Post-hepatectomy liver failure: A timeline centered review
2024-01-02MohmBkhitLisGrunyAhmKASlihPtruBucurEricVibrtMussrGhznfr
Mohm Bkhit ,Lis Gruny ,Ahm KA Slih ,b,Ptru Bucur ,Eric Vibrt ,Mussr Ghznfr
a Department of Surgery,NHS Grampian,Foresterhill Health Campus,Ashgrove Road,AB252ZN Aberdeen,UK
b Institute of Medical Sciences,Medical School,Foresterhill Health Campus,Ashgrove Road,AB252ZN Aberdeen,UK c Hépatica,Integrated Center of HPB Care,Elite Hospital,Agriculture Road,Alexandria,Egypt
d Department of Surgery,University Hospital Tours,Val de la Loire 37000,France
e Centre Hépatobiliaire,Paul Brousse Hospital,12 Paul Valliant Couturier,94804 Villejuif,France
Keywords: Post-hepatectomy liver failure Liver neoplasms Prediction Prevention Management
ABSTRACT Background: Post-hepatectomy liver failure (PHLF) is a leading cause of postoperative mortality after liver surgery.Due to its significant impact,it is imperative to understand the risk stratification and preventative strategies for PHLF.The main objective of this review is to highlight the role of these strategies in a timeline centered way around curative resection.Data sources: This review includes studies on both humans and animals,where they addressed PHLF.A literature search was conducted across the Cochrane Library,Embase,MEDLINE/PubMed,and Web of Knowledge electronic databases for English language studies published between July 1997 and June 2020.Studies presented in other languages were equally considered.The quality of included publications was assessed using Downs and Black’s checklist.The results were presented in qualitative summaries owing to the lack of studies qualifying for quantitative analysis.Results: This systematic review with 245 studies,provides insight into the current prediction,prevention,diagnosis,and management options for PHLF.This review highlighted that liver volume manipulation is the most frequently studied preventive measure against PHLF in clinical practice,with modest improvement in the treatment strategies over the past decade.Conclusions: Remnant liver volume manipulation is the most consistent preventive measure against PHLF.
Introduction
Curative surgery remains the gold standard treatment for liver tumors within a multimodal management approach [1].However,feasibility of curative resection is hampered by the limits of residual functional liver volume.The adequacy of volume and function of the remnant liver depends on the extent of resection,and any associated liver disease including cirrhosis,steatosis,and postchemotherapy liver disease.This necessitates a careful preoperative planning for any major hepatectomy to avoid post-hepatectomy liver failure (PHLF).
PHLF is one of the severe complications after hepatectomy,and a leading cause of death [2].It is a functional failure whereby the residual liver is unable to maintain one or more of its synthetic,excretory,and detoxifying functions which manifests as impaired coagulation and hyperbilirubinemia typically on postoperative day 5 (POD5) [3].PHLF is linked with sepsis,or ischemia-reperfusion injury which can ultimately lead to death [4].The incidence of PHLF in the literature varies between 1% and 32% [5].There has been a steady decrease in PHLF over the last decade due to the improvement in understanding of risk factors and defining preventative strategies.Terms like PHLF and small-for-size syndrome share common mechanisms causing a contextual perplexity [6].This review adopted the term PHLF given the clinical context of resection as adopted by The International Study Group of Liver Surgery (ISGLS) [7].
Whilst the literature addressing PHLF appears ubiquitous,there is no specific structure that summarizes the evidence that can guide surgeons regarding the timeline of the preventive measures against PHLF.The objective of this review is to summarize the published measures and their sources of evidence,in a timeline centered way around the index (i.e.,definitive) hepatectomy,thus,summarizing the practice in prediction,prevention,and treatment of PHLF at different time points through the patient journey from diagnosis,through resection and to the treatment of the PHLF.
Eligibility criteria and search strategy
This review included both human and animal studies on major hepatectomy aimed at prediction,prevention,diagnosis,or management of PHLF.We summarized the measures to predict,prevent,diagnose,and manage PHLF.The review followed the Preferred Reporting Items for Systematic reviews and Meta-Analyses(PRISMA) guidelines [8].
A literature search was conducted by two independent researchers (Bekheit M and Grundy L) who were blinded to each other’s work,across the Cochrane Library,Embase,MEDLINE/PubMed,and Web of Knowledge electronic databases published before December 2019 in English.Subsequently,hand searches of relevant citations were conducted by three researchers(Bekheit M,Grundy L and Salih AKA) and the search was periodically updated until June 2020.Studies presented in other languages were equally considered for inclusion based on the inclusion and exclusion criteria and the presence of an abstract in English,French,or Italian.A comprehensive search strategy using a combination of free text,and medical subject headings (MeSH) was tailored across the major electronic databases in accordance with each of the individual indexing terms.
Selection process
The review included all types of studies,editorial,letters,comments,review articles,and conference abstracts.The titles and abstracts from the search results from each database was imported to Rayyan platform (www.rayyan.qcri.org).Duplicates were excluded and screening of the remainder of the list was performed by authors as above.Full-text articles were retrieved for the shortlisted titles and abstracts and the final list of studies was included in the summary.The final list was imported to Mendeley® Citation manager (Elsevier,London,UK),which was then used to create the citation list.
The selection process was carried out independently and blindly as indicated above.Any conflict in inclusion of a particular study was resolved with consensus.While this review focused on PHLF after major resection,limited citations from partial liver transplantation context were used as an analogy to the pathophysiology in the context of resection.These citations were utilized from hand search during specific search for mechanisms to explain certain findings.
Data collection was performed independently.The review used a specific Patient,Intervention,Comparison,and Outcome (PICO)structure focused on the interventions and outcomes related to prediction,prevention,diagnosis,and treatment of PHLF.Data related to the study specific PICO were extracted in Microsoft Excel(2016).
The review explored the definition of PHLF.Previously there was no universally accepted definition of PHLF,and multiple definitions have been proposed for postoperative hepatic insufficiency [3].In the last two decades,common themes agree on the principle of abnormal levels for bilirubin and/or coagulation markers as indicators for PHLF.The cut-off criterion may slightly differ from series to series,but this concept has been validated in over 12000 patients [3].
The “50-50 criteria” outlined by Balzan and colleagues indicate the presence of reduction of the prothrombin activity to less than 50% of baseline and serum bilirubin >50 μmol/L (>3 mg/dL) on POD5 is associated with 59% risk of early postoperative mortality of inpatient mortality in patients who met both criteria [9].The“50-50 criteria” have been prospectively validated [10].In a retrospective multicenter cohort of 1059 patients,Mullen et al.have suggested postoperative peak bilirubin >7 mg/dL (>119 μmol/L)as a sole criterion for PHLF with reported specificity and sensitivity of 94.3% and 93.3%,respectively [2].The peak bilirubin level has additionally been validated as a long-term prognostic factor [11].The ISGLS in a consensus conference in 2011 used POD5 as a defining point for PHLF indicating hyperbilirubinemia and/or a rise in INR as characteristic of liver dysfunction [3,12].The group grades PHLF severity from A to C.Grade A indicates deranged liver function test without change to clinical management;grade B changes clinical management but does not require invasive treatment;and grade C indicates profound dysfunction requiring invasive treatment [12].In severe cases it can lead to gastrointestinal hemorrhage,sepsis,and eventual fulminant hepatic failure with subsequent death [4].Typically,PHLF occurs on PODs 3-7 with increased bilirubin and intractable ascites [4,13].Up to half the patients with PHLF died from sepsis within the first postoperative month [14].
This review followed a pragmatic approach in evaluating the quality and risk of bias in the included studies to fit with the scope of the review.Studies were initially classified and ranked based on their design using the Oxford levels of evidence [15].Subsequently,quality assessment was performed using Downs and Black’s checklist [16].The review presented a summary of quality and a risk of bias assessment for the study ranked highest in design.This review followed a systematic approach in search and the findings were summarized in a narrative timeline format.Results from studies with common specific outcomes were summarized together instead of the traditional PRISMA recommendation to provide a more relevant overview.There was no meta-analysis planned as part of this review.Hence,reporting bias assessment was not considered as part of this protocol.
Included studies and quality assessment
This review included 245 studies in the summative analysis.PRISMA chart illustrates the search and selection process (Fig.1).There were 8 randomized clinical trials (RCTs),109 experimental studies,3 case reports,1 pilot and 124 retrospective cohorts and case series analysis.

Fig.1.PRISMA chart of the systematic review process.
This review utilized the Downs and Black concept of quality assessment and the summary of the scores for the RCTs were presented in Table S1 [17–24].There were two high quality studies addressing this subject.Grendar et al.[17]used the N-acetylcysteine and Petrowsky et al.[18]used pentoxifylline in their study.In both studies,no clinically meaningful difference was identified.The remainder of the RCTs scored moderate as in Table S1.
Pathophysiology of PHLF
The regenerating capacity of the remaining liver and its ability to maintain normal physiological functions are the key components to drive the pathophysiological response.The exact pathophysiology of PHLF is a matter of ongoing debate.However,there is a strong emphasis on imbalance between residual liver volume and portal hemodynamic as a cause of PHLF.
Implications of the hemodynamic in the development of PHLF
While PHLF has been known as small-for-size syndrome for many years,an emerging debate shed some light on one pathophysiological aspect of the process as a small for flow [25].Clinical observations found the association between the increased portal pressure and the development of PHLF [26].Other portal hemodynamic parameters -surrogate for increased portal pressure -have similarly been linked to PHLF within the experimental setting [27].
Reduction in hepatic micro-vasculature total surface area generates resistance within the portal vein,mediating cytokine injury to sinusoidal epithelium and Kupffer cells [13].There is subsequent dysregulated hepatic necrosis which contributes to the development of PHLF [28].The resulting effect is referred to as sinusoidal hyperperfusion (barotrauma) [29].This dysfunction is facilitated by a reflex dearterialization of the remnant liver [29].Portal hyperperfusion induces a hypermetabolic state [26,27]that generates oxidative stress,which can induce failure of the remnant liver to regenerate [30].Portal hyperperfusion adversely causes sinusoidal dilatation,centrilobular obliteration,cholestasis,hemorrhagic disruption of the sinusoidal basement membranes,oxidative stress,and inhibition of cellular function [4].Plugging of accumulated macrophages within sinusoids equally contributes to dysfunctional perfusion,adding to microcirculatory disturbance [31].
Role of remnant liver volume and regeneration in development of PHLF
Measures to prevent PHLF often look at the ‘safe’ limit of remnant liver volume,and it is generally agreed those with healthy livers can tolerate remnants between 25%-30%,while in co-morbid livers the residual remnant should aim to be 40%-50% of the original liver volume [32].However,it is commonly accepted that remnant liver volume to body weight ratio is more specific than remnant liver volume to total liver volume in predicting postoperative course after extended hepatectomy [33].Liver regeneration results from compensatory hyperplastic changes after liver injury [34].Cell signaling and remodeling of the extracellular matrix is vital to restore mass and microarchitecture [35].The growth pattern of hepatocytes is controversial,and some claim clonal hepatocyte development occurs equally within all hepatic lobule zones [36],while others state hepatocyte growth begins in the centrilobular area before slowly expanding into other lobular zones [37].Structure of hepatocytes is crucial for maintaining function,their polarity contributes to alignment and if the connection between hepatocytes and sinusoids is disrupted,then liver function is altered [38].The space of Disse is positioned between hepatocytes and endothelial cells lining sinusoids.It is within this space hepatocytes project their villi which increase metabolic exchange between the two cells.Understanding arrangement of hepatocytes in relation to sinusoidal cells is perhaps critical in understanding how PHLF develops.Hoehme and colleagues suggest hepatocytesinusoid alignment is crucial for liver regeneration and that misalignment could be a poorly recognized contributor to PHLF [39].
Gut microbiota and PHLF
The role of gut and microbiota in PHLF is emerging [40].Gut microbiota acts as a metabolic player that takes part in host metabolism by partially regulating bile acids metabolism,as well as farnesoid X receptor signaling.If microbiota functions are impaired,its role in supporting both bile acids and farnesoid X receptor pathways will be similarly undermined resulting in a diminished liver regeneration [41,42].In the initial period post-hepatectomy,bile acid plays a role in orchestrating the second wave of liver regeneration via fibroblast growth factor modulation [43–46].
Risk prediction and stratification of PHLF
For practical purposes,prediction is considered anticipating PHLF based on parameters obtained preoperatively.The pivotal importance of the prediction of a complication lies in providing the capability of prevention.The current practice takes into consideration the liver related factors including liver volume and functional assessment as major risk predicting factors for PHLF.Other risk factors include patient related factors and surgery related factors.
The risk factors are a collection of modifiable and nonmodifiable factors contributing to the development of PHLF.Not all these factors have a clearly known mechanism nor are part of the standard workup before surgery.Moreover,some of these factors are usually known in retrospect and not during preoperative workup,therefore losing their predictive ability.For this practical purpose,this review discriminates between the risk factors and prediction despite the overlap.
Patient related factors
Most of the described patient risk factors are markers of reduced physiologic capacity and reserve.The presence of these comorbidities: age >65 years,male,and diabetes mellitus place patients at higher risk of PHLF [47].The contribution of such risk factors to PHLF is not clear as these are potential causes of complication for many major operation [48].The older the patient,the lower the hepatic reserve [49].Unlike younger patients,those older than 69 years were only considered for resection if the future liver volume was greater than 45% of the original total liver volume [50].Bachellier et al.[51]showed male had 7.5 times risk for development of PHLF than female (odds ratio=7.5,95% confidence interval: 1.3-39.7).This may be due to elevated levels of immunosuppressing testosterone thus increasing likelihood of septic complications [52].There are likely to be other reasons why sex contributes to outcomes as it is a common observation [53].
Due to reduced capacity to meet metabolic demand,diabetes mellitus unsurprisingly places patients at higher risk of PHLF.Insulin alters immune and inflammatory response rendering diabetic patients vulnerable to PHLF [54].There was a 10-fold increase risk of PHLF in diabetic patients (29.2% vs.2.5%) [55].Similarly,metabolic syndrome has negative effect on the liver quality and capacity to regenerate [19,56,57].
Surgery related factors
Perioperative events can have significant impact on postoperative liver regeneration.Intraoperative blood loss and blood transfusions are recognized as risk factors for PHLF [58].Bleeding can lead to coagulopathy [59],hypotension and fluid shift during major hepatectomy [60].Inflammatory and immune modulation effect of blood transfusion can further contribute to PHLF [61].Sepsis and major bile leak can have significant impact on liver regeneration and contribute to hepatic insufficiency [62,63].Surgical dissection technique,although less well established,can contribute especially with inferior vena cava repair and excessive dissection around portal triad [64].Pringle manoeuver can result in ischemia-reperfusion injury,which is linked to PHLF [65].However,in centers adopting routine Pringle,blood loss is a more significant predictor for PHLF [66].Noteworthy,intermittent clamping appears to be better tolerated than continuous clamping and is linked to improved outcomes and shorter hospital stay [67].Prolonged operative time is considered a risk factor by some authors [68].
It is perceived that resections involving the right lobe are more prone to complications [69].This could be attributed to many factors,including the smaller left liver remnant.There is a wide acceptance for laparoscopic resection especially for minor hepatectomies and peripherally situated lesions which had less postoperative morbidities [70]and less frequent postoperative decompensation and ascites in cirrhotic patients [71],however,its benefits in major or more complex resections are still not clear.
Liver related factors
Quality and quantity of future liver remnant (FLR) are key determinants of postoperative liver regeneration.Functional and volumetric assessment of the liver is therefore critical in hepatectomy planning.
Volume assessment
There is a consensus that an FLR of 20% total liver volume is required to avoid PHLF in a healthy liver,more than 30% for patients with hepatotoxic chemotherapy and over 40% for cirrhotic patients [72].FLR volume can be calculated based on the standardized total liver volume which can either be compared with body weight or body surface area [33,73].There have been several formulas on calculations of the total and future liver volume [72,74–76].The method of calculation of the liver volume is clinically relevant.Measuring the volume is far superior to estimation.Measurement allows far more accurate predictions of postoperative risk of PHLF [77].However,these calculations may not be reproducible in different populations [78].
Previously,CT volumetric was two-dimensional and a poor predictor of outcome,however,newer three-dimensional CT and MRI accurately predict the liver volumes [79].Both MRI and CT based volume measurements can be used interchangeably [80].MRI has been used to simultaneously assess volume,function,and successfully predict postoperative outcomes,including PHLF [81].
One of the technical tips observed is that the slice thickness in image acquisition could influence the accuracy of volume calculations [82].A correction factor for the intrahepatic blood volume might be required to improve the prediction of the clinical outcome [83].Other tools,such as ultrasonography-based volume assessment was found comparable to the most widely accepted CT volumetric assessment [84].
Functional assessment
Indocyanine green (ICG) clearance rate is a widely used method of assessing liver function [85].ICG clearance is measured 15 min(ICG-15) from injecting the water-soluble cyanine dye.In healthy livers,90% of the dye will be hepatically cleared,while less than 60% cleared suggests poor liver function and risk of PHLF [74].Whilst it gives a measurement of total liver function,it is not specific to FLR functionality [86].Kim et al.[74]found that the FLR volume is a predictor of PHLF regardless to ICG retention in patients without cirrhosis.For patients with cirrhosis,a ratio of FLR:ICG-15 >1.9 had 100% specificity in predicting PHLF [74].
Other studies looked at radioactive measurement of liver function using analogues such as99mTc-iminodiacetic acid for scintigraphy [87,88].This allows measurement of distribution of functional hepatocytes;however,it can give spurious results and over predict regeneration as any hepatocyte with an intact membrane can give a signal.de Graaf et al.[89]found functional assessment of the liver was superior as it could reduce the interval between imaging and resection compared to standard CT imaging.In a small study of 29 patients using Gd-EOB-enhanced MRI,Cho et al.[90]found Gd-EOB-enhanced MRI could predict PHLF with a sensitivity of 85.7%and specificity of 77.3% which was superior when compared to ICG,and this finding has been reported in other studies,however,all have a small sample size [91–93].
Quality of liver parenchyma
Liver parenchyma compliance can be defined as the accommodative response of the liver in response to change in blood volume [94].Liver compliance is a product of liver parenchymal and vascular quality and elasticity,and it can predict the occurrence of PHLF [95].Rajakannu et al.[96]designated liver stiffness measurement the only predictive marker of postoperative liver decompensation.They suggested assessing transient elastography should be compulsory before hepatectomy,ideally within 2 weeks,and 22 kPa is the “cut-off” for patients pre-hepatectomy with hepatocellular carcinoma.The addition of spleen volumetry with a cut-off point of 381.1 cm3will increase the accuracy in predicting posthepatectomy decompensation [97].Portal vein velocity was a sensitive and specific predictor of PHLF,as a surrogate for hepatic resistance.Salman et al.[98]showed portal vein velocity was significantly higher in those that developed PHLF.
It was long perceived that steatosis is a major risk for liver failure [99,100].An experimental study has shown the impact of severe steatosis without inflammation on the hepatic resistance and hemodynamic parameters [101].A large meta-analysis suggested an adverse impact of steatosis on the outcome of liver surgery but without distinction between steatohepatitis and steatosis [102].Steatosisperse(without inflammation) has not been correlated to major,but minor complications after hepatectomy [103].In a small study of 37 patients,there was a higher rate of infection after resection in patients with steatosis compared to the control group [104].These findings were confirmed in a larger study with >300 patients,with increased complications with marked steatosis [105].Steatohepatitis was found to influence the outcome post-hepatectomy [105,106].While most pretreatment regimens for metastatic cancer were associated with steatosis [105],steatohepatitis was linked to irinotecan [107].Steatohepatitis can occur with as little steatosis as 5% [108].Potentially previous classifications based on the amount of steatosis is clinically irrelevant [99].Unfortunately,no reliable marker for steatohepatitis is available [109,110]and biopsy remains the gold standard [111].Assessment of steatosis,on the other hand,can be achieved noninvasively using elastography with an area under the curve of up to 0.89 [112].
Hepatotoxicity is common after chemotherapy [113].Derangement in liver functions is the most common indicator of hepatotoxicity [114].If not all,many of the chemotherapy regimens indicated in the context of liver metastasis are hepatotoxic [114].The detailed influence of the individual agents on the liver is not the subject of this review.Prolonged chemotherapy was associated with increased morbidity [115,116].This is particularly related to the extent of hepatectomy and the intraoperative blood loss [117].Whilst the larger body of literature connect chemotherapy to postresection complications,some as in Fahy et al.[117]suggested that there is no major impact of the preoperative chemotherapy on PHLF.Hubert and coworkers [118]found that chemotherapy before operation is significantly associated to sinusoidal congestion without any significant impact on postoperative clinical outcome.
Remarkably,the prevalence of liver metastasis in the presence of liver cirrhosis was previously underestimated [119].Hepatectomy for secondary lesions on cirrhosis is associated with increased mortality [120].The hepatocyte growth factor administration demonstrated effectiveness in hepatocyte regeneration in cirrhotic rats that underwent hepatectomy [121,122].
Cholestasis inhibits the genes responsible for early liver regeneration [123]and induces ischemia-reperfusion injury and reduced antioxidants leading to inflammation [124].The current literature suggests that preoperative jaundice may contribute to PHLF [125,126].Interestingly,measuring a daily bilirubin level of 56 mg/d in the drained FLR could be a useful indicator of poor outcome and PHLF [127].
Risk modification: preventions and interventions
Due to substantial risk of mortality and minimal treatment options,the focus is on prevention of PHLF.Risk modification is directed to modifiable factors with efforts to preserve liver functions,minimize the effect of contributing factors and supportive measures for liver failure.In the above-mentioned sections,there are highlights of different known risk factors.Herein,this review summarizes the documented mitigation of the modifiable risk factors.
Modifying patient and systemic related risks
Patient related risk modifications include intense glycemic control and protection of liver function post-hepatectomy [128].Improving the performance status through a limited prehabilitation program was linked to improving the outocmes after liver surgery [129].Although the published studies have not addressed specifically PHLF,improvement in outcomes is expected to reflect on the decrease of PHLF indicence,particularly early grades.In additon,energy efficiency was observed at the level of the liver tissue [130].
High body mass index was linked to adverse outcomes after liver surgery [36,131–135].Whilst surgically induced weight loss resulted in improvement in liver morphology and inflammation [136],aggressive weight loss interventions have been associated with liver dysfunction in patients not undergoing liver surgery [137].Lifestyle induced weight loss has a perceived benefit prior to non-liver surgery but is not associated with improvement in outcomes [137].We have not identified dedicated studies on the value of weight loss in the context of hepatectomy.However,a meta-analysis has shown histological improvement of liver morphology following bariatric surgery [138].Interpreting this in the context of preparing for surgery for secondary liver cancer,where the patient has undergone many treatment phases,including surgical ones,is challenging.It appears that the most applicable strategy to address this risk would be enrolment to prehabilitation programs,which showed promise in improving the oxygen utilization [139]and outcome of patients undergoing hepatectomy [140].
Manipulation of the gut microbiome seemed to influence the course of liver regeneration suggesting different pathophysiological mechanisms [141].The chemical alteration of the gut microbiota appeared to reduce serum zonulin levels and plasma endotoxins [142].This may explain why half of the patients die with manifestations of sepsis [14].
Modifying the technical and liver related risks
Currently,strategies against post-chemotherapy induced liver injury are limited to volume manipulation and time to recovery after chemotherapy.Prevention of chemotherapy induced steatohepatitis might be possible using S-adenosyl methionine compounds [143]as well as tiopronin [144].Ischemic preconditioning was associated with reduction of necrosis where total vascular exclusion is applied [145].Mild steatohepatitis is potentially reversible with a simple lifestyle intervention [146].
Pharmacological options like insulin sensitizer and vitamin E were found helpful in reducing the inflammation associated with steatohepatitis [147].Vitamin E and pioglitazone have been proposed in the context of reducing further risk of hepatocellular carcinoma development on nonalcoholic steatohepatitis [148].Caloric restriction also showed benefit in reversal of steatohepatitis but again not in the context of hepatectomy [149].High protein diets were useful in reversal of steatosis in short duration [150].Phosphate balance is an important issue in post-hepatectomy period as hypophosphatemia after a hepatectomy suggests liver regeneration.Elevated phosphorus levels (>2.4 mg/dL) in POD2 is a poor prognostic sign and is associated with increased postoperative complications,hepatic insufficiency and death [151].Table 1 summarizes these risk factors along with the best available evidence of modification [2,6,9,26,36,47–52,55,72,73,95,96,104–107,109–111,113,114,117–122,128,129,131–135,143,144,146,147,152–182].

Despite some authors reporting no difference in preoperative biliary drainage of jaundiced patients,Cherqui et al.reported an incidence of PHLF 5% in not drained versus 0 in drained patients [183].At present,a larger number of studies advocate preoperative drainage of jaundice to reduce PHLF.
The decision to operate has significantly been facilitated with the utilization of chemotherapy [184].However,a delay of 5-8 weeks between chemotherapy and surgery was shown to reduce the perioperative side effects [185].Many of the surgery related risks are modifiable.Blood loss could be reduced using low caloric diet which may reduce steatosis [153].Also,low central venous pressure reduced the blood loss during partial hepatectomy [186].Stapler based parenchyma transection could reduce the operative time although its safety is questionable among large sector of liver surgeons [187].Pringle maneuver was not linked to clinically significant grade B/C PHLF,but to non-clinically significant PHLF [188]and to postoperative complications [189].It was also linked to ischemia-reperfusion injury [65]but ischemic preconditioning was not found effective in clinical practice [190–192]except in post-chemotherapy livers undergoing total vascular exclusion,where it was protective [145].
The concept of staged resection was introduced to allow an interval regeneration of the FLR [193].The two-stage procedure (TSP)aims at allowing the FLR to grow sufficiently to prevent PHLF when definitive resection is performed.The major concept behind the TSP is manipulation of the FLR volume.TSP could include only vascular intervention such as portal vein embolization or ligation.The portal vein embolization and/or ligation are usually performed as part of the TSP and are directed towards diverting the inductive portal flow to the FLR to stimulate hypertrophy [194].Portal vein ligation is generally performed earlier than portal vein embolization,at around 5-8 weeks preoperatively,whereas portal vein embolization is performed 3-6 weeks prior to operation.This could be explained by the effect of vascularization of the distal portal branches on the atrophy hypertrophy complex [195].Liver venous deprivation showed more rapid growth of FLR with similar rates of morbidity and mortality in comparison to portal vein embolization [196].
Interestingly,other vascular interventions such as splenic embolization or ligation,or portosystemic shunt,or partial reduction of portal flow are performed to alleviate excessive portal flow from the FLR that would have otherwise induced barotrauma [29,197].Splenic artery ligation showed higher rates of mitosis 72 h post-hepatectomy,which may account for the reduction of oxidative stress secondary to the reduction of traumatic portal flow to the FLR [198].The vascular embolization,whether splenic artery or portal vein,is often done as part of the TSP.Similarly,the portal vein ligation could be part of the TSP,while ligation is often performed at the time of the definitive hepatectomy.
TSP concept also includes parenchymal maneuvers as in the classic two-stage hepatectomy,where clearance of the remnant is performed alongside portal vein ligation [199]or embolization [193].A newer modification including parenchymal transection (associating liver partition and portal vein ligation for staged hepatectomy,ALPPS),whether partial or complete,has drawn large attention over the past years due to enhanced volume gain feature [200,201].
Apart from the aforementioned procedures,most of the first stage of the TSP are performed at several weeks prior to resection depending on the kinetics of FLR volume growth [2,202,203].ALPPS procedure was initially heralded as revolutionary due to impressive rates of hypertrophy in the first week after procedure with growth of up to 35 mL/d [204,205].Often this is not possible in portal vein embolization alone,and up to 40% of patients may be irresectable post portal vein embolization due to tumor progression [183].This was predominantly to ensure volume gain,however,recently volume gain is found disproportionate to functional recovery [206,207]and longer waits could be preferable [200].
Medications directed to enhancing regeneration could have value in preventing the PHLF
Petrowsky et al.[18]showed that pentoxifylline was associated with 3.6 times increase in production of interleukin 6 (IL-6) which in turn associated with accelerated liver volume gain and reduced liver injury [208].The effect is more pronounced as early as in the first postoperative day [209].However,there were more complications in the pentoxifylline group caused by drug related side effects.Preoperative administration of olprinone,a selective phosphodiesterase III inhibitor at a concentration of 10 ng/mL(not 20 ng/mL) reduced platelet aggregation,sinusoidal plugging,and upregulated endothelial nitric oxide synthase resulting in reduction of portal venous pressure to a level that prevented subsequent PHLF [210].
Granulocyte-colony stimulating factor (G-CSF) has been explored as a means of reducing hepatic congestion [211].Those treated with G-CSF perioperatively showed markedly improved velocity of mitosis which in turn hastened the cell cycle [211].Ji et al.[212]found G-CSF had a positive impact on post-hepatectomy survival.Whilst stem cell therapy did appear an attractive option at increasing liver regeneration,it has not been found to be effective at treating those with PHLF [213];perhaps this could be explained by pathogenesis of PHLF and problems of reaching appropriate functioning cell numbers,rather than merely increasing the number of cells within the liver.Drugs like NIM811,significantly reduced the incidence of PHLF in mice via reducing mitochondrial dysfunction and optimizing proapoptotic cytochrome-c release [214].
Other medications to modulate splanchnic flow such as splanchnic vasoconstrictors propranolol,somatostatin and terlipressin were tested by Kim et al.[215].Through comparing these drugs after hepatectomy against control,these medications were found to significantly decrease portal pressure.Out of all the groups,terlipressin was statistically associated with improved survival [216].Propranolol,a non-selective betablocker,causes hypotension,which will be exacerbated in patient post-hepatectomy [217]and arrest hepatocyte cell division impairing hepatocyte regeneration [218].Whilst it may appear counterintuitive to arrest regeneration,if there is too quick and too much regeneration,the remnant liver becomes functionally smaller with associated increased portal pressure.By halting regeneration,there may be a way to manipulate regeneration so that is occurs at an acceptable rate.Table 2 summarizes how the interventions act to prevent PHLF [15,17–24,27,31,75,162,170,171,198,200,203,209-212,214–216,218–240].Fig.2 summarizes the available interventions in a timeline around the definitive hepatectomy.
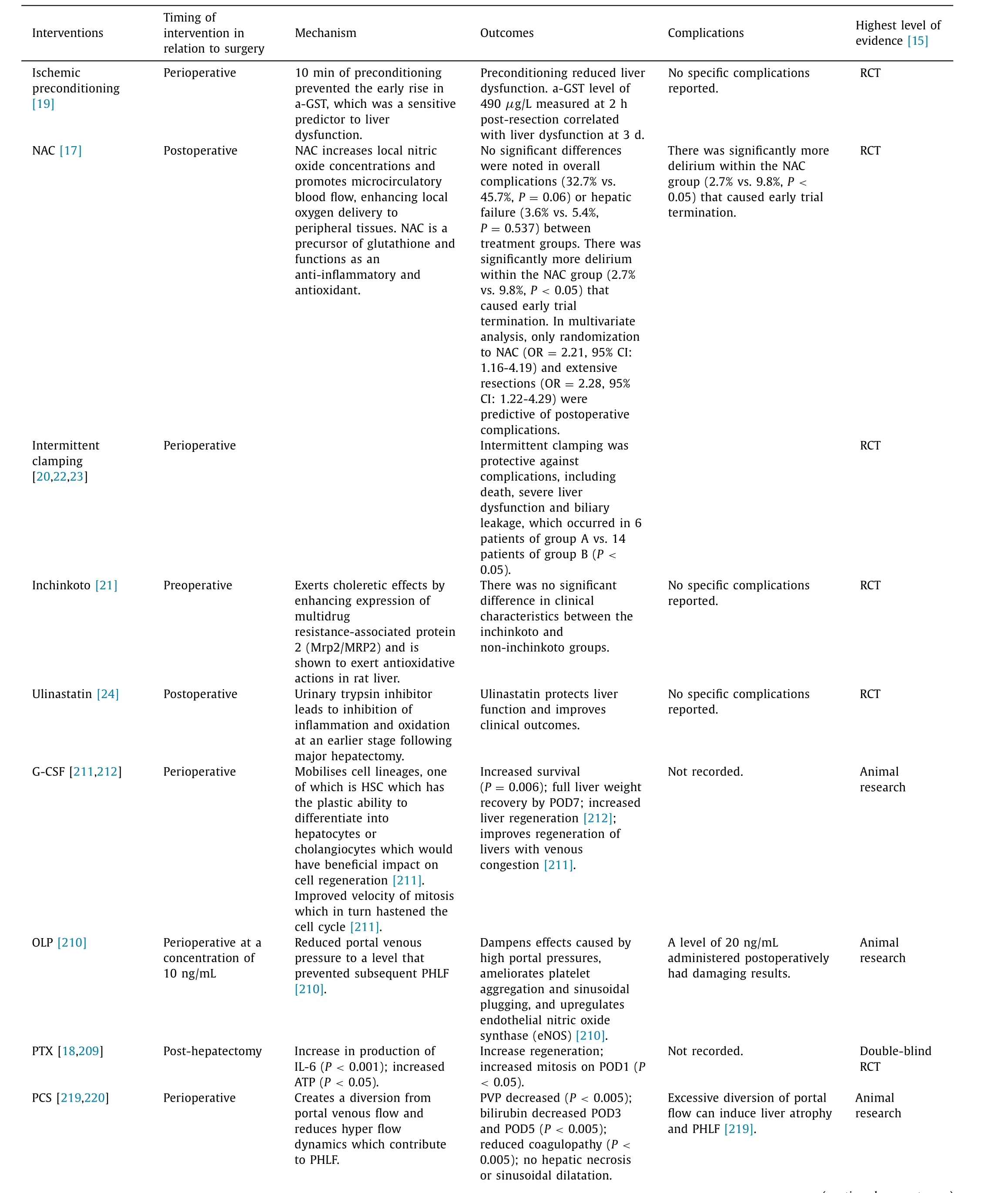
Table 2Interventions to prevent PHLF and their best available evidence.
Treatment
PHLF remains a difficult and important obstacle in the treatment of both primary and secondary liver tumors.Despite the wealth of literature there is no consensus as to how PHLF develops and whether perioperative techniques hold the elixir to avoid often fatal complications.Unfortunately,once PHLF develops,there is often little that can be done other than best supportive care measures,or liver transplant.
Establishing risk criteria of a patient developing PHLF can help predict and prevent potential complications.Accepted diagnostic criteria iterate progressive hyperbilirubinemia on POD5 as a positive predictor of mortality [10].Low C-reactive protein on POD1 was found to predict sepsis and subsequent mortality,and it is expected initial poor hepatic synthetic function heavily impacts prognosis [241].Careful monitoring of patient’s electrolytes,fluid balance,liver function,and coagulation is important.Prompt correction of derangement may improve patient outcomes [12,242].Management will aim to correct organ dysfunction as per standard treatment,and application of devices such as molecular absorbent recirculating system may be required [242].Evidence for such therapies in patients with PHLF has not been established.Patients who develop severe PHLF are likely to require liver transplantation,and national criteria for transplantation should be applied [242–244],otherwise,death remains an expected outcome [11,245].Table 3 describes manifestations of the PHLF and their management [9,12,14,93,242,246–250].

Table 3Manifestations of the PHLF,their management and the best available evidence.
Future directions
Indication of surgery for liver metastasis has evolved over decades from considering it as contraindication to surgery to proposing cure [251].Similarly,indications for liver transplantation are evolving and it is offered in some countries for unresectable colorectal liver metastases resulting in the longest survival [252].In addition,it could be a lifesaving option for patients with irreversible PHLF [253].The major concern related to this is the organ paucity and the current allocation system that prioritizes patients with end-stage liver disease or primary liver cancer.Addressing this concern,techniques that maximize organ use like split liver transplant and auxiliary liver transplant could be considered.There is evidence from animal model that auxiliary partial transplant alleviated symptoms of PHLF and reduced fatality [254].A relatively new technique was described in those lines with partial resection and small volume partial liver transplant takes place followed by a delayed hepatectomy,known as the RAPID concept,has produced encouraging results albeit the complexity of the procedure [255].Medical interventions such as carbamazepine,olprinone,leucine-serine-lysine-leucine,propranolol,and terlipressin have shown promise,but require robust research into their clinical application.Novel methods to modulate portal flow such as adjustable vascular band and portocaval shunting again are promising,but require validation.
In summary,the available evidence is of low quality and there is a significant knowledge gap in this area.Preventative measures are the mainstay of intervention,and volume manipulation is the most widely used approach to prevent PHLF.Transplant is the only“cure” treatment.
Acknowledgments
The authors acknowledge Mr.Wai-Lum Sung from the Medical Illustration Department,University of Aberdeen in the realization of the graph.
CRediTauthorshipcontributionstatement
MohamedBekheit: Conceptualization,Data curation,Investigation,Writing -original draft,Writing -review &editing.Lisa Grundy: Data curation,Investigation,Writing -original draft.AhmedKASalih: Data curation,Investigation,Writing -original draft.PetruBucur: Writing -review &editing.EricVibert: Writing -review &editing.MudassarGhazanfar: Writing -review &editing.
Funding
None.
Ethicalapproval
Not needed.
Competinginterest
No benefits in any form have been received or will be received from a commercial party related directly or indirectly to the subject of this article.
Supplementarymaterials
Supplementary material associated with this article can be found,in the online version,at doi:10.1016/j.hbpd.2023.03.001.
杂志排行
Hepatobiliary & Pancreatic Diseases International的其它文章
- A new prognostic model for drug-induced liver injury especially suitable for Chinese population
- INSTRUCTIONS FOR AUTHORS
- Value and prognostic factors of repeat hepatectomy for recurrent colorectal liver metastasis
- Older liver grafts from donation after circulatory death are associated with impaired survival and higher incidence of biliarynon-anastomotic structure
- Development and validation of a novel model to predict liver-related mortality in patients with idiosyncratic drug-induced liver injury
- Clinical-radiomics predictors to identify the suitability of transarterial chemoembolization treatment in intermediate-stage hepatocellular carcinoma: A multicenter study