Effects of infrared CO2 laser moxibustion on patients with knee osteoarthritis: a double-blind,randomized, controlled study
2023-12-25XUJingwen徐靖雯SHENXueyong沈雪勇DENGHaiping邓海平CHENGKe程珂WUFan吴凡ZHAOLing赵玲
XU Jingwen (徐靖雯), SHEN Xueyong (沈雪勇),2,3, DENG Haiping (邓海平),2, CHENG Ke (程珂),2, WU Fan (吴凡),ZHAO Ling (赵玲)
1 Acupuncture and Tuina School, Shanghai University of Traditional Chinese Medicine, Shanghai 201203, China
2 Shanghai Research Center of Acupuncture & Meridian, Shanghai 201203, China
3 Shanghai Key Laboratory of Acupuncture Mechanism and Acupoint Function, Fudan University, Shanghai 200433, China
Abstract
Keywords: Osteoarthritis, Knee; Laser Therapy; Acupoint Therapy; Point, Dubi (ST35); Randomized Controlled Trial
Osteoarthritis (OA), a disabling joint disease, is the most prevalent form of arthritis among people aged 60 years or older in the United States[1-2], and the knee joint is the most commonly affected[3].The prevalence rate of knee osteoarthritis (KOA) increases with age and presents an almost linear growth after 40 years of age in China[4-5].Currently, OA’s treatments focus on alleviating pain and maintaining or improving joint function and quality of life[6].
Traditional moxibustion therapy, known for its warming effects mainly achieved by thermal radiation generated by burning moxa, has been widely used to treat KOA in clinics in China[7-9].However, the irritating smoke and odor produced by traditional moxibustion therapy are detrimental to the health of physicians and patients[10].Previously, our group’s research showed that specific wavelengths of infrared radiation produced by moxibustion are equally important as the generated thermal radiation.We also found that the wavelength of human acupuncture points is approximately 10 μm[11], which is coincidental with that of traditional moxibustion infrared radiation.Therefore, we supposed that a resonance between the burning moxa and the human body might explain the mechanism of traditional moxibustion.We have developed a laser moxibustion device of 10.6 μm wavelength, which has the thermal nature of moxibustion without smoke and smell.This wavelength can be easily absorbed by biological tissue to produce potent superficial and nonpenetrating heat and can be used as a proxy for traditional moxibustion.The purpose of this clinical trial was to determine whether CO2laser moxibustion can improve joint pain, stiffness, and functional activities in patients with KOA by comparing its efficacy with that of sham treatment.
1 Materials and Methods
1.1 Trial design
Our study was a double-blind, randomized, and controlled clinical trial with a 4-week follow-up.Allocation concealment was ensured with disguised letter codes of the laser moxibustion devices (either active or sham devices) that were generated and sent to the site coordinators via a central randomization system.After receiving the device code from the site coordinator, the device operator used the laser moxibustion device labeled with that code for treatment.The operators were unaware of the active or sham device as both produced the same red light.The whole procedure was supervised by the coordinators to ensure that the protocol was followed.Participants in the two groups were treated by trained operators.Communication among participants was discouraged and avoided as they were treated in separate rooms.Therefore, all involved personnel, including participants,device operators, outcome assessors, research coordinators, and statisticians, were blinded to the treatment allocation.The entire trial was conducted in Longbai Community Health Center of Minhang District,Shanghai.Our study protocol was approved by the Institutional Review Board of Shuguang Hospital,Shanghai University of Traditional Chinese Medicine,and all included patients gave informed consent.
1.2 Patient recruitment
We recruited voluntary participants by screening all residents within a 3 km radius of the hospital.During their first visits to the hospital, the patients received an X-ray examination of the anteroposterior and lateral view of the knee.The function of knee joints was examined by an orthopedist who decided whether the patients met the inclusion criteria.Patients were required to understand the questions asked in standard Mandarin and properly respond.
1.3 Diagnostic criteria
According to the KOA diagnostic criteria of the American College of Rheumatology[12-13], key diagnostic points included radiographic confirmation of KOA(Kallgren-Lawrence grade Ⅱ or Ⅲ)[14-15], moderate or greater clinically significant knee pain on most days of the past month, and the subject’s visual analog scale baseline score for arthritic pain was 40 points or above.
1.4 Inclusion criteria
Met the diagnostic criteria for KOA; aged 50 years or older, male or female; must not have had acupuncture or moxibustion treatment in the last 3 months; willing to be randomly assigned, and understood and signed the informed consent.
1.5 Exclusion criteria
Patients were diagnosed with inflammatory arthritis,gout, acute knee joint injury, other knee arthritis(without cartilage involvement), meniscus injury,ligament injury, or intra-articular fracture; patients with serious heart, kidney, or liver diseases, or malignant tumors (unless the patient was surgically treated, and had no relapse for more than 5 years), systemic infections, or contagious diseases; patients receiving intra-articular corticosteroid or hyaluronate injections,or any knee surgery or topical use of medication in the latest 6 months, or previous history of knee surgery;patients with previous experience with drug tests.
1.6 Criteria for discontinuing and elimination
Patients were withdrawn from the study if they had serious adverse effects during the treatment or took a treatment deviating from the plan.Patients were also withdrawn if any other treatments were used during the trial that might potentially interfer with the assessment of the effects or if consent was withdrawn.
1.7 Randomization and blinding method
Block randomization was used for group allocation.The distribution list with sequence numbers, random numbers, block numbers, and group allocation marks were kept by two researchers: one was for group randomization, and the other was not used for the study.Neither researcher was involved in the clinical trial after randomization.The participants were screened and recruited according to the inclusion criteria by the researchers responsible for recruitment and were given sequence numbers and group allocation marks based on their visiting sequence.All information,including names, sequence numbers, and group allocation marks, was recorded and kept by the recruiter.Treatment providers were only responsible for providing treatment with the laser device indicated by the participant’s group allocation marks.Treatment providers recorded the details for each treatment, but they were not allowed to answer any questions asked by the participants.Case report forms, 50-yard walking test time, and related questions were completed by the recruiters.None of the research staff or participants were aware of group allocation until unblinding after trial completion.The CO2laser moxibustion device and the sham device used in the trial were manufactured by the same company.The two devices were exactly the same in appearance, body mass, and operational procedures, except for their group allocation marks.The treatment providers switched on each device in accordance with the participant’s group allocation marks.
1.8 Laser moxibustion device
The SX10-C1 CO2laser moxibustion device was manufactured by Shanghai Wonderful Opto-Electrics Tech.Co., Ltd., China.The CO2laser generates a 10.6 μm infrared light with output power ranging from 50 mW to 300 mW.The sham device was identical to the CO2laser device in appearance, body mass, and operational procedures but with no laser output.
1.9 Treatment time and methods
Participants were supine with exposed knees that were slightly flexed and supported by a pillow.The laser tip was placed perpendicularly above the skin of Dubi(ST35).The indicator light was turned off when the treatment started.In the CO2laser moxibustion group,the diameter of the laser beam passing through a defocusing probe on the skin was 2 cm.The skin was irradiated by a laser output of 200-220 mW (with the highest energy at the center of the irradiated area).The sham laser moxibustion group was operated in the same way but without laser output.Each treatment session lasted 20 min, 3 times a week, for a total of 12 treatments in 4 weeks.
1.10 Outcome measures
1.10.1 Primary outcome measures
The Western Ontario and McMaster Universities osteoarthritis index (WOMAC) questionnaire was used to assess the therapeutic effects by recording measures of joint pain, stiffness, and functional disorder after 2 weeks and 4 weeks of treatments.The long-term effects were also assessed 4 weeks after treatment.
1.10.2 Secondary outcome measures
The 50-yard (1 yard is equal to 0.914 m) walking time was assessed and recorded among the participants after 2 weeks and 4 weeks of treatments, and 4 weeks after treatment to observe possible improvements in walking.Adverse effects reported by the participants were recorded during treatment.Serious adverse effects were reported to the Institutional Review Board of Shuguang Hospital, Shanghai University of Traditional Chinese Medicine.At the follow-up, we asked participants to assess therapeutic effects and guess their group assignment to evaluate trial masking effectiveness.Additionally, the participants were asked whether they thought the treatment was safe.
1.11 Estimation of sample size
Before conducting the formal trial, we completed a pilot clinical observation with a small sample size (n=22).We determined the sample size (n=160) using PASS software (NCSS, LLC, USA) with the following conditions,α=0.05 and 1-β=0.80, by taking the mean and the standard deviation of two groups’ WOMAC total scores at the end of the treatment session as variables.
1.12 Statistical methods
Statistical analysis was performed using SPSS version 25.0 software (IBM, USA).All measurement data were expressed as mean ± standard deviation (when following a normal distribution; otherwise, median(lower quartile, upper quartile) [M (QL, QU)] was used.And those data were recorded by three graduate students who were not involved in the trial.The three copies of the data were verified by a self-designed program.Two-sample t-test or Mann-Whitney U test was used for the WOMAC scores at baseline (week 0) to evaluate statistically significant differences in the distribution of different variables at baseline according to whether the data were normally distributed.Mann-Whitney U test was performed for the ranked data,WOMAC scores, and the 50-yard walking time at the same time points.The differences were considered significant when P<0.05.
2 Results
2.1 Participants recruitment
The trial recruited and treated participants between August 2013 and July 2015.There were 223 participants recruited and 45 excluded (Figure 1), among which 36(80.0%) were excluded because of insufficient pain, 6(13.3%) for no radiographic evidence of osteophyte, and 3 were diagnosed with other knee diseases.After randomization of 178 eligible patients, 5 participants withdrew from the treatment, among which 3 withdrew in the first 2 weeks of treatment and the remaining 2 in the second to fourth weeks.Four (90.0%)of the withdrawn participants were in the CO2laser moxibustion group, and 1 (10.0%) was in the sham laser moxibustion group.All withdrawals were because of personal reasons irrelevant to the trial.Finally, 173 participants completed the trial, but 3 were lost to follow-up: 1 case in the CO2laser moxibustion group and 2 cases in the sham CO2laser moxibustion group.Later telephone contact revealed that the 2 participants in the sham laser moxibustion group were hospitalized because of accidental falls, and the one in the CO2laser moxibustion group was abroad visiting relatives.
Among the eligible cases, 78.7% were female, and 68.0% of the cases were above 60 years old.Before treatment, there were no statistically significant differences between the CO2laser moxibustion and the sham laser moxibustion groups in gender, age, body mass index (BMI), affected joints, or disease course,which suggests that the two groups are comparable at baseline (Table 1).

Table 1 Participant demographics
2.2 WOMAC scores
Before treatment, there was no significant difference between the two groups in three major outcome measurements: pain, stiffness, and functional disorders based on WOMAC scores.During the trial, all three WOMAC scores of both groups improved significantly(P<0.001), in a linear relationship with treatment progression.However, the CO2laser moxibustion group had a significantly greater improvement than the sham laser moxibustion group (P<0.05).The WOMAC score improvement in participants treated by CO2laser moxibustion was superior to those by the sham laser moxibustion at each assessment through the trial(Table 2).
Table 2 Mean changes from baseline in WOMAC outcomes ()/[M (QL, QU)] Unit: point
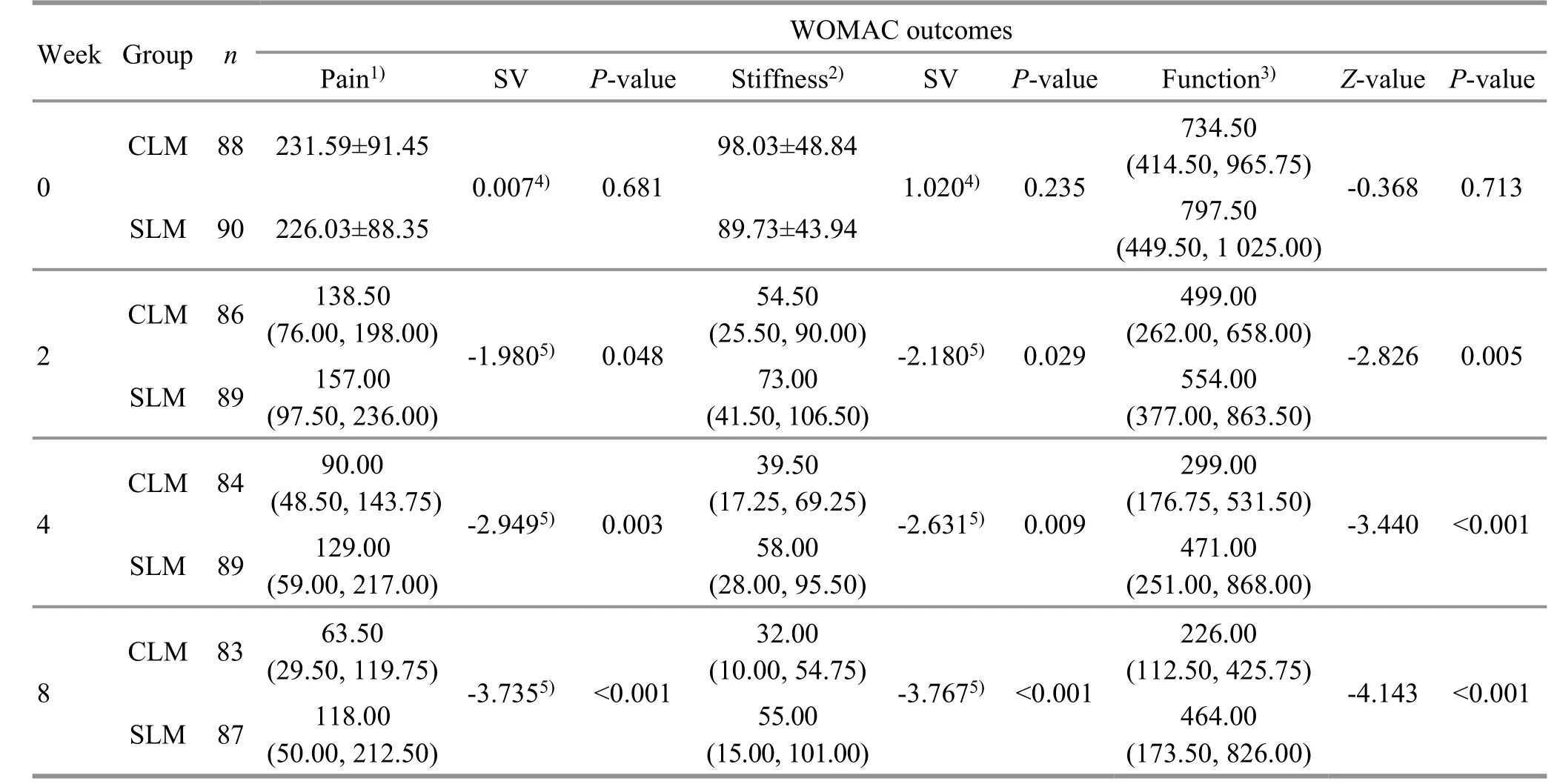
Table 2 Mean changes from baseline in WOMAC outcomes ()/[M (QL, QU)] Unit: point
Note: WOMAC=Western Ontario and McMaster Universities osteoarthritis index; SV=Statistical value; CLM=CO2 laser moxibustion; SLM=Sham laser moxibustion; 1) ranges from 0 to 500 points; 2) ranges from 0 to 200 points; 3) ranges from 0 to 1700 points; 4) t-value; 5) Z-value.
Week Group n WOMAC outcomes Pain1) SV P-value Stiffness2) SV P-value Function3) Z-value P-value 0 CLM 88 231.59±91.45 98.03±48.84 0.0074) 0.681 1.0204) 0.235 734.50(414.50, 965.75) -0.368 0.713 SLM 90 226.03±88.35 89.73±43.94 797.50(449.50, 1 025.00)2 4 CLM 86 138.50(76.00, 198.00) -1.9805) 0.048 SLM 89 157.00(97.50, 236.00)CLM 84 90.00(48.50, 143.75) -2.9495) 0.003 SLM 89 129.00(59.00, 217.00)54.50(25.50, 90.00) -2.1805) 0.029 73.00(41.50, 106.50)39.50(17.25, 69.25) -2.6315) 0.009 58.00(28.00, 95.50)499.00(262.00, 658.00) -2.826 0.005 554.00(377.00, 863.50)299.00(176.75, 531.50) -3.440 <0.001 471.00(251.00, 868.00)8 CLM 83 63.50(29.50, 119.75) -3.7355) <0.001 SLM 87 118.00(50.00, 212.50)32.00(10.00, 54.75) -3.7675) <0.001 55.00(15.00, 101.00)226.00(112.50, 425.75) -4.143 <0.001 464.00(173.50, 826.00)
2.2.1 Pain
After 2 weeks of treatments, the WOMAC pain score decreased by 33% in the CO2laser moxibustion group,which was significantly better than that in the sham laser moxibustion group (P<0.05).By the end of the treatment, the WOMAC pain score decreased 48% in the CO2laser moxibustion group, which was significantly better than that in the sham laser moxibustion group (P<0.05).The difference in pain improvement between the two groups continued until the end of the follow-up at the 8th week (P<0.05).See Table 2.
2.2.2 Stiffness
After 2 weeks of treatments, the WOMAC stiffness score decreased more in the CO2laser moxibustion group than in the sham laser moxibustion group(P<0.05).By the end of the treatment, the WOMAC stiffness score decreased by 42% in the CO2laser moxibustion group, which was significantly greater than that in the sham laser moxibustion group (P<0.05).The difference was significant until the end of the follow-up at the 8th week (P<0.001).See Table 2.
2.2.3 Functional disorders
WOMAC functional disorder scores were significantly lower in the CO2laser moxibustion group than in the sham laser moxibustion group after 2 weeks and 4 weeks of treatments and at the follow-up (P<0.05).At the end of treatment and follow-up, WOMAC functional disorder scores in the CO2laser moxibustion group decreased by 41% and 56%, respectively.See Table 2.
2.3 50-yard walking time
Before treatment, there was no significant difference in the 50-yard walking time between the two groups(P>0.05).During treatment, 50-yard walking time in both groups decreased with a similar tendency compared with the baseline.In the CLM group, the 50-yard walking time at weeks 2, 4, and 8 was significantly reduced compared with before treatment, and the Z-values are -4.969, -5.889, and -5.795, respectively(P<0.05).In the sham laser moxibustion group, the 50-yard walking time at weeks 2, 4, and 8 was reduced compared with before treatment, and the Z-values are-2.295, -2.373, and -3.447, respectively (P<0.05).There was no significant difference in 50-yard walking time between the two groups at each assessment of the trial(P>0.05).See Table 3.
2.4 Participant self-assessment
At the follow-up, the participants were asked to selfassess the treatment they received.Compared with the sham laser moxibustion group (43%), more participants in the CO2laser moxibustion group (64%) thought their treatments were more effective (P<0.001).
2.5 Masking effectiveness
We asked the participants to guess their group assignment at the final follow-up to assess masking effectiveness.The results showed that most participants were uncertain about their group assignment, and there was no statistical difference between the two groups (P>0.05).Because 165 of the participants (97%) were uncertain about their group assignment, we believed that the results of the primary outcome measurements were not influenced by participants guessing their group assignment.
2.6 Safety evaluation
Among the 178 participants, 73 participants (88.0%)in the CO2laser moxibustion group reported a postmoxibustion reaction, while only 3 (3.5%) in the sham laser moxibustion group reported reactions (Table 4).Skin flushing on the irradiated site occurred in 23.3% of the 73 post-moxibustion reactions in the CO2laser moxibustion group.Blistering occurred in 75.3% of the reported adverse events in the same group.This local skin injury was induced by the thermal effects of CO2laser moxibustion.One participant reported slight festering after local skin blistering.The wound healed quickly after the application of topical antibacterial medication.There were 2 participants in the sham laser moxibustion group who reported likely local skin flushing after treatment, and 1 participant reported that his joint stiffness symptom was aggravated after 8 treatments.
Participants were asked to evaluate the safety of the treatment at the final follow-up (Table 5).Although most participants in the laser group reported reactions such as blistering after treatment, none considered these effects to be serious adverse events.In the sham laser moxibustion group, 86 participants (98.9%)thought the treatment was very safe or comparatively safe, and one participant regarded aggravation of joint stiffness as a slight post-moxibustion reaction effect caused by the treatment (P>0.05).

Week Group n 50-yard walking time/s Z-value P-value 0 CO2 laser moxibustion 88 34.655 0 (31.592 5, 38.352 5) -0.300 0.764 Sham laser moxibustion 90 35.355 0 (30.675 0, 39.765 0)2 CO2 laser moxibustion 86 32.460 0 (30.307 5, 37.532 5) -0.415 0.678 Sham laser moxibustion 89 32.570 0 (28.625 0, 38.215 0)4 CO2 laser moxibustion 84 31.835 0 (29.520 0, 35.092 5) -1.134 0.257 Sham laser moxibustion 89 33.300 0 (29.350 0, 39.485 0)8 CO2 laser moxibustion 83 31.650 0 (28.582 5, 34.975 0) -1.084 0.278 Sham laser moxibustion 87 32.400 0 (27.900 0, 38.735 0)

After-moxibustion reaction CO2 laser moxibustion (n=83) Sham laser moxibustion (n=87)Local erubescence 17 2 Blister 55 0 Blister with suppuration 1 0 Exacerbation of knee stiffness 0 1 Total 73 3
3 Discussion
Some systematic reviews and clinical studies on moxibustion in the treatment of KOA concluded that moxibustion might be an effective treatment for KOA symptom management[16-19].According to the traditional Chinese medicine (TCM) theory, joint pain is inextricably linked to coldness and dampness.The effect of moxibustion is considered mainly due to its thermal effect on the skin surface.Our study used the 10.6 μm CO2laser beam, and its uniqueness is that it produces potent superficial heat, which mimics moxibustion in TCM.Our research demonstrated that CO2laser moxibustion could significantly improve symptoms such as pain, stiffness, and functional disorders in patients with KOA.Meanwhile, effective blinding methods are possible in a trial design with CO2laser moxibustion, but blinding is not feasible while using traditional moxibustion.
We found that three WOMAC parameters dropped significantly in KOA participants after 2 weeks of CO2laser moxibustion treatment, and they continued to drop throughout the trial.These trends were maintained even 4 weeks after completion of the treatment.Therefore, we concluded that CO2laser moxibustion has significant short-term therapeutic effects and continues to relieve symptoms after treatment termination in patients with KOA.This study was designed to determine the short-term therapeutic effects of CO2laser moxibustion on KOA patients.Therefore, we conducted a follow-up assessment at just 1 month instead of 6 months after treatment as recommended by the Osteoarthritis Research Society International (OARSI)[20].We did not monitor the longterm therapeutic effects of CO2laser moxibustion.
In the trial, some patients observed local skin flushing or blistering (normally one day after treatment) at the site of irradiation.Usually, the blister was naturally absorbed within a day or two without obvious scarring of the skin.The formed blisters were similar to blistering and mild local skin burns caused by traditional moxibustion treatment.And in TCM, it’s an irreplaceable way to ameliorate the clinical symptoms of patients.For example, blistering cupping has been used to treat the syndrome of intense heat.Besides,some researchers found that blistering moxibustion could relieve the visceral hypersensitivity of mice with visceral hypersensitive IBS, and the underlying mechanism is related to the regulation of the gut-brain axis[21].The 10.6 μm CO2laser applied in this study has a 0.2 mm penetration depth, and 90% of its thermal energy is absorbed by the water content in the skin epidermis and stratum corneum.The heat is then conducted from superficial layers to deeper skin layers[22].Although we tried different laser output intensities in our pilot study to determine the one used in this study, the possibility of blistering after treatment cannot be entirely avoided.This is because the acceptance of moxibustion treatment varies among patients because of pain threshold, thicknesses of superficial skin layers, and local skin temperature differences induced by secretion of sweat glands.Therefore, all enrolled participants were informed of the possibility of blistering after treatment.Because blistering during moxibustion is common and accepted among Chinese patients, many patients did not regard blistering as a negative side effect of the treatment.This explains why the patients did not complain about blistering or regard it as an adverse event.
At the follow-up assessment, we asked participants to guess their group assignments to test the masking effectiveness of our trial.We found that most of the participants chose “not sure” instead of either “CO2laser moxibustion” or “non-CO2laser moxibustion.”Firstly, the participants were not familiar with the real treatment sensation, and the CO2laser is infrared, so it is impossible to guess group assignments based on appearance.Further, improved outcomes of WOMAC scores of the sham laser moxibustion group compared with the baseline suggested that placebo effects occurred among participants in the sham laser moxibustion group who thought they received real treatments.Nevertheless, some participants might have realized they were in the CO2laser moxibustion group based on local skin flushing or blistering after treatment,which causes problems for our allocation concealment.Regardless, most patients still chose “not sure” at the follow-up assessment.This may be a result of a vague explanation in the informed consent form.In the form,we did not tell our participants that they would receive real or sham treatments.Instead, we told patients that either “CO2laser moxibustion” or “non-CO2laser moxibustion” would be given, and there was no guarantee for therapeutic effects in either group.This can partly explain why most participants were not sure about their group assignment even after treatmentinduced skin flushing and blistering.We ascribe this response to the lack of knowledge about this new treatment modality among the participants.
Some weaknesses of this study may be able to inspire further studies in several areas.First, an assessment of the long-term therapeutic effects is warranted to determine the impact of CO2laser moxibustion on patients with KOA in terms of treatment time.This would be an important reference for deciding a course of treatment in clinical application.Second, we noticed that local skin flushing or blistering occurred in some participants even though we strictly controlled laser output intensity and the distance between the laser tip and skin.These individualized responses to the treatment indicate differences in absorbed laser moxibustion stimuli, which are caused by local skin thickness, skin water content, or skin keratosis.Future studies may take individual differences into account when prescribing moxibustion treatments.
In conclusion, this clinical trial shows that CO2laser moxibustion can reduce pain and improve joint function in patients with KOA.Therefore, CO2laser moxibustion may be an effective and convenient way to treat patients with KOA.
Conflict of Interest
The authors declare that there is no potential conflict of interest in this article.
Acknowledgments
This study was partially supported by the National Basic Research Program of China (973 Program, 国家重点基础研究发展计划项目, No.2009CB522901); Project of National Natural Science Foundation of China (国家自然科学基金项目, No.81202648); the Key Program of State Administration of Traditional Chinese Medicine of China(国家中医药管理局重点项目); Project of Shanghai Municipal Natural Science Foundation (上海市自然科学基金项目, No.11DZ1973300).
Statement of Informed Consent
This study protocol was approved by the Institutional Review Board of Shuguang Hospital, Shanghai University of Traditional Chinese Medicine (Approval No.ISRCTN26065334).Informed consent was obtained from all individual participants in this study.
Authors’ contributions
Professor ZHAO Ling and Doctor WU Fan had full access to all study data and took responsibility for the integrity of the data and the accuracy of data analysis.XU Jingwen, CHENG Ke, DENG Haiping, and SHEN Xueyong contributed equally to this manuscript.All authors read and approved the final manuscript.
Received: 6 April 2023/Accepted: 16 May 2023
猜你喜欢
杂志排行
Journal of Acupuncture and Tuina Science的其它文章
- Effects of electroacupuncture at Baihui (GV20) and Yintang (GV29) on endoplasmic reticulum stress in depressive rats caused by chronic unpredictable mild stress
- Effects of acupuncture and moxibustion on PINK1/Parkin signaling pathway in substantia nigra of Thy1-αSyn transgenic mice with Parkinson disease
- Acupuncture compound anesthesia for traditional thyroidectomy: a systematic review and meta-analysis
- Effects of abdominal Tuina on behavioral function and 5-hydroxytryptamine 1A receptor/synapsin-1 in hippocampal CA1 region of rats with hypoxic-ischemic brain injuries
- Effects of auricular point sticking on labor pain and anxiety
- Clinical study of Tuina combined with functional training to improve the clinical symptoms and balance function in patients with meniscus injury
