Trends in prevalence and disability-adjusted life years of cataract in China from 1990 to 2019
2024-01-20
Abstract
•KEYWORDS:cataract; prevalence; disability-adjusted life years (DALYs); disease burden
INTRODUCTION
Cataracts stand as a significant global contributor to blindness and visual impairment. This degenerative ailment, characterized by a reduction in lens transparency or color change, is particularly prevalent in developing countries, according to epidemiological investigations[1-2].Afflicting the elderly predominantly, with a staggering 92.6% prevalence rate among those over 80 years old[2], cataracts represent a major age-related eye disease leading to blindness. Despite an overall decline in prevalence, more than 35 million individuals worldwide still suffer from moderate or severe visual impairment attributed to cataracts[3]. As cataracts progress to stages affecting vision, the impact extends beyond physical consequences, giving rise to psychological distress for patients and a decline in overall quality of life[4-5]. Cataract surgery has greatly improved the visual quality of patients. However, with an aging global population and increased life expectancy, the public health and socio-economic ramifications linked to cataracts and their complications are poised to escalate[6].
The Global Burden of Diseases (GBD) database encompasses comprehensive epidemiological information on 369 diseases and injuries across 204 major countries andregions[7]. Unlike prior research that has explored the prevalence trends of cataracts[8], our focus extends to describing the disease burden by age, sex, and social development index (SDI) from 1990 to 2019. Additionally, we draw comparisons between China and its neighboring countries. The aspiration is that the findings from this study will serve as a foundation for the development of targeted population screening strategies, ultimately reducing the prevalence of cataract-induced blindness more effectively.
MATERIALSANDMETHODS
EthicalApprovalThe study obtained clearance from the institutional review board at Wenzhou Hospital of Integrated Traditional Chinese and Western Medicine in Zhejiang Province, China. Approval was deemed unnecessary as the research exclusively utilized publicly available data. The study is based on data obtained from a public database (https://vizhub.healthdata.org/gbd-results/), and access to it does not require any permissions.
DataAcquisitionData pertaining to cataracts, including prevalence, disability-adjusted life years (DALYs), numbers, and rates, were extracted from the GBD 2019 Study website. These publicly available data were accessible through the Global Health Data Exchange (GHDx, https://vizhub.healthdata.org/gbd-results/). A comprehensive methodology, detailed in a previous study[9], guided the estimation of prevalence and DALYs related to cataracts. DALY serves as a holistic measure of disease burden, representing the number of years lost due to poor health, disability, or premature death. Data sources encompassed literature reviews, scientific reports from registers and cohorts, administrative health data, and demographic surveys[7]. All measurements were reported based on the original values, ratios per 100 000 population, and age-standardized ratios (ASRs) per 100 000 population. Age standardization was in accordance with the standard age structure of the World Health Organization. Descriptive and visual analyses covered cataract prevalence and DALYs data from 1990 to 2019 by gender, age, region, and year. Uncertainty intervals (UI) were established using the 2.5th and 97.5th ordered 1000 draw values of the posterior distribution[10]. The prevalence of cataracts employed Disease Modeling-Meta Regression with the pooled epidemiology database, estimated through random-effects meta-analysis methods[11].
StatisticalAnalysisASRs served as a metric for assessing changes in disease patterns across population distributions, reported per 100 000 population in a specific year, with point estimates having a 95%UI. The ASR (per 100 000 population) is calculated using the following formula:
Where,aidenotes a specific age ratio in theithage group,widenotes the number of individuals (or weight) in the correspondingithage group for the chosen reference standard population, and A denotes the total number of age groups.
The estimated annual percentage change (EAPC) was used to evaluate the trends of ASR, which were calculated using the regression model: y=α +βx+ε, where y=l n (ASR), x is the calendar year, and ε is the error term. EAPC = 100 × (exp (β) -1) and its 95%UIwere obtained from the regression model. A negative EAPC and lower limit of UI indicated a descending trend, while a positive EAPC and upper limit of UI suggested an ascending trend. All figures were generated using GraphPad Prism software (version 9.0.0, GraphPad Prism Software; San Diego, CA, USA) and R program (version 4.2.3, R core team).
RESULTS
TimeTrendsforthePrevalenceandDisability-AdjustedLifeYearsofCataractDegenerationinChinafrom1990to2019As shown in Figure 1, the prevalent of cataract cases experienced a remarkable surge of 223.54% from 1990 (5.61×106, 95%UI: 4.90×106to 6.40×106) to 2019 (1.81×107, 95%UI: 1.56×107to 2.08×107). Throughout this period, the prevalence of cataracts among females consistently exceeded that of males. Concurrently, the prevalence rate exhibited a significant upward trend, escalating by 169.25% over the past three decades (1990=473.74, 95%UI: 413.62 to 540.93; 2019=1 275.53, 95%UI: 1 097.98 to 1 465.30 per 100 000 population; Figure 1A-1B). However, upon standardizing for population size and age structure, the age-standardized prevalence rate (ASPR) was observed at 867.09 (95%UI: 761.36 to 975.42 per 100 000 population) in 1990, with troughs and peaks observed in 1995 and 2017 (1995=796.01, 95%UI: 699.80 to 896.57; 2017=1 066.90, 95%UI: 935.43 to 1 203.66 per 100 000 population, respectively). Subsequently, it gradually decreased to 991.56 (95%UI: 861.52 to 1 131.04 per 100 000 population) in 2019 (Figure 1C).
Similar to the prevalence trends, the number of DALYs exhibited a gradual increase, surging by 142.14% from 449 322.84 (95%UI: 317 651.80 to 618 751.82) in 1990 to 1 087 987.61 (95%UI: 761 917.08 to 1 487 672.38) in 2019. Meanwhile, the DALYs rate raised by 101.51% from 37.96 (95%UI: 26.84 to 52.27) in 1990 to 76.50 (95%UI: 53.57 to 104.59) in 2019 (Figure 1D-1E). However, the trend of age-standardized DALYs rate (ASDR) fluctuated from 1990 to 2019, with the minimum and maximum values occurring in 1995 and 2001 (1995=58.69, 95%UI: 41.32 to 79.71; 2001=76.28, 95%UI: 53.62 to 103.19 per 100 000 population, respectively). Subsequently, it rapidly dropped to 59.16 (95%UI: 41.70 to 80.15 per 100 000 population) in 2019 (Figure 1F). In terms of gender, females were consistently more susceptible to the burden of cataract-related diseases than males over the past 30 years.
DifferencesinAgeandGenderBurdenAttributabletoCataractDegenerationinChinaBetween1990and2019As depicted in Figure 2, cataracts were exclusively observed in individuals aged 20 and above. When examining gender disparities in 1990, DALYs cases were higher in females (268 605.12, 95%UI: 191 239.94 to 368 524.29) than in males (180 717.72, 95%UI: 126 384.78 to 250 235.49). This gender contrast persisted in 2019, with female DALYs cases numbering 667 683.36 (95%UI: 470 817.20 to 905 386.26) and male cases at 420 304.26 (95%UI: 294 944.25 to 582 247.37). Additionally, prevalent cases in females (3 389 569.02, 95%UI: 2 949 971.84 to 3 847 246.49) surpassed those in males (2 218 031.92, 95%UI: 1 928 740.42 to 2 537 501.91) in 1990. This trend persisted in 2019, with prevalent cases in females (11 159 984.56, 95%UI: 9 618 369.08 to 12 767 304.08) and males (6 982 584.40, 95%UI: 5 988 188.77 to 8 089 726.50), respectively.
When stratified by age groups, the highest number of DALYs, 191 123.25 (95%UI: 131 987.88 to 270 175.76), occurred in the 70 to 74 years age group in 2019. Similarly, the most prevalent cases, 1 045 828.43 (95%UI: 829 688.49 to 1 303 784.47), were observed in the same age group, with females at 1 954 010.79 (95%UI: 1 530 967.78 to 2 466 945.49) and males at 1 266 203.56 (95%UI: 981 393.40 to 1 613 267.51). Notably, the prevalence of cataracts and DALYs in China was predominantly higher in females, both in 1990 and 2019. This pattern was particularly pronounced for females aged over 85, where the incidence rate of cases exceeded two times that of males.
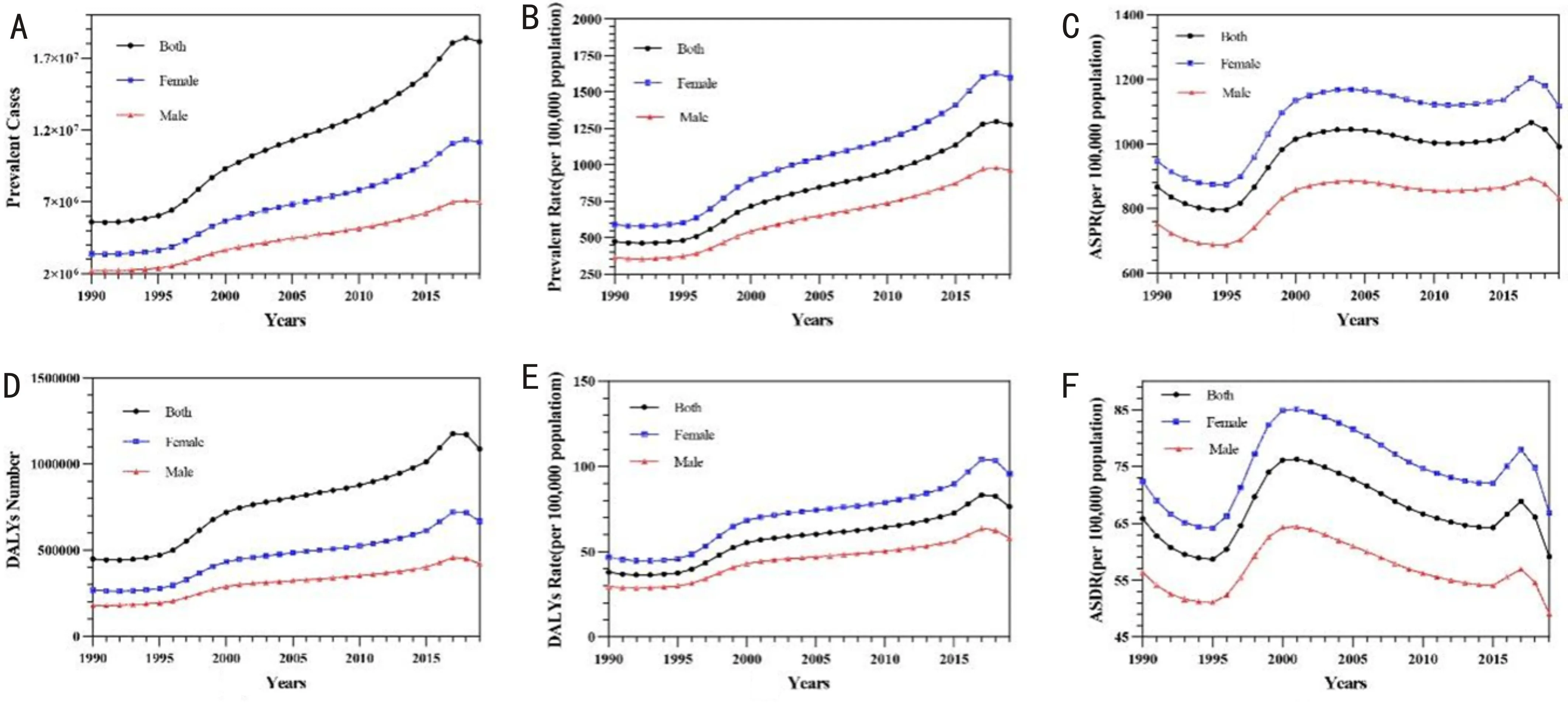
Figure 1 Prevalence and disability-adjusted life years of cataract degeneration from 1990 to 2019 in China. A: Number of prevalent cases; B: Crude prevalent rate; C: Age-standardized prevalence rates; D: Number of DALYs; E: Crude DALYs rate; F: age-standardized DALY rates. Red and blue line segments represent female and male, respectively. ASPR: Age-standardized prevalence rates; DALYs: Disability-adjusted life years; ASDR: Age-standardized DALY rates.
DifferencesinCataractDiseaseBurdenbetweenChinaandNeighboringCountriesfrom1990to2019Analyzing the ASR and cases provides insights into the evolving disease burden of cataracts in China and neighboring countries from 1990 to 2019. Among the neighboring nations, Indonesia exhibited the highest ASDR and ASPR for blindness and vision loss due to cataracts in 2019 (338.64 and 3 599.99 per 100 000 populations, respectively). This was followed by Pakistan (273.31 and 3 184.53 per 100 000 populations) and Myanmar (217.49 and 3 066.19 per 100 000 populations), demonstrating a significant decline compared to 1990. Conversely, North Korea (18.63 per 100 000 population), Japan (19.25 per 100 000 population), and South Korea (20.34 per 100 000 population) had the lowest ASDR among neighboring countries. Remarkably, China ranked 13th (ASDR: 59.16 per 100 000 populations) and 12th (ASPR: 991.56 per 100,000 populations) in 2019, reflecting comparatively low rates (Figure 3A-3B).
In contrast to the changing ASR trend, the overall number of events exhibited an upward trajectory over the past three decades. Among neighboring countries, India recorded the highest number of DALYs and prevalence of blindness and vision loss due to cataracts in 2019 (DALYs number=2 037 409.11, 95%UI: 1 459 770.20 to 2 721 858.22; prevalent cases=28 092 006.92, 95%UI: 24 739 238.87 to 32 157 180.02). China followed closely (DALYs number=1 087 987.61, 95%UI: 761 917.08 to 1 487 672.39; prevalent cases=18 142 568.96, 95%UI: 15 617 088.67 to 20 841 571.94), and Indonesia ranked third (DALYs number=641 584.7304, 95%UI: 453 513.57 to 874 043.46; prevalent cases=6 754 971.085, 95%UI: 6 137 036.66 to 7 451 019.04; Figure 3C-3D). This indicates that, despite a decrease in disease burden related to ASR, the substantial demographic characteristics contribute to the sustained high number of cases in public health governance.
TemporalTrendsinCataractBurdenamong204CountriesandTerritoriesfrom1990to2019On a national scale, both ASDR and ASPR exhibited a consistent downward trend across almost all countries and territories from 1990 to 2019. Notably, Equatorial Guinea demonstrated the most substantial decrease in ASR, with the EAPC in ASPR at -3.21 (95%UI: -3.39 to -3.03) and EAPC in ASDR at -4.05 (95%UI: -4.25 to -3.86). Conversely, only one country, Burkina Faso, displayed a slight upward trend in ASR for both Prevalence and DALYs, with EAPC in ASPR at 2.07 (95%UI: 1.69 to 2.46) and EAPC in ASDR at 1.26 (95%UI: 0.89 to 1.621). Cte d’Ivoire (EAPC in ASPR=1.16, 95%UI: 0.5 to 1.82; EAPC in ASDR=0.71, 95%UI: 0.09 to 1.34) and Benin (EAPC in ASPR=1.28, 95%UI: 1.09 to 1.47; EAPC in ASDR=0.64, 95%UI: 0.45 to 0.83) also showed a slight increase. At the national level, a significant disparity in cataract ASPR and ASDR was observed among various countries in 2019. Seven countries and territories reported ASDR exceeding 200/100 000 person-years, with Indonesia having the highest (338.6/100 000 person-years, 95%UI: 240.2 to 460.3), followed by Pakistan (273.3/100 000 person-years, 95%UI: 195 to 368.6) and Ethiopia (233.5/100 000 person-years, 95%UI: 165.5 to 318.1). Remarkably, 96 countries and territories reported an ASPR beyond 1 000/100 000 person-years, constituting nearly half of the total. Indonesia (3 600/100 000 person-years, 95%UI: 3 279.9 to 3 962.8), Pakistan (3 184.5/100 000 person-years, 95%UI: 2 859.8 to 3 551.8), and Cambodia (3 071/100 000 person-years, 95%UI: 2 738.7 to 3 414.9) reported the highest ASPR, while Bulgaria had the lowest (245.1/100 000 person-years, 95%UI: 197.1 to 297.9) globally. Despite the high absolute values of ASDR and ASPR, the EAPC in most countries and regions exhibited a consistent downward trend (Figure 4).

Figure 3 The evolving trend of disease burden due to cataracts in China and other neighboring countries by the social development index for both sexes from 1990 to 2019. A: Age-standardized DALYs rate (ASDR); B: Age-standardized prevalence rate (ASPR); C: DALYs number; D: Prevalent cases. DALYs: Disability-adjusted life years.

Figure 4 Global distribution of the age-standardized rates of cataract prevalence and disability-adjusted life years in 2019, along with their estimated annual percentage changes from 1990 to 2019. A: Age-standardized prevalence rate (per 100 000) in 2019; B: Global distribution of EAPC in age-standardized prevalence rate of cataracts from 1990 to 2019; C: Age-standardized DALYs rate (per 100 000) in 2019; D: Global distribution of EAPC in age-standardized DALYs rate of cataracts from 1990 to 2019. ASPR: Age-standardized prevalence rate; ASDR: Age-standardized DALYs rate; DALYs: Disability-adjusted life years; EAPC: Estimated annual percentage changes.
DISCUSSION
Over the past three decades, both the ASDR and ASPR of cataracts in China have exhibited a notable decrease. However, the absolute number of new cataract cases and the years of disability-adjusted life expectancy have increased, attributed to the advent of a society experiencing severe population aging and a rise in the popularity of visual health examinations among the elderly. Age, sex, and race, being crucial and immutable risk factors for senile cataracts, are supplemented by the suggestion from scholars that certain socioeconomic and lifestyle factors may influence cataract progression[12-13].
A surprising revelation has emerged regarding gender inequality contributing to the cataract burden in China since 1990, escalating with age and reaching a gap of 2 to 3 times between the sexes in the higher age groups. Notably, gender disparities in cataract patients may be closely linked to life expectancy. According to demographic data from the Institute for Health Metrics and Evaluation in 2017[14], the number of females among the elderly population over 80 years old significantly exceeded that of males (80 to 84: Male, 8.18M, Female, 10.05M; 85 to 89: Male, 3.37M, Female, 4.98M; 90 to 94: Male, 832.88K, Female, 1.64M; 95+: Male, 118.54K, Female, 326.24K, respectively). Furthermore, studies indicate an increased risk of cataracts among those with lower household economic income and education levels. A Korean study on cataract epidemiology revealed a more pronounced economic disparity for females[15], emphasizing the need for further exploration in this domain. Despite global studies on the disease burden of cataracts, none have specifically addressed the situation in China. An analysis by Louetal[16]on the global cataract burden revealed a declining trend in global ASDR, inversely associated with the human development index (β=-0.522,P<0.01) from 1990 to 2013. Louetal[16]also reported a substantial increase of 89.42% in global DALYs numbers for cataract vision loss, with females exhibiting a higher crude rate of 38.29 after adjusting for age and country from 1990 to 2015[17]. Following the updated GBD 2019 database, Fangetal[18]further demonstrated associations between aging, females, lower socioeconomic status, and a higher cataract burden. Remarkably, despite the use of different GBD database versions, these studies arrived at relatively similar conclusions. The declining trend of ASDR and prevalent cases in China indicates positive progress in cataract prevention and treatment, with further guidance anticipated as public databases continue to improve.
According to data from the 2017 GBD Study[19], visual impairment ranked as the third leading cause of impairment, following anemia and heart failure. Our findings indicate a decrease in the disease burden of cataracts in China over the past three decades, following a standardized adjustment for population structure. In comparison to neighboring countries, China’s ranking in age-standardized cataract prevalence and DALYs rates dropped from ninth to eleventh and tenth, respectively (Figure 3A-3B). Additionally, both ASDR and ASPR displayed a declining trend from 2017 to 2019 (Figure 1C-1F). These results demonstrate a significant progress in cataract prevention and treatment in China. However, the persistence of visual impairment remains a serious concern, particularly among the elderly, females, and those with lower education levels[20-21]. This issue persists despite increased awareness of eye health and the widespread adoption of the national physical fitness testing system.
The Institute for Health Metrics and Evaluation categorizes the world into 204 countries and territories based on geographical location and levels of economic development[7]. In 2019, both the ASPR of blindness and vision loss due to cataracts and the ASDR in China were notably lower than the average levels observed in most regions (Figure 4). This difference may be attributed to economic development, improved allocation of medical resources, and the increasing prevalence of cataract surgery in the elderly in recent years[22].
Despite the notable strengths of this study, including its large-scale public database, several limitations should be acknowledged. First, the reliance on a large public database introduces a certain lag in updating the original data, limiting the inclusion of the latest research results. Second, evolving definitions and diagnoses of cataracts over time in different countries pose a potential source of bias. Finally, the absence of detailed data from various provinces in China hinders the analysis of specific cataract burdens at the provincial level.
CONCLUSION
In summary, the prevalence and DALYs of blindness and vision loss due to cataracts in China have witnessed a significant increase from 1990 to 2019, with females and the elderly bearing a disproportionate burden of the disease. Addressing this issue requires an improvement in the distribution of medical resources and the establishment of an early cataract screening system for those at high risk.