New trends in diagnosis and management of gallbladder carcinoma
2024-01-26EfstathiosPavlidisIoannisGalanisTheodorosPavlidis
Efstathios T Pavlidis,Ioannis N Galanis,Theodoros E Pavlidis
Abstract Gallbladder (GB) carcinoma,although relatively rare,is the most common biliary tree cholangiocarcinoma with aggressiveness and poor prognosis.It is closely associated with cholelithiasis and long-standing large (>3 cm) gallstones in up to 90% of cases.The other main predisposing factors for GB carcinoma include molecular factors such as mutated genes,GB wall calcification (porcelain) or mainly mucosal microcalcifications,and GB polyps ≥ 1 cm in size.Diagnosis is made by ultrasound,computed tomography (CT),and,more precisely,magnetic resonance imaging (MRI).Preoperative staging is of great importance in decisionmaking regarding therapeutic management.Preoperative staging is based on MRI findings,the leading technique for liver metastasis imaging,enhanced three-phase CT angiography,or magnetic resonance angiography for major vessel assessment.It is also necessary to use positron emission tomography (PET)-CT or 18F-FDG PET-MRI to more accurately detect metastases and any other occult deposits with active metabolic uptake.Staging laparoscopy may detect dissemination not otherwise found in 20%-28.6% of cases.Multimodality treatment is needed,including surgical resection,targeted therapy by biological agents according to molecular testing gene mapping,chemotherapy,radiation therapy,and immunotherapy.It is of great importance to understand the updated guidelines and current treatment options.The extent of surgical intervention depends on the disease stage,ranging from simple cholecystectomy (T1a) to extended resections and including extended cholecystectomy (T1b),with wide lymph node resection in every case or IV-V segmentectomy (T2),hepatic trisegmentectomy or major hepatectomy accompanied by hepaticojejunostomy Roux-Y,and adjacent organ resection if necessary (T3).Laparoscopic or robotic surgery shows fewer postoperative complications and equivalent oncological outcomes when compared to open surgery,but much attention must be paid to avoiding injuries.In addition to surgery,novel targeted treatment along with immunotherapy and recent improvements in radiotherapy and chemotherapy (neoadjuvant-adjuvant capecitabine,cisplatin,gemcitabine) have yielded promising results even in inoperable cases calling for palliation (T4).Thus,individualized treatment must be applied.
Key Words: Biliary tract neoplasms;Extrahepatic cholangiocarcinoma;Gallbladder carcinoma;Gallbladder diseases;Biliary tree diseases;Gastrointestinal malignancies
INTRODUCTION
Gallbladder (GB) carcinoma,although relatively uncommon,is the most common biliary tree cholangiocarcinoma and constitutes an aggressive,lethal malignancy with a dismal prognosis[1-5].It is the 6thmost common gastrointestinal tract carcinoma and is more common in women.Although 5-year survival has progressively increased to between 7% and 20%,patients with advanced disease still have a lower than 5% 5-year survival[1,4,6-8].
Gene mutations,socioeconomic status and environmental factors may explain the differences in geographical incidence distribution[9-11].The global incidence is 1.2 cases per 100000 inhabitants,with the highest rates in Asia,mainly China and India (1.4 cases per 100000 inhabitants),and the lowest rates in Europe (0.66 cases per 100000 inhabitants) and North America (0.67 cases per 100000 inhabitants).However,with an increased aging population and obesity,a substantial increase in GB carcinoma rates is estimated to occur by 2040[1].
GB carcinoma is closely associated with cholelithiasis and long-standing (>20 years) large (>3 cm) gallstones[12] in up to 90% of cases[9,13-15].In approximately half of all cases,GB carcinoma is revealed in cholecystectomy specimens,and its incidence among specimens fluctuates between 0.19% and 1.6%[9,16,17].In addition,because of its cooccurrence with cholelithiasis,it is associated with female sex,obesity,and increased age[9,18].Gallstones are the main cause of GB mucosa inflammation and secondary infection byHelicobacter pylorior Salmonella.This chronic inflammation induces mediator release,which in the long term may cause gene alterations,ultimately leading to carcinogenesis[15] through previous mucosal damage,metaplasia and dysplasia[12].Among other notable predisposing factors for GB carcinogenesis are mutated genes,mainlyTP53(up to 91%) andKRAS(29.0%)[15,19,20],GB wall calcification (porcelain GB) or mainly mucosal microcalcifications,GB neoplastic true polyps ≥ 1 cm in size[12,16] and aflatoxin[21] or the older contrast medium Thorotrast[10].
GB carcinoma arising from the epithelium is typically adenocarcinoma (95.7%) but can also infrequently be squamous carcinoma (2.4%) or adenosquamous carcinoma (1.9%),both with more aggressiveness and worse prognoses than adenocarcinoma[12,22-24].
There are two precancerous lesions of GB adenocarcinoma: (1) Intracholecystic papillary-tubular neoplasm;and (2) biliary intraepithelial neoplasia.The malignant transformation of these precursors has a better prognosis than the original carcinoma.Multivariate analysis showed that the absence of coexistence with such lesions in adenocarcinoma was associated with symptomatic cases and advanced stage at presentation,poor cancer cell differentiation,and poor prognosis[25].
Mucinous adenocarcinoma is a rare subtype of GB adenocarcinoma with more aggressiveness,but it has the same management[26].
Diagnosis is made by ultrasound (US),computed tomography (CT)[27],and,more precisely,magnetic resonance imaging (MRI) by detecting a filling defect in the GB or wall thickening and assessing the depth of invasion[7,12].Preoperative staging is of great importance in the decision-making plan of therapeutic management.Preoperative staging is based on MRI contrast-enhanced findings,the leading technique for liver metastasis imaging[28],enhanced three-phase CT angiography or magnetic resonance angiography for major vessel assessment.It is also necessary to use18F-FDG positron emission tomography (PET)-CT[29,30] or18F-FDG PET-MRI[28] to more accurately detect metastases and any other occult deposits with active metabolic uptake.PET is complementary to traditional imaging for primary lesions and imperative for doubtful metastases with high specificity,including follow-up[31].Staging laparoscopy may detect dissemination that cannot otherwise be found preoperatively in 20%-28.6% of cases;thus,it must be included in evaluation planning[32,33].
A prediction model of prognosis that is based on multiple clinical indications,in combination with artificial intelligence algorithms,has been recently developed[34].
Surgical curative resection is the cornerstone of treatment but is often impossible in advanced metastatic disease.Its extent depends on staging ranging from cholecystectomy to major resections with wide lymphadenectomy[3,29,35-37].However,a debate exists about extended operations,which increase morbidity and mortality with unclear long-term outcomes[3].
Laparoscopic or robotic surgery has the advantages of minimally invasive surgery and equivalent long-term outcomes to open surgery but requires much attention and expertise to avoid major complications[38-40].
Other management options include chemotherapy and radiotherapy,immunotherapy,and targeted therapy by monoclonal antibody biological agents[41-45].The current rapidly evolving,multimodal therapeutic approach[46] and Medicaid expansion[47] have improved the results,opening new perspectives even in inoperable cases involving palliative treatment[4,13,48-50].
Nanotechnology using photodynamic nanoparticles to target the tumor has been reported recently as a novel treatment[51].
In this narrative review,we evaluate the updated knowledge on GB carcinoma,emphasizing current diagnosis and surgical management.This study was based on an extensive literature review from PubMed until October 2023,focusing particularly on full-text papers published only in the English language over the last six years.
DIAGNOSIS
The diagnostic steps are shown schematically in Figure 1.
Clinical presentation
Unfortunately,GB carcinoma is usually asymptomatic in the early stages,or the symptoms of coexisting cholelithiasis predominate,and GB carcinomas may be detected incidentally by histopathological examination of the cholecystectomy specimen or by imaging performed for other reasons.The appearance of pain,mainly obstructive jaundice,anorexia,weakness,and weight loss,indicate a more advanced disease[12].
The presence of preoperative obstructive jaundice may be considered a contraindication for curative resection because it is accompanied by increased morbidity and mortality and worse overall survival;obviously,a careful high selection of jaundiced patients is mandatory[35,52].
GB carcinomas are located in the GB fundus (60%),body (30%) and/or neck (10%).On imaging,it can be found as an intraluminal mass or occupying the GB along with focal or diffuse wall thickening[12].
US plain,contrast-enhanced US,high-frequency US,high-resolution US,and endoscopic US in combination with threephase contrast-enhanced multidetector CT[53] and contrast-enhanced MRI constitute the basic steps for diagnosis and preoperative staging[7,12,27,28].
18F-FDG PET-CT[54,55] or18F-FDG PET-MRI[28] must be performed before every intended major curative resection to exclude any occult metastatic lesion,which is not visible by the other imaging techniques,particularly in port-site metastases after laparoscopic cholecystectomy[29] and in ambiguous cases or at follow-up[12,31,56].
Artificial intelligence may analyze computerized imaging.Radiomics is a sophisticated method of imaging analysis machine learning that ensures,on the one hand,precise diagnosis and staging,including lymph node involvement and depth of wall invasion,particularly serosal infiltration,and,on the other hand,reliable prognosis predicting oncological outcomes,including survival and recurrence[27].
Endoscopy
In addition to magnetic resonance cholangiopancreatography and percutaneous transhepatic cholangiography,endoscopic retrograde cholangiopancreatography (ERCP) and cholangioscopy may be used to evaluate the common bile duct in the presence of obstructive jaundice.ERCP may also provide bile samples or brushings for cytological examination in doubtful cases[13,42,57].
Endoscopic ultrasound (EUS) provides high-quality images.In addition,EUS-guided fine needle aspiration biopsy may be used to safely diagnose GB malignancy in suspected cases but has the drawback of bile leakage and potent intraperitoneal dissemination of cancer cells[58].Additionally,imaging-guided fine needle aspiration cytology of GB bile is sometimes used[22].
Transpapillary GB biopsy by insertion of a novel cholangioscopeviathe cystic duct may overcome these disadvantages and has been recently introduced[57,59].
Tumor markers
The tumor markers CA 19-9,CA 125,CA 242,CA 15-3,and CEA have been found to be elevated in GB carcinoma and could contribute to its early diagnosis and in the follow-up for prompt detection of recurrence[12,16].
The preoperative value of CA 125 was found to be an independent risk factor for early recurrence[60].CA 19-9 is valuable for detecting recurrence,with a sensitivity of 79.1%,specificity of 97.2%,positive predictive value of 95%,and negative predictive value of 87.5%[61].
Circulating tumor cell assessment is feasible and constitutes a determinant factor of the management plan and preoperative prognostic marker[62].
To date,there is no indication for including gut microbiota assessment in the diagnosis and management of GB carcinoma[63].
Molecular factors, genes and other molecules
Knowledge of molecular mechanisms is valuable for aiding in the development of novel therapeutic targets.Heet al[64] recently demonstrated that zinc finger protein 64 (ZFP64) plays an important role in GB carcinogenesis and progression through the ZFP64-Notch1-HDAC1 pathway.It promotesin vitroandin vivocell proliferation,anti-apoptosis,migration,and invasion[64].Thus,targeting this protein may be the basis for a prospective efficient treatment.
Topological alterations in genomic structure lead to genomic dysfunction that promotes malignant transformation[65].Genomic analysis may be useful as a diagnostic biomarker or,most importantly,for potent targeted therapy.Genes of interest includeVEGF,VEGFR,EGFR,MEK1,MEK2,MET,mTOR,HER2,N-cadherin,PI3K,PDL-1andPD-1[15].
Zhouet al[23] recently reported the genetic characteristics of GB carcinoma in elderly individuals over 65 years.They found increased expression of the cell cycle-related genesAURKA,AURKB,CCNA2,CCNB1,CDK1,DLGAP5,KIF11,MELK,NCAPG,andTPX2and decreased expression of the mitochondrial function-associated genesND1,ND2,ND3,ND4,ND4L,CYTB,COX1,COX2,ATP6,andATP8.These genes promote cancer cell overgrowth and metastasis.In addition,Zhouet al[23] found that elderly patients were less responsive to gemcitabine and cisplatin chemotherapy,similar to immunotherapy,with high PD-L1 and CTLA-4 expression[23].
Mishraet al[19] studied 37 formalin-fixed GB carcinoma paraffin-embedded cubes of specimens and found that the most common mutations occur in combination inTP53(90.9%),SMAD4(60.6%),NOTCH1(45.45),ERBB2(45.45%),PIK3CA(33.33%),MET(30.30%),PTEN(30.3%),EGFR(24.24%),KRAS(21.21%) andBRAF(9%).Mutations that could be targeted constituted 89.91% of cases and included all the above genes,except theTP53gene.CTNNB1,KRASandNRASgene mutations were more highly related to metastatic disease[19].
Chaeet al[20] conducted a study of 124 patients in Korea and found that 83.8% of patient samples contained genetic alterations,and the most common mutations were inTP53(44.4%),KRAS(29.0%),ERBB2-3(20.0%),ARID1A(12.1%),andIDH1(4%)[20].
Expression of theHer2/neugene,a receptor of tyrosine kinase 2,is found,apart from breast carcinoma,in GB carcinoma and is associated with the degree of cell differentiation and advanced stage (III,IV).It could be used for prognosis and in follow-up[66].HER2/ERBB2gene overexpression has been found in 20% of advanced GB carcinoma stages and may be a target of relevant treatment[67].
A study of 157 GB carcinoma patients in China found that mutatedERBB2/ERBB3genes (7%-8%) promoted proliferation and migration,upregulated PD-L1 expression,and were associated with a worse prognosis.These mutations may be useful biomarkers for targeted therapy[68].
The expression of theFASNgene (fatty acid synthase),a key enzyme of lipid metabolism that has great importance in cancer progression through the PI3K/AKT pathway,was found to promote GB carcinoma growth and is related to a decreased response to gemcitabine chemotherapy[69].
The expression ofthe EMP3gene was decreased in GB carcinoma and was related to poor prognosis.Its therapeutic targeting may inhibit carcinoma progression through the miR-663a/EMP3/MAPK/ERK pathway[70].
The expression ofthe YTHDF2gene promoted GB carcinoma cell proliferation,growth,migration,and invasion and inhibited apoptosisin vitroandin vivo.Additionally,it was related to a decreased response to gemcitabine treatment and may be a therapeutic target[71].
The expression of theFOXA2suppressive gene is poor in GB carcinoma[72].
The expression of them6Agene,which modifiesCLDN4gene stability,induces immunosuppression and poor prognosis in GB carcinoma due to an aggressive phenotype;thus,it may be a therapeutic target[73].
TheCEP55gene was overexpressed in GB carcinoma and associated with a decrease in apoptosis,advanced stage,lower cell differentiation,and dismal prognosis.Thus,it constitutes not only a diagnostic and prognostic biomarker but also a potent prospective therapeutic target[74].
It has been found thatDLGAP5gene expression was increased in GB cancer and associated with poor prognosis by promoting proliferation and migration;it could be a therapeutic target[75].
The mutatedPBRM1gene has been found in a small proportion of GB carcinomas related to DNA damage repair.It could be amenable to targeted therapy[76].
It has been found that the mutatedTRIM37gene was increased in GB carcinoma,promoting progression by increased proliferation and decreased apoptosis.It was related to lower cell differentiation,advanced stage,and reduced survival;it could be a therapeutic target[77].
A recent study of 148 GB carcinoma patients in Korea performed multivariate analysis and found thatPAK4gene expression and the associatedPHF8gene were independent predictive factors of reduced survival and dismal prognosis[78].
miRNAs may be valuable biomarkers and therapeutic targets[6,15].The most dysregulated miRNAs in GB carcinoma were the upregulated miRNAs miR-4430 and miR-642α-3p and the downregulated miRNAs miR-451α and miR-145-5p.miR-642α-3p and miR-145-5p were associated with invasion and metastasis and could constitute a prospective therapeutic target[79].miR-214-3p,which is expressed in mesenchymal stem cells of the umbilical cord,may decrease proliferation and increase apoptosis of GB carcinoma by inhibitingACLY/GLUT1gene expression[80].
Histopathological staging
Histopathological staging is based on the TNM system (primary tumor invasion,lymph node involvement,and distant metastases).The applicable 8thEdition of TNM classification and staging by the American Joint Committee on Cancer (AJCC),which entered into force on January 1,2018,replacing the 7thEdition,are shown in Tables 1 and 2[81].Jianget al[81] proposed a small modification of this staging system in 2020 to improve its diagnostic accuracy,but the AJCC has not made any change thus far[81].
MANAGEMENT
Surgery remains the first-choice basic treatment for long-sustained oncological outcomes even in elderly patients (70-84 years)[82],but unfortunately,the disease is usually inoperable at presentation.Curative resection may be performed in only 15%-35% of cases and is associated with high recurrence.Thus,multimodal management is imperative,and the current efforts have been focused in this direction[46,47,83].
Precise and evidence-based decisions must be made to determine the best management strategy.The optimal extent of surgical resection and the appropriate adjuvant treatment should be individualized based on the patient’s physical status,comorbidity,imaging staging and molecular genetic factors[41,83,84].
Surgery
Therapeutic radical operative resection is the cornerstone of management.The extent of resection depends on the T classification stage of tumor invasion[85-88].For Tis and T1a,simple cholecystectomy is an adequate treatment.For T1b and T2a,extended cholecystectomy with removal of the GB bed or segment IVb and V resection (T2b) and regional lymphadenectomy have gained wide acceptance[37,85-87,89].For T3,major hepatectomy (trisegmentectomy or right hepatectomy),extended lymphadenectomy,and common bile duct resection with hepaticojejunostomy or hepatopancreato-duodenectomy in more advanced cases can be performed[85,86,90].For inoperable stage T4,palliative systematic treatment (chemoradiation,immunotherapy,targeted therapy) is recommended[46].The management policy according to T stage is shown schematically in Figure 2[46,85,86].Extended cholecystectomy in the T1b stage was related to better survival than simple cholecystectomy,particularly in elderly patients (≥ 67 years)[91].
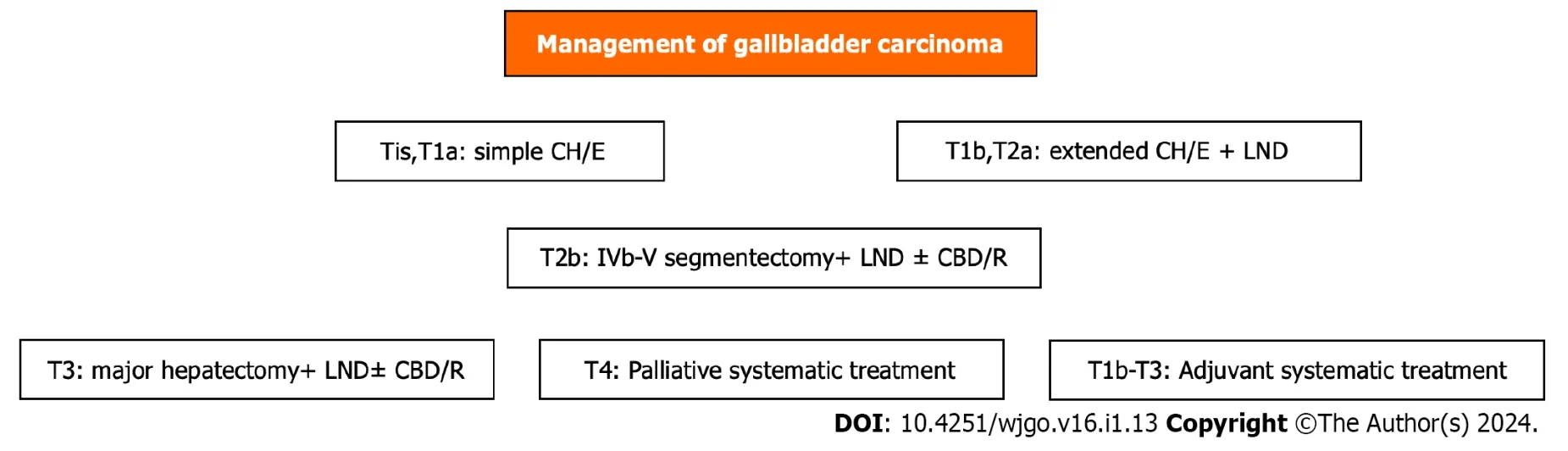
Figure 2 Scheme of gallbladder carcinoma management. CBD/R: Common bile duct resection;CH/E: Cholecystectomy;LND: Lymphadenectomy.
A recent study in China of 144 patients with T2-T4 stage advanced GB carcinoma determined that the total number of removed lymph nodes must be at least 6,and the optimal lymph node ratio (positive to total) is 0.28.Lymphadenectomy may be D1 (lymph nodes of hepatoduodenal ligament and common hepatic artery) or D2 (lymph nodes of posterior duodenum and celiac artery)[85].Adequate lymphadenectomy has an increasing trend in the United States and Japan,affecting survival[92-94].Extrahepatic bile duct resection was performed only in jaundiced patients and cystic duct invasion[85,95].Resection of adjacent organs and portal vein or hepatic artery reconstruction was possible if there was related infiltration.Multivariate analysis identified T stage,R (residual) resection and G (grade) of cell differentiation as independent prognostic factors[85].
The method of lymphadenectomy influences the outcome.Another study in China of 133 patients found that fusion lymphadenectomy,which uses 3D-SPECT (photon emission CT) and CT or MRI data,may increase the number of both overall retrieved lymph nodes and positive lymph nodes.It improved both the diagnostic accuracy and survival[96].A study of 227 GB carcinoma patients assessed the effect of three-dimensional visualization preoperative evaluation and enhanced recovery after surgery and found that precise surgery improved oncological outcomes.The researchers found that this effect,compared to the control group,showed a higher R0 resection rate (67.4%vs20.9%) and number of retrieved lymph nodes (26.6 ± 12.6vs16.3 ± 7.6%) and better median overall survival (27.4 movs12.7%),1-year survival (84.4%vs53.5%) and 3-year survival (29.8%vs15.1%)[97].
A recent large national cohort study in Japan of 4917 GB carcinoma patients,including 1609 T2 stage patients,evaluated the efficacy of extrahepatic bile duct resection in this stage compared to nonresection.They found that resection was associated with higher lymph node involvement (38.2%vs20.7%),postoperative complications (32.4%vs11.7%),and 5-year survival (64%vs54%) but comparable disease-specific survival (76%vs79%);they recommended much caution in decision-making for such resection in the T2 stage[98].A recent systematic review and meta-analysis including 2086patients and 9 studies with T2 stage GB carcinoma who underwent wedge hepatectomy (extended cholecystectomy) or hepatic segment IV and V resection found that segment resection provided better disease-free survival than wedge resection but more postoperative complications[99].Another recent meta-analysis including 7 studies and 1795 GB carcinoma patients with stage T2 and T3 disease found that extended cholecystectomy had better short-term outcomes than hepatic segment IV and V resection and equivalent oncological outcomes[100].Wuet al[90] demonstrated that extended lymphadenectomy provided a significant survival benefit in patients with preoperative N0 stage disease[90].A recent study of 197 stage T2 GB carcinoma patients found that liver resection added to lymphadenectomy did not improve survival compared to lymphadenectomy alone,while it involved more blood loss and hospitalization.The 5-year disease-free survival was equivalent (82.7%vs77.9%) in both T2a and T2b stages.A multivariate analysis showed lymph node involvement and perineural invasion,but not the absence of liver resection,as risk factors for worse survival outcomes.The researchers recommended T2 stage extended cholecystectomy with lymphadenectomy,without hepatic segment IV and V resection in selected cases[101].Perineural invasion has been considered an important indicator of early recurrence and worse prognosis.In such cases,adjuvant chemotherapy has been associated with improvement in survival[102].

Table 1 T classification in TNM system for gallbladder adenocarcinoma of AJCC 8th edition
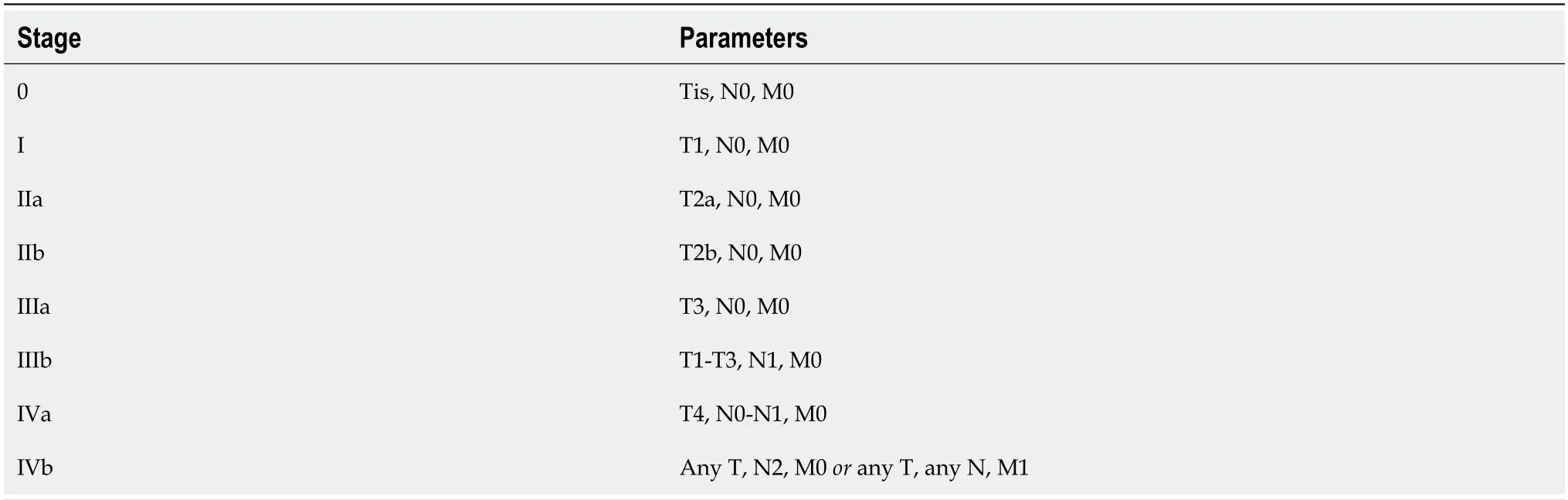
Table 2 TNM staging for gallbladder adenocarcinoma of American Joint Committee on Cancer 8th edition
The importance of GB carcinoma location has been evaluated.Proximal tumors (neck and cystic duct) are less common,more frequently associated with obstructive jaundice,and had more aggressiveness with worse prognosis compared to distal tumors (body and fundus)[103].Cystic duct location was an independent prognostic risk factor that did not have any survival benefit by common bile duct resection.Likewise,the latter also applies to distal locations,where extrahepatic bile resection may even be harmful[104].A systematic review and meta-analysis confirmed increased morbidity,particularly in patients without jaundice[95].
For incidentally discovered GB carcinoma (stage ≥ Ib) after cholecystectomy,there have been different conflicting aspects about the optimal extent following surgical resection of the liver GB bed (≥ 2 cm wedge excision).A recent study of 111 patients found that there were no significant differences in overall survival after R0 resection independent of precise excised hepatic volume.However,a volume ≥ 105 cm3was associated with increased morbidity.Thus,for ≥ T3 stage,the authors recommended a volume of 77.5 cm3-105 cm3,but some concerns have been raised regarding overall survival[105].
A recent study conducted in the United States including 791 GB carcinoma patients incidentally discovered after cholecystectomy stage T1b-T3 evaluated the optimal reresection time.The researchers found that the optimal reoperation time for improved overall survival was over 4 wk after initial surgery,but there were no significant differences when surgery was performed at 5-8 wk,8-12 wk or more[106].
Hepatectomy for countable,treatable metastatic liver disease with increased CA 19-9 values after initial curative surgery for GB carcinoma has been described,but with high recurrence,mainly within the following 6 mo[107].
A recent large multicenter,retrospective,international study (Omega) including 3676 patients showed that hepatectomy did not improve survival,and extended operations increased morbidity and mortality without oncological benefit[3].Likewise,Creasyet al[108] reported that there was a trend in the United States to perform fewer biliary and major liver resections[108].Choet al[109] reported that liver resection is not essential for curative treatment in the T2b stage[109].
Therapeutic excision has been recently proposed in selected cases for stage IV GB carcinoma,but with limited metastases.A study conducted in India of 1040 GB carcinoma patients,234 of which were stage IV with low volume metastases (among them,62 patients underwent R0 resection and adjuvant systemic therapy) found that patients in the operation group had better median overall survival (19 movs12 mo) compared to those receiving only palliative chemotherapy[8].
The repeated surgical resection for GB carcinoma,as for intrahepatic cholangiocarcinoma,has recently gained attention,and Laurenziet al[4] reported good outcomes[4].Xieet al[110] found that the excision of primary tumors in metastatic advanced GB carcinoma may improve survival[110].Chanet al[111] proposed frozen sections in suspected cases of GB carcinoma to confirm the diagnosis[111].
Textbook outcomes in liver surgery (TOLS) is a new assessment method designed by experts to evaluate the optimal course after liver excision.A multicenter study conducted in China including 11 tertiary hospitals and 242 patients found that TOLS was achieved in almost half of GB carcinoma patients who were treated by pressurized therapeutic excision.A multivariate analysis determined the following as independent prognostic factors for optimal outcome: Age ≤ 70 years;preoperative bilirubin ≤ 3 mg/dL;T1 stage;N0 stage;extended cholecystectomy;and no need for neoadjuvant therapy.Subsequently,a relevant accurate prediction nomogram by logistic regression analysis has been proposed[112].
High-quality surgery is essential in the management of GB carcinoma.An international multicenter study including 13 high-volume centers and 906 GB carcinoma patients with indented therapeutic surgery assessed the outcomes.Among them,245 operations (27%) fulfilled the evaluation criteria,which included the following benchmark values: (1) Retrieved lymph nodes ≥ 4;(2) blood loss ≤ 350 mL;(3) blood transfusion ≤ 13%;(4) duration of operation ≤ 322 min;(5) hospitalization ≤ 8 d;(6) R1 resection (margin macroscopic infiltration) ≤ 7%;(7) overall complications ≤ 22%;and (8) complications of grade ≥ 3 at a rate of ≤ 11%[113].
Minimally invasive surgery
Laparoscopic hepatic bisegmentectomy (segment IVb and V) and lymph node dissection for T1b or T2a are feasible,safe and effective with better short-term outcomes than open procedures and equivalent long-term outcomes[114].Equivalent short-term and long-term oncological outcomes were exhibited by laparoscopic and open surgery for T3 stage incidentally discovered GB carcinoma[40].
However,a debate still exists between laparoscopic and open procedures.According to applicable guidelines of the National Comprehensive Cancer Network,the European Society of Medical Oncology,the Japanese Society of Hepato-Biliary-Pancreatic Surgery,and the Chinese Surgical Society and Chinese Committee of Biliary Surgeons,open surgery is recommended as a rule and laparoscopic surgery only in selected cases and for research purposes[115-118].This recommendation has been based on the fears and reservations regarding intraperitoneal cancer cell dissemination in cases of GB perforation and bile spillage,as well as the doubtful achievement of laparoscopic radicality and adequate lymphadenectomy mainly around the hepatoduodenal ligament and hepatic artery[39,86,119-121].However,despite these uncertainties,by improving equipment and operative skills,advances in laparoscopic techniques[122-126] or even robotic management[38,127] can overcome the disadvantages and difficulties of laparoscopic procedures.The subject remains amenable to further evaluation and possible revision of the guidelines.A recent study conducted in Korea of 125 patients who underwent extended cholecystectomy for ≥ T2 stage GB carcinoma showed that robotic surgery was associated with less blood loss (382.7 mLvs644 mL),shorter hospitalization (6.9 dvs8.4 d),and equivalent 3-year overall survival (92.3%vs96.3%) and disease-free survival (84.6%vs78.3%) compared to open surgery[127].
Chemotherapy
Chemotherapy has seen increased acceptance in the management of GB carcinoma in combination with systemic therapy,either as neoadjuvant therapy for downstaging in borderline resectable cases and adjuvant therapy in operable cases or as palliative treatment in inoperable cases[128-130].Perioperative chemotherapy is increasingly being used[131].Neoadjuvant chemotherapy may increase survival[132].
There are several schemes,but gemcitabine with cisplatin (the standard chemotherapy) in combination with immunotherapy with pembrolizumad or durvalumab and targeted treatment as first-line therapy is widely preferable[128,133].For second-line therapy,folonic acid (leucovorin),5-fluorouracil,oxaliplatin (FOLFOX) or irinotecan with 5-fluorouracil is indicated[128].FOLFOX chemotherapy has been proven effective after gemcitabine-cisplatin treatment in increasing overall survival at 6 and 12 mo[134].
Adjuvant chemotherapy alone or combined with radiotherapy is recommended in every case of ≥ T2 disease stage.However,it has absolute indications in high-risk patients,which are those with positive lymph node involvement,microscopic infiltration of the resection margin (R1 resection),perineural invasion or vascular invasion[135-137].
Neoadjuvant chemotherapy with gemcitabine-cisplatin followed by curative surgery increased survival compared to surgery alone[138].For advanced inoperable GB carcinoma,the combination of gemcitabine and either cisplatin or S-1 (modified regimens of 5-fluorouracil) or gemcitabine,cisplatin,and S-1 has been used as first-line chemotherapy[116].
Chemoresistance,particularly in gemcitabine of GB carcinoma or even cisplatin,occurs frequently and constitutes an important problem that affects treatment efficacy[139].This is attributed to the effects of the produced cytokines against apoptosis.Expression of some miRNAs (miR-125b-5p,miR-205-5p,miR-31) are implicated in this drug resistance and could be used as diagnostic biomarkers.In addition,recent research efforts have focused on the innovation of novel drugs that could overcome chemoresistance[140].
In the case of high microsatellite instability and chemoresistance,the immunotherapeutic pembrolizumad may be efficient[116].In cases of locally advanced or inoperable metastatic stage IV GB carcinoma,the addition of nab-paclitaxel to the standard gemcitabine-cisplatin treatment (GCNP scheme) as first-line therapy exhibited an increased response with potential resection after downstaging and prolonged survival[141].Patients with resistance to gemcitabine-cisplatin as first-line therapy may benefit from second-line therapy with trifluridine-tipiracil and irinotecan[48].
It has been recently proposed that adjuvant combined chemoradiation therapy instead of chemotherapy alone provides improved survival after curative surgical resection,particularly for those with advanced stage (III,IV) disease and lymph node-positive cases[142-144].Chemoradiotherapy had a beneficial effect independent of lymph node status[145].
Immunotherapy
Despite the increasing application of immunotherapy in many carcinomas,its use in GB carcinoma is still limited[146-148].Immunotherapy includes targeting checkpoint inhibitors such as monotherapy,vaccines,oncolytic viruses,adoptive cells,and cytokines (interleukin-2,interferon-α,granulocyte-macrophage colony-stimulating factor).Monoclonal antibodies against programmed cell death 1 (PD-1) (pembrolizumab,nivolumab and camrelizumab) and PD-L1 (durvalumab and atezolizumab) have been applied during the last decade in various solid tumors[146,147].However,there are still no reliable markers predicting immunotherapy effectiveness[147].
A heterogeneous immune microenvironment and increased expression of the immune checkpoint inhibitors PD-1 and TIM3 have been correlated to worse prognosis.Thus,their simultaneous blockage as potential targets could be an effective novel treatment[145].
In inoperable advanced cases,the combination of treatment (KEYNOT-966 trial) by pembrolizumab with gemcitabine and cisplatin improved survival compared to treatment with gemcitabine and cisplatin alone[133].Additionally,the TOPAZ 1 trial used durvalumab instead of pembrolizumab as immunotherapy in the same scheme for such cases,with similar results[148].Nevertheless,immunotherapy in such advanced cases improved unbearable pain relief,reducing opioid use[149].
Targeted therapy
Molecular profiles and a better understanding of the mechanisms involved in carcinogenesis,growth,invasion and metastasis have led to the search for certain targetable mutated genes by monoclonal antibody biological targeted treatment in solid tumors.This endeavor may improve survival and constitute a short future research direction.However,for GB carcinoma,more work is needed in the field[42,44,150].
Several targeted genomics,including potent sensitive mutations,have been assessed against the genesPD-1,PDL-1,HER2,VEGF,N-cadherin,VEGFR,EGFR,mTOR,MET,PI3K,MEK1,andMEK2[15].For targeted therapy,the following factors are used: (1)NTRKgene alterations (larotrectinib or entrectinib);(2)BRAF V600E(B-Raf proto-oncogene serine/threonine kinase) mutated gene (combination of dabrafenib with trametinib)[151];(3)HER2(human epidermal growth factor-2) gene reinforcement (trastuzumab with pertuzumab or trastuzumab with deruxtecan)[49];(4)RETgene alterations (selpercatinib);(5)FGFR-2gene (fibroblast growth factor receptor-2) alterations (multityrosine kinase inhibitors,i.e.pemigatinib,infigratinib,futibatinib,derazantinib,erdafitinib,ponatinib,debio-1347);(6) EGFR (cetuximab,panitumumab);and (7) IDH inhibitors (ivosidenib)[20,42,46,128,152].
Radiotherapy
The role of radiation therapy in GB carcinoma is limited.It is usually combined with chemotherapy as adjuvant or neoadjuvant treatment[142-144].The progress made by precise stereotactic body radiotherapy has limited side effects by providing accurate targeting and increased effectiveness[128,153].Patients with lung and lymph node metastases had better response to radiotherapy[154].It has also been recommended in combination with chemotherapy after R1 resection[155].
PROGNOSIS
Seventy percent of GB carcinomas are not amenable to radical surgery.However,for those receiving curative resection,recurrence is common.Early recurrence predicts worse prognosis[60].A recent study of 1601 GB carcinoma patients who underwent surgical resection were followed for survival.The 5-year survival rate for stage I was 82.7%,73.4% for stage II,31.9% for stage IIIA,24.1% for stage IIIB,and 10% for stage IV.They found that adjuvant treatment had a beneficial effect[156].Likewise,a study in Japan of 200 GB carcinoma patients who underwent surgical resection reported the following 5-year overall survival rates: Stage I,90.8%;stage IIA,94.4%;stage IIB,73.6%;stage IIIA,33.7%;stage IIIB,57.7%;stage IVA,14.3%;and stage IVB,11.8%[88].A study conducted in Australia including 104 patients with GB carcinoma and a median follow-up of 60 mo found a median overall survival of 35 mo in those with intended curative resection and 4 mo in inoperable cases with palliative treatment[36].For a T1b follow-up of 69.9 mo,the disease-free survival was 92%[50].For advanced stage III-IV GB carcinoma patients,the overall survival was as follows: 1-year at 47.6%;2-year at 29.1%;and 3-year at 19.9%[157].
The site of metastases (liver,distant lymph nodes,lung,bone,brain) may have an effect on survival.The most common sites of liver and lymph nodes can be affected by primary tumor resection[158].More removed lymph nodes (above 6) are associated with better survival when they are negative[159].
Revealing residual disease in the specimen of the second operation after incidental discovery of GB carcinoma with cholecystectomy predicts worse prognosis,despite the achievement of R0 resection[160].The ratio of γ-glutamyl transferase to platelet count may predict GB carcinoma patient survival and was included in a relevant nomogram[161].There are several prognostic scoring systems and nomograms predicting survival[162-166] or lymph node metastases[167].Three immunological markers (TRAIL,TIE2,CSF1) in plasma were associated with survival after surgery[168].Infiltrated lymph nodes and the degree of cell differentiation in stage T1b-T2 GB carcinoma restrict survival[169].The presence of acute cholecystitis in GB carcinoma patients had a negative influence on prognosis[170].
A recent multicenter study conducted in Japan of 290 patients found that postoperative infectious complications negatively affect prognosis.They reported a median overall survival in the infection group of 38 movs62 mo in the noninfection group[171].
Food insecurity may affect long-term postoperative outcomes,reducing survival[172].
It was found that immunohistochemical markers MRP2,CXCR4,and PD-L1 were associated with increased survival and could be used as prognostic biomarkers[173].Additionally,PD-L1 and NY-ESO1 are indicative markers for immunotherapy[150,174].The predictive factors for favorable prognosis are shown in Table 3[34,112,156,169,170].

Table 3 Predictive factors for favorable prognosis of gallbladder carcinoma
NEW DIRECTIONS AND PERSPECTIVES
In summary,surgery is the main therapeutic first step;nevertheless,it is impracticable in most cases,and when it is achieved,it is often accompanied by recurrence.Neoadjuvant treatment may ensure better local control in a manner of downstaging the disease.Moreover,it allows potential R0 resection,contributing to limited recurrence[175].The use of 6 mo of capecitabine treatment after therapeutic excision represents a standard cure.However,novel adjuvant systemic treatment opens new perspectives[176].First-line treatment with cisplatin and gemcitabine combined with immune checkpoint inhibitors and targeted therapy has broadened the management horizons of advanced biliary tract carcinoma[177,178].
CONCLUSION
GB carcinoma is relatively uncommon but has a dismal prognosis.It is usually diagnosed in an advanced,inoperable stage,where palliative systematic treatment is the only option.However,progress in diagnostic modalities may allow for earlier detection,and its management is rapidly evolving.Radical surgery followed by adjuvant therapy with capecitabine and cisplatin as the first-line therapy,followed by 5-fluorouracil and oxaliplatin-irinotecan as the second-line therapy,offers the best chance for a cure.Management through surgery is dependent on T stage classifications.However,the most extended operative procedures remain in recent debate.Multimodality treatment is needed.Targeted therapies and immunotherapy constitute novel treatments but do not have the same efficacy as in other solid tumors.Research efforts are ongoing with promising prospects.An individualized approach could be more appropriate.
FOOTNOTES
Author contributions:Pavlidis TE designed research,contributed new analytic tools,analyzed data and review;Galanis IN analyzed data and review;Pavlidis ET performed research,analyzed data,review,and wrote the paper.
Conflict-of-interest statement:There is no conflict of interest associated with the senior author or any of the other coauthors who contributed their efforts in this manuscript.
Open-Access:This article is an open-access article that was selected by an in-house editor and fully peer-reviewed by external reviewers.It is distributed in accordance with the Creative Commons Attribution Non-Commercial (CC BY-NC 4.0) license,which permits others to distribute,remix,adapt,build upon this work non-commercially,and license their derivative works on different terms,provided the original work is properly cited and the use is non-commercial.See: https://creativecommons.org/Licenses/by-nc/4.0/
Country/Territory of origin:Greece
ORCID number:Efstathios T Pavlidis 0000-0002-7282-8101;Ioannis N Galanis 0009-0001-4283-0788;Theodoros E Pavlidis 0000-0002-8141-1412.
S-Editor:Fan JR
L-Editor:Filipodia
P-Editor:Zhang XD
杂志排行
World Journal of Gastrointestinal Oncology的其它文章
- Comprehensive analysis of the role of ubiquitin-specific peptidases in colorectal cancer: A systematic review
- Colonoscopy plays an important role in detecting colorectal neoplasms in patients with gastric neoplasms
- Analysis of the potential biological value of pyruvate dehydrogenase E1 subunit β in human cancer
- Colorectal cancer’s burden attributable to a diet high in processed meat in the Belt and Road Initiative countries
- Emerging role of liquid biopsy in rat sarcoma virus mutated metastatic colorectal cancer: A case report
- Comprehensive evaluation of rare case: From diagnosis to treatment of a sigmoid Schwannoma: A case report
