,isolation or emotional relief that they may feel.
Most of the studies in the present review were of moderate quality,and although they provided knowledge and understanding of the competencies for LTE in the ICU,these findings are limited due to the lack of generalizability of their results.
5.Limitations
In analyzing the findings of this integrative review,it is necessary to explain the limitations of the research.
First,since most of the studies included in this review were conducted in different cultural contexts and healthcare models,therefore,their application to practical contexts,such as the Colombian context,requires adaption.
Another aspect to take into account is that few articles were found that address or identify the skills in LTE in Adult ICUs,thus evidencing that the study phenomenon has not been widely explored.Finally,because the search process for this research was limited to Spanish and English,it was possible to exclude evidence from other research related to the study phenomenon in other countries,so it is suggested in future research to expand the search criteria.
6.Conclusions
This study described the competencies of the nursing professional for LTE in the ICU.It was identified that the study phenomenon is in the descriptive and exploratory phase,since most of the articles report levels of evidence 3a and 4 with grades of recommendation B and C,respectively;this suggests the need to carry out primary research,which broadens the approach on the subject.The results show that the development of palliative care has allowed the research problem to be addressed more widely at the international level than in the national context,where despite its relevance;it is still in the exploration phase.
Three categories were identified to define the competencies of the nursing professional who works in adult ICUs in the LTE: (a)advocacy agent between the patient,the family,and the interdisciplinary team with a property that refers to the application of ethical principles,(b)decision making in the LTE where the nursing professional stands out as the main attribute as a communicator agent between the patient,the family and the interdisciplinary team;and (c) therapeutic nursing interventions at the end of life,being humanized care,knowledge and family support;these are the properties that are required for the development of this competence.
The literature reports that decision making for the establishment of LTE is mainly in the medical domain,but at the same time,it highlights the nursing professional as responsible for ensuring the quality and continuity of care and as the main manager of endof-life care interventions due to its ability to act as an intermediary between the patient,their family,and the health.
CRediT authorship contribution statement
Elvia R.Conceptualization,Methodology,Validation,Formal analysis,Investigation,Data curation,Writing -original draft.Vanessa C.Pacheco-Roys:Conceptualization,Methodology,Validation,Formal analysis,Investigation,Data curation,Writing -original draft.Kelly J.-Ahumada:Validation,Formal analysis,Investigation,Data curation,Writing -original draft.Conceptualization,Methodology,Validation,Formal analysis,Investigation,Data curation,Writing -original draft,Writing -review &editing.Conceptualization,Methodology,Validation,Formal analysis,Investigation,Data curation,Writing -original draft,Writing -review &editing.Elizabeth Villarreal-Cantillo:Investigation,Writing-original draft,Writing-review&editing.Cesar I.Aviles Gonzalez:Writing-original draft,Writingreview &editing.
Funding
This research received no external funding.
Declaration of competing interest
The authors declare no conflict of interest.
Appendix A.Supplementary data
Supplementary data to this article can be found online at https://doi.org/10.1016/j.ijnss.2023.12.011.
杂志排行
International Journal of Nursing Sciences的其它文章
- Editorial Board of International Journal of Nursing Sciences
- Chinese Abstract
- Corrigendum to “Relationship between nurses’ perception of professional shared governance and their career motivation in Egypt:A cross-sectional study” [Int J Nurs Sci 10/4 (2023) 485-491]
- 《国际护理科学(英文)》进入中科院分区护理类2 区
- 关于翻译量表使用授权的问答
- Summary of Guide for Authors