Colonoscopy plays an important role in detecting colorectal neoplasms in patients with gastric neoplasms
2024-01-26XuRuiLiuZeLinWenFeiLiuZiWeiLiXiaoYuLiuWeiZhangDongPeng
Xu-Rui Liu,Ze-Lin Wen,Fei Liu,Zi-Wei Li,Xiao-Yu Liu,Wei Zhang,Dong Peng
Abstract BACKGROUND Gastric cancer (GC) and colorectal cancer (CRC) are the fifth and third most common cancer worldwide,respectively.Nowadays,GC is reported to have a potential predictive value for CRC,especially for advanced CRC.AIM To evaluate the necessity of colonoscopy for gastric neoplasm (GN) patients.METHODS Four databases,including PubMed,EMBASE,the Cochrane Library,and Ovid,were used to perform the search strategy on May 2,2023.The prevalence of colorectal neoplasms (CRN) and baseline characteristics were compared between the neoplasm group and the control group.Continuous variables are expressed as the mean difference and standard deviation.Relationships of categorical variables in the two groups are expressed as odds ratios (OR) and 95% confidence intervals (95%CIs).Subgroup analysis according to different kinds of GNs was conducted for more in-depth analysis.The results of this study are represented by forest plots.Publication bias was evaluated by a funnel plot.All data analyses were performed by STATA SE 16.0 software.RESULTS A total of 3018 patients with GNs and 3905 healthy controls (age and sex matched) were enrolled for analysis.After comparing the prevalence of CRNs between the two groups,CRNs were detected significantly more frequently in GN patients than in controls (OR=1.69,95%CI=1.28 to 2.23,I2=85.12%,P=0.00),especially in patients with GC (OR=1.80,95%CI=1.49 to 2.18,I2=25.55%,P <0.1).Moreover,other risk factors including age (OR=1.08,95%CI=1.00 to 1.17,I2=90.13%,P=0.00) and male sex (OR=2.31,95%CI=1.26 to 4.22,I2=87.35%,P=0.00),were related to the prevalence of CRNs.For patients in the GN group,body mass index (BMI,OR=0.88,95%CI=0.80 to 0.98,I2=0.00%,P=0.92) and smoking (OR=1.03,95%CI=1.01 to 1.05,I2=0.00%,P=0.57) were protective and risk factors for CRNs,respectively.CONCLUSION Patients are recommended to undergo colonoscopy when diagnosed with GNs,especially GC patients with a low BMI and a history of smoking.
Key Words: Gastric neoplasm;Gastric cancer;Colorectal neoplasm;Colonoscopy
INTRODUCTION
According to the International Agency for Research on Cancer,gastric cancer (GC) is the fifth most common cancer worldwide,accounting for 1.1 million new cancer cases[1,2].Helicobacter pylori(H.pylori) infection is the greatest known risk factor for GC and shows a positive association with gastric polyps[3,4].Gastric polyps are asymptomatic lesions found incidentally during endoscopy that may develop into GC.Gastric neoplasm (GN) is a general term for gastric adenoma and GC.
Similar to GC,colorectal cancer (CRC) is a gastrointestinal malignant disease that develops from colorectal polyps[5].Early colorectal polyps can be removed under colonoscopy,which significantly decreases the incidence of CRC[6,7].Some characteristics,including age,male sex,family history,obesity,and red meat intake,have been reported to have predictive value for colorectal neoplasms (CRNs) (including colorectal polyps and CRC)[8-10].Therefore,regular colonoscopy in high-risk patients with CRN is important to improve their survival.
Recently,GN was also reported to have potential predictive value for CRN,especially for advanced CRN[11-15].However,some other studies demonstrated that colonoscopy surveillance is not recommended for all GN patients[16-18].Therefore,this study sought to investigate whether it is necessary for GN patients to receive colonoscopy.
MATERIALS AND METHODS
Study population and data collection
This current analysis was conducted by the PRISMA statement[19].
Search strategy
Two items including colonoscopy and GN were used for searching articles studying on the necessity of colonoscopy for GN patients.The text words of colonoscopy included colonoscopy,colonoscopies,and colonoscopic.The text words of GN included GC,gastric carcinoma,GNs,stomach cancer,stomach carcinoma,and stomach neoplasms.The search scope was limited to titles,abstracts,and author keywords.Only English was allowed.
Inclusion and exclusion criteria
The inclusion criteria were as follows: (1) Patients were divided into the GN group (gastric adenoma or cancer) and the control group;and (2) prevalence of CRN (colorectal adenoma,polyp or cancer) was reported.The exclusion criteria were as follows: (1) No comparison or insufficient data;and (2) the study types were conferences abstract,trail,review,metaanalysis,case report,letters to the editor,or comments.
Study selection
Eligible studies were searched in four databases including PubMed,EMBASE,the Cochrane Library,and Ovid.After conducting the search strategy,duplicates records were removed at first.Then,records in ineligible study types were excluded.Finally,full-texts were screened and studies were selected according to the inclusion and exclusion criteria.
Data collection
Baseline information of included studies and patients were collected for analysis.As for included studies,author,year,country,study date,study type,sample size,patients in the study group,evaluation of outcomes,conclusion,and the Newcastle-Ottawa Scales (NOS) score were collected.As for patients,age,sex,body mass index (BMI),diabetes,hypertension,alcohol,and smoking were collected.Moreover,for patients with CRNs,size,location,pathology,and number of CRN were also collected.Variables including age,male,BMI,smoking,drinking,and diabetes were collected to find whether there was a potential predictive value for CRNs in the whole patients and in the GN patients.
Quality Assessment
We used NOS score to assess the quality of included studies[20].All the studies were case-control studies,which were assessed in selection,comparability and exposure.Nine score was regarded as high-quality,eight or seven score was regarded as median-quality,and lower than seven score was regarded as low-quality.
Statistical analysis
Continuous variables were expressed as mean difference (MD) and standardized deviation (SD),and the relationship of categorical variables in two groups were expressed as odds ratios (ORs) and 95% confidence intervals (95%CIs).All the variables were pooled up for a pooling up analysis using the random-effects model and DerSimonian-Laird method.WhenP<0.1,the results was considered statistically significant.The chi-squared test and theI2value were used to evaluate the statistical heterogeneity[21,22].When theI²<30%,the statistical heterogeneity was considered nonimportant.When theI²=30%-60%,the statistical heterogeneity was considered moderate.When theI²>60%,the statistical heterogeneity was considered substantial.The funnel plot was used to evaluate the publication bias.STATA SE V16.0 software was used for data analysis.
RESULTS
Study selection
There were 871 studies after conducting the search strategy in four databases (223 studies in PubMed,527 studies in EMBASE,78 studies in the Cochrane Library,and 43 studies in Ovid).Duplicate records and records in ineligible study type were removed by Endnote software,and the left 63 records were ready for screening.Excluded for seven studies without unavailable full-text,56 studies were carefully selected by two authors according to the inclusion and exclusion criteria.Finally,this current analysis enrolled ten studies (Figure 1).
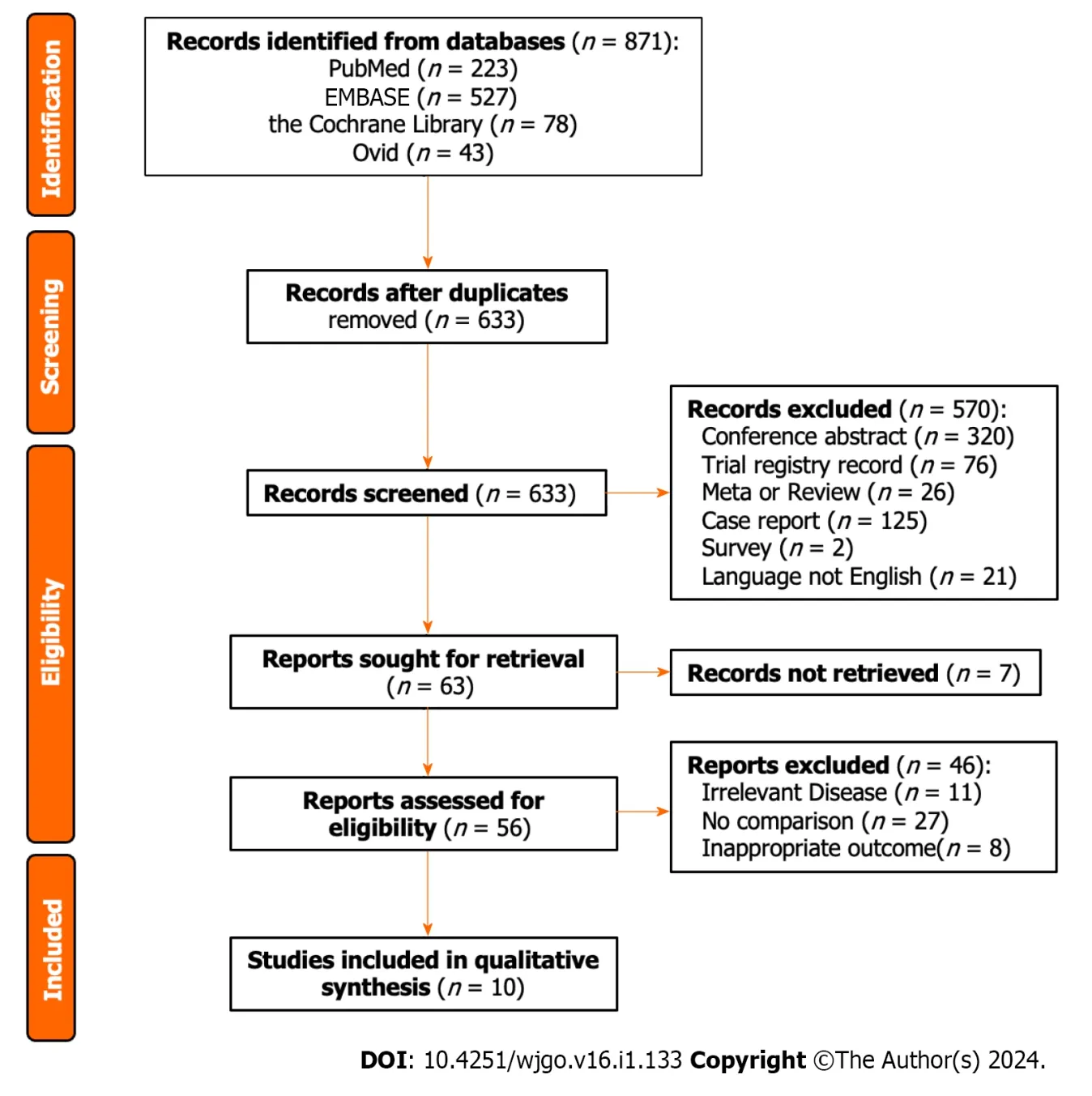
Figure 1 Flowchart of article selection.
Baseline information of included studies
Except for one study conducting in Japan,the other nine studies were conducted in Korea.The ten included studies were all case-control studies,and five were retrospectively conducted,the other five were prospectively conducted.As for patients in the case group,four studies reported GN,three studies reported GC,two studies reported early GC (EGC),and the other one reported early GN (EGN).After receiving colonoscopy,CRNs including colorectal adenoma,high-risk adenoma,cancerous adenoma,and CRC were reported.More information including author,year,study date,patients,conclusion,and the NOS score were shown in Table 1.
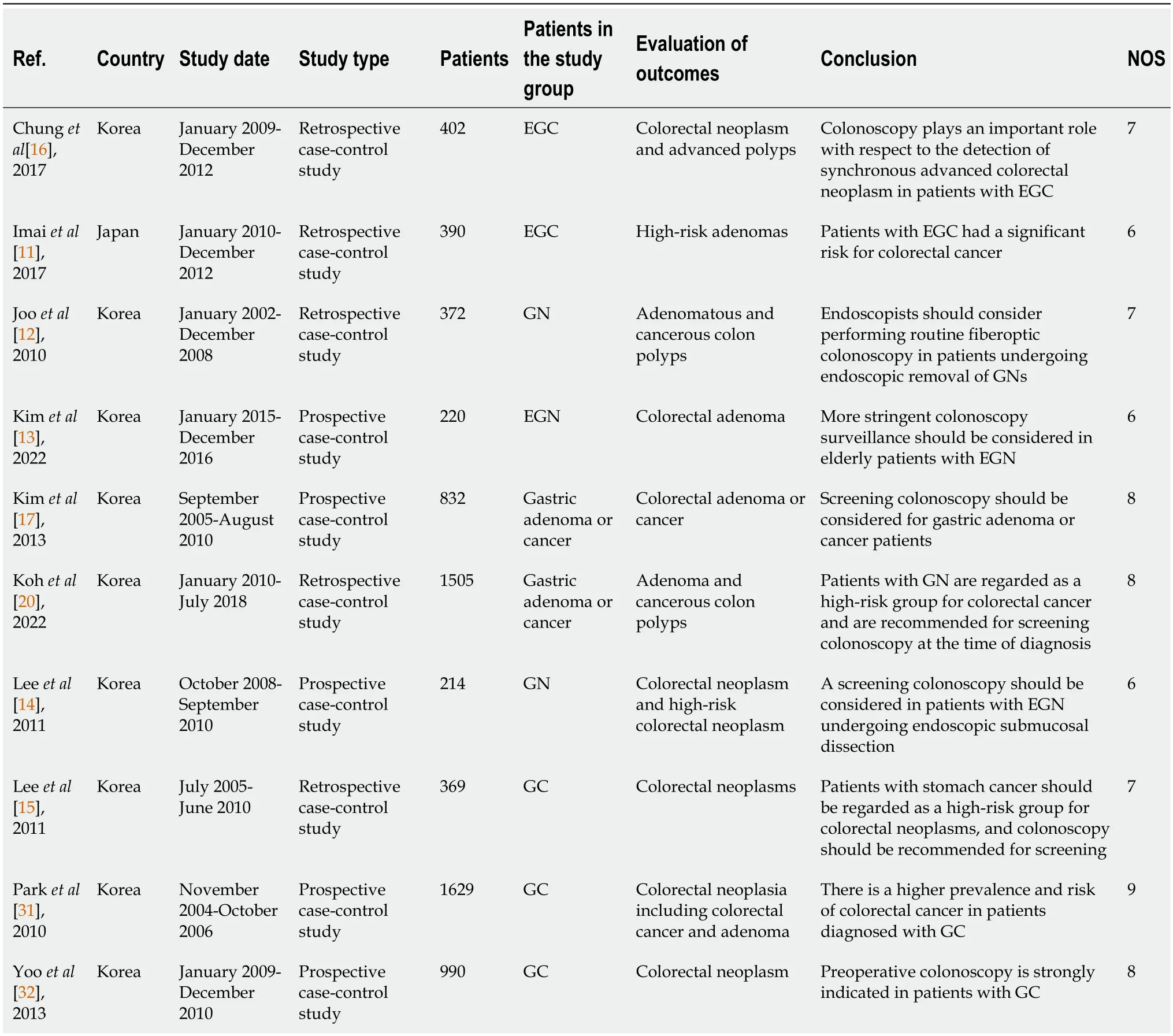
Table 1 Baseline characteristics of included studies
Baseline characteristics of the GN group and the control group
After comparing the baseline characteristics between the GN group and the control group,we found that patients with GNs had lower BMI (MD=-0.38,95%CI=-0.73 to -0.03,I2=8.00%,P=0.03).There was no significant difference in age,sex,diabetes,hypertension,alcohol,and smoking (P>0.1).As for patients who were detected to have CRNs in the two groups,there was no significant difference in size,location,pathology,and number >3 (P>0.1,Table 2).
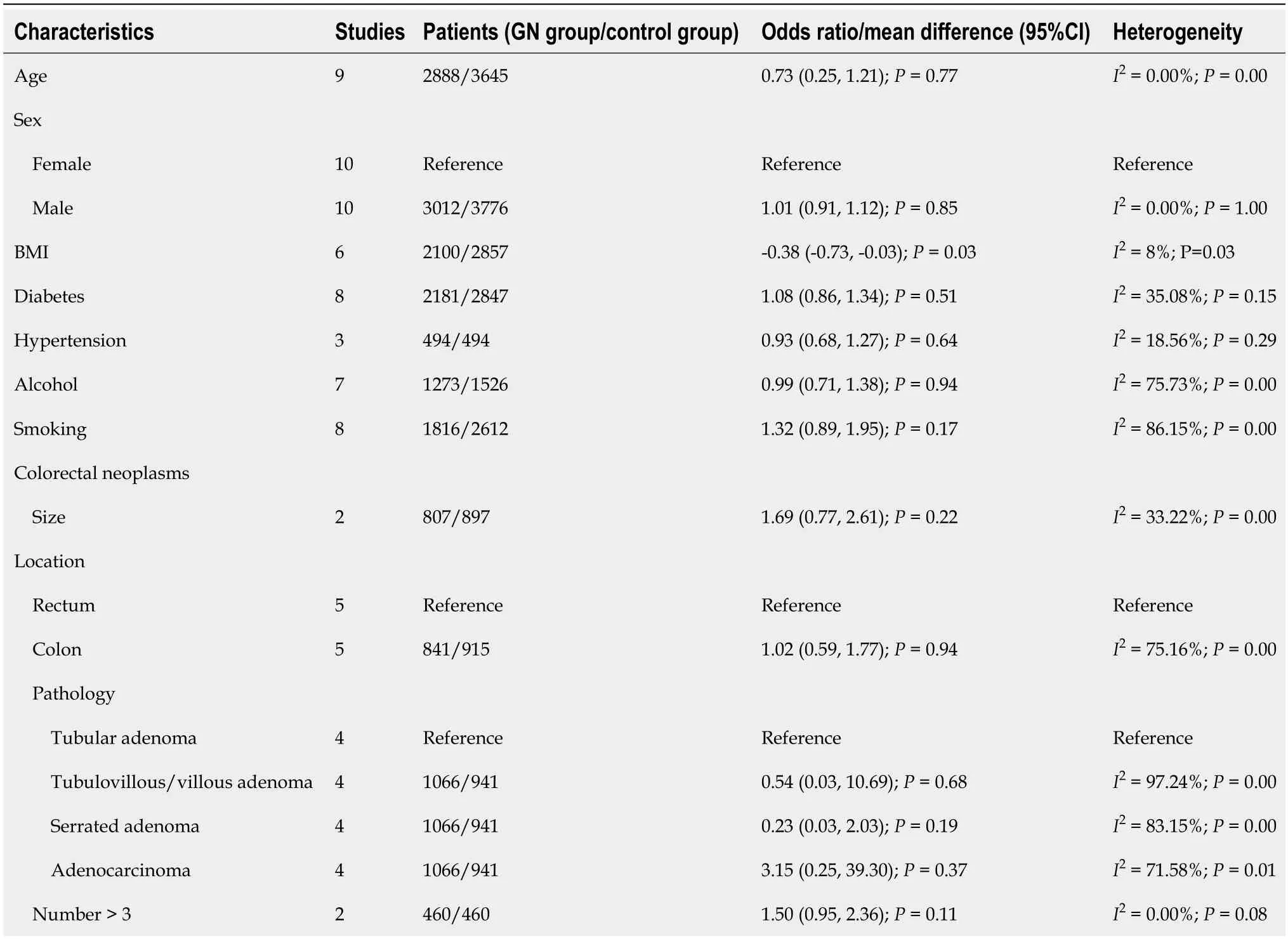
Table 2 Baseline characteristics of the gastric neoplasm group and the control group
Prevalence of CRN between the GN group and the control group
The prevalence of CRN was pooled,and it was found that the detection of CRN was significantly more in the GN group than the control group (OR=1.69,95%CI=1.28 to 2.23,I2=85.12%,P=0.00,Figure 2).
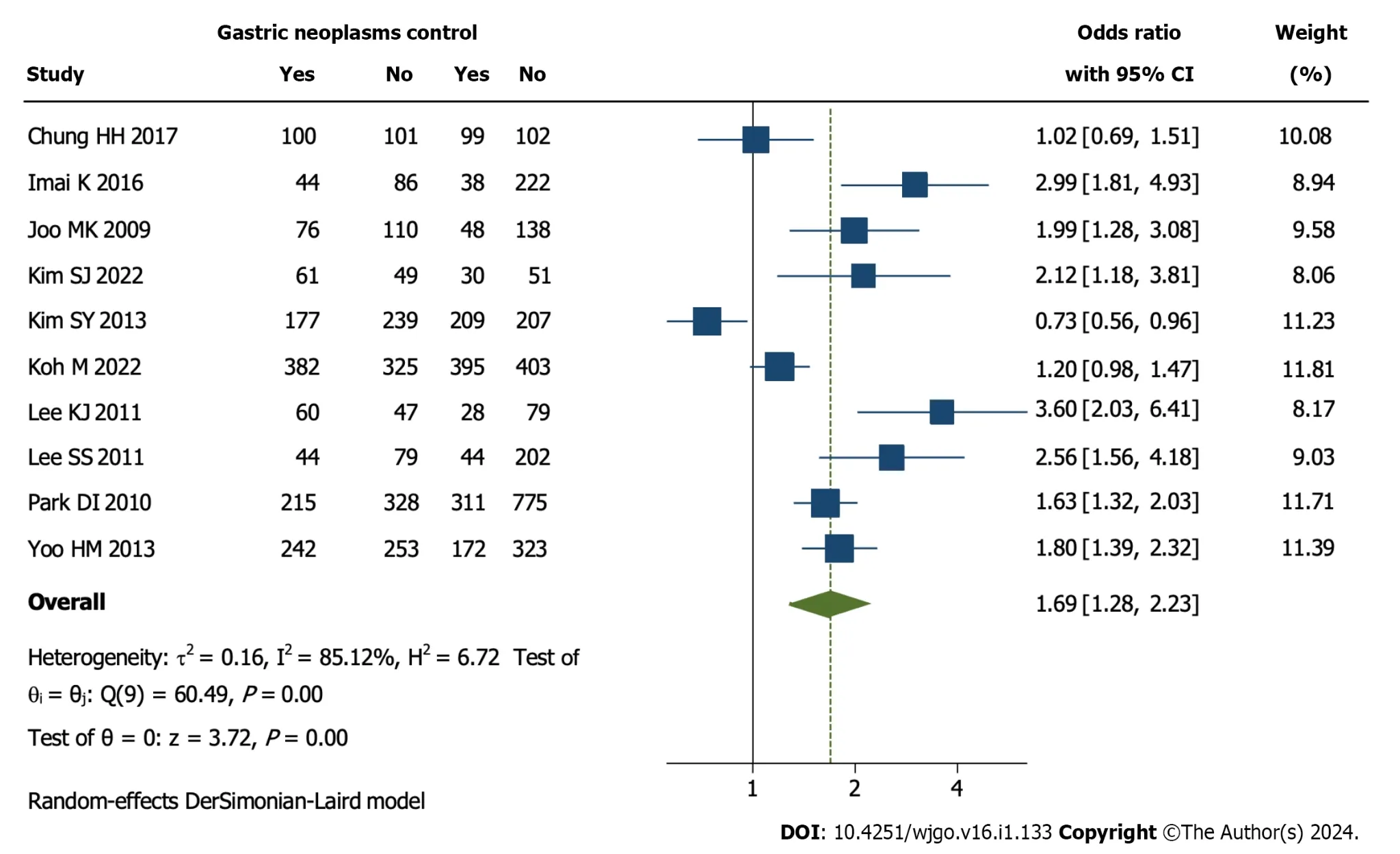
Figure 2 Prevalence of colorectal neoplasms in the gastric neoplasm group and the control group. 95%CI: 95% confidence interval.
Subgroup analysis based on different kinds of GNs
Subgroup analysis according to patients with different kinds of GNs was conducted.The results showed that GC patients (OR=1.80,95%CI=1.49 to 2.18,I2=25.55%,P<0.1) had a higher prevalence of CRN compared to patients with EGC (OR=1.73,95%CI=0.60 to 4.95,I2=90.92%,P>0.1) or EGN (OR=1.60,95%CI=0.99 to 2.23,I2=85.12%,P>0.1,Figure 3).

Figure 3 Subgroup analysis according to difference kinds of gastric neoplasms. 95%CI: 95% confidence interval.
Risk factors for CRN in the whole group (including control) and in the GN group
As for the whole patients included in this study,the analysis showed that age (OR=1.08,95%CI=1.00 to 1.17,I2=90.13%,P=0.00) and male (OR=2.31,95%CI=1.26 to 4.22,I2=87.35%,P=0.00) were independent risk factors for CRN.Other variables including BMI,smoking,drinking,and diabetes had no predictive value (P>0.1).As for patients in the GN group,the analysis showed that BMI (OR=0.88,95%CI=0.80 to 0.98,I2=0.00%,P=0.92) was a protective factor and smoking (OR=1.03,95%CI=1.01 to 1.05,I2=0.00%,P=0.57) was a risk factor for CRN.Other variables including age,male,and drinking had no predictive value (P>0.1,Table 3)
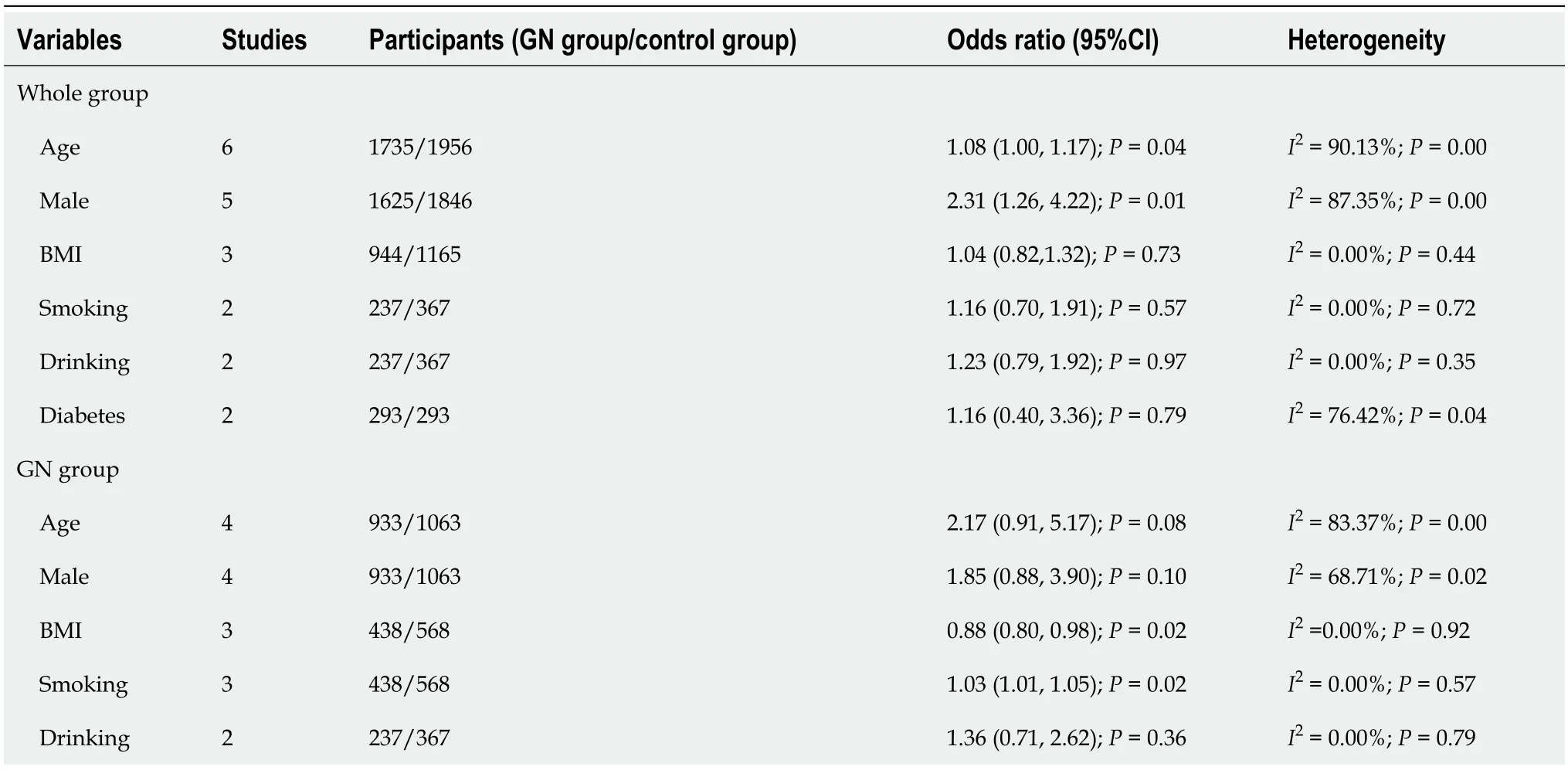
Table 3 Risk factors for colorectal neoplasms among the whole group (including control) and the GN group
Publication bias
The funnel plot was used for evaluating the publication bias.The plot was not relatively symmetrical,and four plots were outside the 95%CIs,which meant that the results were affected by some publication bias (Figure 4).

Figure 4 Funnel plot. 95%CI: 95% confidence interval.
Sensitivity analysis
This study evaluated the sensitivity by duplicate analysis of excluding each study at a time.The results of every time analysis were not significantly different,which meant that the results were relatively robust.
DISCUSSION
The current analysis included 6923 patients and found that GN patients had a higher risk of CRN,especially GC patients.Moreover,age and male sex were found to be independent risk factors for CRN in all patients,and BMI and smoking were protective and risk factors in GN patients,respectively.
Other primary neoplasms are common in GN patients,with the incidence ranging from 3.4% to 42.2%[23-26].CRN is the main neoplasm type of synchronous and homologous neoplasms[23,24].Although early CRN and EGN share many similarities,they have different tumor immune signatures and drug responses,which pose significant challenges for advanced CRN and GN[27-30].Early detection of neoplasms is obviously an important way to improve patient prognosis;therefore,regular medical checkups are needed for GN patients.
Several previous studies have revealed an association between GN and CRN.Imaiet al[11] reported that EGC is a risk factor for CRC.Others have demonstrated that GC patients are at high risk for not only CRC but also all CRN[15,31,32].Moreover,colonoscopy might be considered for patients with benign GN[12-14].However,both Chunget al[16] and Kohet al[18] revealed that the prevalence of CRN was not significantly different between patients with and without GN.Based on the above findings,our study was designed to address the current controversy and provide more valuable suggestions for GN patients.
In addition to GN,H.pyloriis thought to promote the development of CRN[33,34].H.pylorican not only increase the risk of GN and GC by damaging the mucosal barrier but also affect intestinal mucosa through the secretion of gastrin[35,36].Moreover,H.pylorican alter the immune signature by reducing T cells,pro-carcinogenic STAT3 signaling,and goblet cells,which have proinflammatory and degrading microbial effects,contributing to neoplasm development[37,38].Reducing the incidence of GN and CRN through eradication ofH.pylorihas been demonstrated in both mice and humans[37].
Another hypothesis is associated with genetic alteration and microsatellite instability[39,40].Mutations in the hMSH2 and hMLH1 genes,which mainly participate in repair of base-pair mismatches during DNA replication,play an important role in the occurrence of GN and CRN[39].In addition,the same K-ras,p53,andAPCgenes mutations are detected in both GN and CRN[40].These genetic correlations between CRN and GN support the higher risk of CRN in GN patients,as indicated in the current analysis.
This study addresses a current pressing question and provides reliable evidence for GN patients to receive regular colonoscopy.Since almost all the patients were Korean,the results are particularly applicable to Korea.Although there were important discoveries revealed by this study,there are some limitations.The results are limited in terms of region and ethnicity,and there is some publication bias.Therefore,more prospective case-control studies conducted worldwide are needed for further investigation.
CONCLUSION
Patients are recommended to receive colonoscopy when diagnosed with GN,especially those diagnosed with GC.
ARTICLE HIGHLIGHTS
Research background
Gastric cancer (GC) and colorectal cancer (CRC) are the fifth and third most common cancer worldwide,respectively.Nowadays,GC is reported to have a potential predictive value for CRC,especially for advanced CRC.
Research motivation
Colonoscopy is not commonly received by GC patients.Whether colonoscopy is necessary for GC patients is unclear.
Research objectives
The objectives of this study are patients diagnosed with gastric neoplasms (GNs).
Research methods
This study conducted a pooling-up analysis and subgroup analysis by STATA SE 16.0 software.
Research results
Colorectal neoplasm (CRN) was detected significantly more frequently in GN patients than controls.
Research conclusions
GC patients were suggested to receive colonoscopy before surgery.
Research perspectives
This study first systematically reviewed the prevalence of CRNs in patients with and without GNs.
ACKNOWLEDGEMENTS
We acknowledged to all the authors in this article,and we thank Xun Lei for the substantial work in the statistical methods.
FOOTNOTES
Co-first authors:Xu-Rui Liu and Ze-Lin Wen.
Author contributions:Peng D conceived,designed and refined the study protocol;Liu XR and Wen ZL were involved in the data collection;Liu XR and Wen ZL analyzed the data;Liu XR and Wen ZL drafted the manuscript;All authors were involved in the critical review of the results and have contributed to,read,and approved the final manuscript.Liu XR and Wen ZL contributed equally to this work as co-first authors.The reasons for designating Liu XR and Wen ZL as co-first authors are threefold.First,the research was performed as a collaborative effort,and the designation of co-first authorship accurately reflects the distribution of responsibilities and burdens associated with the time and effort required to complete the study and the resultant paper.This also ensures effective communication and management of post-submission matters,ultimately enhancing the paper's quality and reliability.Second,the overall research team encompassed authors with a variety of expertise and skills from different fields,and the designation of co-first authors best reflects this diversity.This also promotes the most comprehensive and in-depth examination of the research topic,ultimately enriching readers' understanding by offering various expert perspectives.Third,Liu XR and Wen ZL contributed efforts of equal substance throughout the research process.The choice of these researchers as co-first authors acknowledges and respects this equal contribution,while recognizing the spirit of teamwork and collaboration of this study.In summary,we believe that designating Liu XR and Wen ZL as co-first authors of is fitting for our manuscript as it accurately reflects our team's collaborative spirit,equal contributions,and diversity.
Supported byCQMU Program for Youth Innovation in Future Medicine,No.W0190.
Institutional review board statement:The data used in this study were obtained from public databases.No Institutional Review board Approval were needed.
Informed consent statement:The data was accessed in the database and all patients sighed informed consent.
Conflict-of-interest statement:The authors declare that there are no conflicts of interests.
Data sharing statement:The data was accessed in the database.
STROBE statement:The authors have read the STROBE Statement—checklist of items,and the manuscript was prepared and revised according to the STROBE Statement—checklist of items.
Open-Access:This article is an open-access article that was selected by an in-house editor and fully peer-reviewed by external reviewers.It is distributed in accordance with the Creative Commons Attribution NonCommercial (CC BY-NC 4.0) license,which permits others to distribute,remix,adapt,build upon this work non-commercially,and license their derivative works on different terms,provided the original work is properly cited and the use is non-commercial.See: https://creativecommons.org/Licenses/by-nc/4.0/
Country/Territory of origin:China
ORCID number:Xu-Rui Liu 0000-0002-6069-2104;Fei Liu 0000-0002-4022-0732;Zi-Wei Li 0000-0001-9759-4535;Xiao-Yu Liu 0000-0001-9448-4592;Wei Zhang 0000-0002-5822-9970;Dong Peng 0000-0003-4050-4337.
S-Editor:Lin C
L-Editor:A
P-Editor:Zhang XD
杂志排行
World Journal of Gastrointestinal Oncology的其它文章
- Comprehensive analysis of the role of ubiquitin-specific peptidases in colorectal cancer: A systematic review
- Prognostic significance and relationship of SMAD3 phosphoisoforms and VEGFR-1 in gastric cancer: A clinicopathological study
- Analysis of the potential biological value of pyruvate dehydrogenase E1 subunit β in human cancer
- Colorectal cancer’s burden attributable to a diet high in processed meat in the Belt and Road Initiative countries
- Emerging role of liquid biopsy in rat sarcoma virus mutated metastatic colorectal cancer: A case report
- Comprehensive evaluation of rare case: From diagnosis to treatment of a sigmoid Schwannoma: A case report
