Abdominal electroacupuncture for post-stroke constipation: a randomized controlled trial
2023-12-25LIUGuanping刘关平SUNYuanzheng孙远征GUOYing郭颖SUNYingzhe孙颖哲YUTianyang于天洋YAOJia姚嘉
LIU Guanping (刘关平), SUN Yuanzheng (孙远征), GUO Ying (郭颖), SUN Yingzhe (孙颖哲), YU Tianyang (于天洋),YAO Jia (姚嘉)
1 Heilongjiang University of Chinese Medicine, Harbin 150040, China
2 The Second Affiliated Hospital of Heilongjiang University of Chinese Medicine, Harbin 150001, China
Abstract
Keywords: Acupuncture Therapy; Electroacupuncture; Lactulose; Constipation; Stroke; Complications; Randomized Controlled Trial
Constipation is one of the common complications of stroke.The incidence rate is as high as 30%-60%[1].It is mainly manifested as dry stools and difficult defecation after the attack of acute cerebrovascular disease.It can be accompanied by abdominal bloating, abdominal pain, loss of appetite, increased blood pressure, and even intestinal obstruction in severe cases[2], closely related to a poor prognosis[3].With the aging of the population, poor eating habits, and increasing pressure in the living environment, the incidence of stroke is increasing year by year[4].Stroke seriously threatens the health of patients[5]and brings great distress to patients and their families.Patients with constipation after stroke can further present with dysphoria,
unconsciousness, and intelligence decline due to intestinal blockage, which not only affects the quality of life but also delays the rehabilitation process of patients.At present, there are two main clinical methods for constipation after stroke: internal treatment and external treatment.The internal treatment mostly facilitates defecation through oral drugs, such as lactulose oral liquid and phenolphthalein tablets.The external treatment mostly uses rectum administration of glycerol enema and enema of warm soapy water.The above methods can often temporarily alleviate the symptoms of constipation, but the dependence is strong, and there may be a risk of damaging the intestinal flora.Therefore, a method with stable efficacy is needed.As a common means of rehabilitation treatment for stroke, acupuncture is effective and easy to operate in the treatment of constipation after stroke[6-8].This study aimed to compare the efficacy of electroacupuncture (EA) plus lactulose and oral lactulose alone in the treatment of constipation after stroke and to observe the effect of abdominal EA on intestinal function.
1 Clinical Materials
1.1 Diagnostic criteria
1.1.1 Diagnostic criteria for stroke
The diagnostic criteria for stroke in traditional Chinese medicine (TCM) referred to the Diagnostic Basis, Classification of Syndromes and Evaluation of Curative Effect of Stroke: Criteria for Diagnosis and Curative Effect of Internal Medicine Diseases of Traditional Chinese Medicine of the Chinese Medicine Industry Standard of the People’s Republic of China
(ZY/T001.1-94)[9], and the diagnostic criteria in Western medicine referred to the diagnostic criteria for hemorrhagic or ischemic cerebrovascular disease in
Neurology[10].
1.1.2 Diagnostic criteria for constipation
The diagnostic criteria for constipation in TCM referred to the Criteria of Diagnosis and Therapeutic Effects of Diseases and Syndromes in Traditional Chinese Medicine[11], and the diagnostic criteria in Western medicine referred to the diagnostic criteria in Rome Ⅳ[12].
1.2 Inclusion criteria
Those who met the diagnostic criteria for stroke in TCM and Western medicine; met the diagnostic criteria for constipation in TCM and Western medicine; those who had constipation after stroke; patients with clear consciousness and stable vital signs, aged 18-80 years old, gender unlimited; those who did not have any treatments for constipation 1 week before the trial;patients and their families agreed and signed the informed consent.
1.3 Exclusion criteria
Patients with habitual constipation; those who had mechanical ileus; patients with pathological or physiological conditions that affected the detection indicators; those who received other interventions that conflicted with the current treatment.
1.4 Elimination and dropout criteria
Those who discontinued the treatment arbitrarily or were not able to cooperate with the treatment; those who had serious adverse reactions that had to stop the treatment; those who got worse in the disease condition or who received other treatments; those who dropped out during the treatment.
1.5 Statistical methods
All data were statistically analyzed using SPSS version 26.0 statistical software.Counting data were analyzed by Chi-square test.Rank-sum test was used for comparisons of ranked data.Measurement data were first tested for normality, and those in normal distribution were expressed as mean ± standard (.Independent sample t-test was applied to the comparisons between groups.Paired t-test was applied to intra-group comparisons.If data did not meet the normal distribution, non-parametric test was applied.P<0.05 indicated a statistically significant difference.
1.6 General data
This clinical study was reviewed and approved by the Ethics Committee of the Second Affiliated Hospital of Heilongjiang University of Chinese Medicine, and the approval number was [2021]K158.Patients from the outpatient and ward of the Acupuncture Department of the Second Affiliated Hospital of Heilongjiang University of Chinese Medicine were collected between May 2021 and May 2022.A total of 100 patients who met the inclusion criteria were enrolled.All cases were divided into an observation group and a control group by the random number table method according to the visiting sequence on the first visit, with 50 cases in each group.During the treatment, 4 cases in the observation group dropped out (1 case dropped out due to condition worsening and 3 cases due to taking other interventions),and 4 cases in the control group dropped out due to taking other interventions.Finally, 92 cases were included in the statistics.The disease duration in the observation group ranged between 7 d and 90 d.The disease duration in the control group ranged between 9 d and 88 d.There were no significant differences in the general data of gender, age, and duration of disease between the two groups (P>0.05), indicating that the two groups were comparable (Table 1).
2 Treatment Methods
All enrolled patients were given the routine basic treatment for stroke.
2.1 Control group
The control group was treated with oral lactulose,10 mL each time, 3 times a day, for 2 consecutive weeks.

Group n Gender/case Age/year(Male Female x ±s)Duration/day(x ±s)Observation 46 26 20 60.2±9.1 40.5±26.2 Control 46 28 18 60.2±8.8 40.4±22.6
2.2 Observation group
The observation group was treated with additional EA at abdominal points on the basis of oral lactulose.
Points: Bilateral Tianshu (ST25), Fushe (SP13), and Daheng (SP15).
Methods: The patient emptied the urine in advance and took a supine position with the abdomen exposed.Point areas were disinfected with 75% alcohol cotton balls.The Hwato brand disposable sterile acupuncture needles (0.40 mm in diameter and 40 mm in length)were inserted 30 mm deep.Balanced reinforcingreducing manipulation was applied for all points.After the arrival of needling sensation (Deqi), bilateral Tianshu (ST25), left Fushe (SP13) with left Daheng(SP15), and right Fushe (SP13) with right Daheng (SP15)were connected to a KWD-808I pulse acupuncture therapeutic apparatus, with a continuous wave at 3 Hz.The intensity was set according to the patient’s tolerance.The needles were retained for 30 min each time.The treatment was performed once a day for 2 consecutive weeks.
3 Observation of Curative Efficacy
3.1 Observation items
3.1.1 Primary observation item
The constipation symptom score referred to the
Consensus on TCM Diagnosis and Treatment of Constipation[13], mainly including 6 items: fecal traits,defecation effort, defecation time, persistent feeling of heaviness and bloating of the anus, defecation frequency, and abdominal bloating.Each item scored 0-3 points, with a maximum of 18 points.The higher the score, the severer the constipation symptoms.
3.1.2 Secondary observation item
Patient assessment of constipation quality of life scale (PAC-QOL)[14]mainly assessed physiology,psychology, anxiety, and satisfaction with a total of 28 items.The Likert scale five-level scoring method was adopted, 0-4 points for each item, and the total score was between 0-112 points.The higher the score, the worse the quality of life of patients.
Serum motilin (MTL) detection: Venous blood was collected from patients on an empty stomach, placed in a serum separation tube for 2 h at room temperature,and centrifuged at 1 000 r/min for 20 min.The supernatant was taken and measured using the MTL enzyme-linked immunosorbent assay kit.
Mini-mental state examination (MMSE) score: the cognitive level was evaluated according to the educational level of patients[15].
3.2 Criteria for curative efficacy
This study referred to the Consensus on TCM Diagnosis and Treatment of Constipation[13].According to the reduction rate of constipation symptom score, the efficacy was evaluated by Nimodipine method.Reduction rate of constipation symptom score = (Constipation symptom score before treatment - Constipation symptom score after treatment) ÷ Constipation symptom score before treatment × 100%.
Cured: Constipation basically disappeared, and the reduction rate of constipation symptom score was≥95.0%.
Markedly effective: Constipation was significantly improved, and the reduction rate of constipation symptom score was ≥70.0% but <95.0%.
Effective: Constipation was improved, and the reduction rate of constipation symptom score was≥30.0% but <70.0%.
Invalid: Constipation was not significantly improved or even worse, with the reduction rate of constipation symptom score <30.0%.
3.3 Results
3.3.1 Comparison of the clinical efficacy
The total effective rate of the observation group was higher than that of the control group, and the difference between the two groups was statistically significant (P<0.05).See Table 2.
3.3.2 Comparison of the constipation symptom score
Before treatment, there was no statistical difference in the constipation symptom score between the two groups (P>0.05), indicating that the two groups were comparable.After treatment, the constipation symptom scores in both groups decreased (P<0.05), and the score in the observation group was lower than that in the control group (P<0.05).See Table 3.
3.3.3 Comparison of the PAC-QOL score
Before treatment, there was no statistical difference in the PAC-QOL score between the two groups (P>0.05),indicating that the two groups were comparable.After treatment, the PAC-QOL scores in both groups decreased (P<0.05), and the score in the observation group was lower than that in the control group (P<0.05).See Table 4.
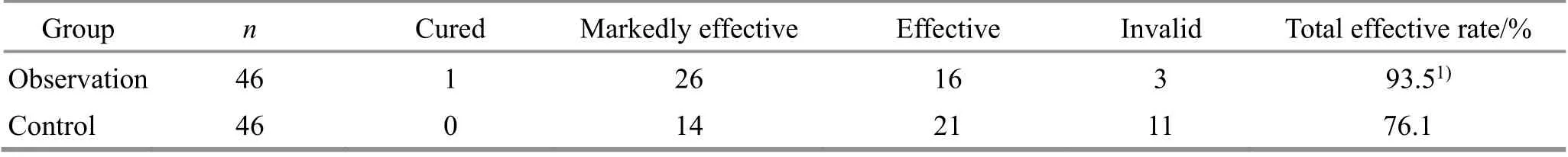
Group n Cured Markedly effective Effective Invalid Total effective rate/%Observation 46 1 26 16 3 93.51)Control 46 0 14 21 11 76.1
3.3.4 Comparison of the serum MTL level
Before treatment, there was no statistical difference in the serum MTL level between the two groups(P>0.05), indicating that the two groups were comparable.After treatment, the serum MTL levels in both groups increased (P<0.05), and the serum MTL level in the observation group was higher than that in the control group (P<0.05).See Table 5.

Group n Before treatment After treatment Observation 46 215.50±23.12 250.30±23.201)2)Control 46 216.63±22.31 238.98±24.261)
3.3.5 Comparison of the MMSE score
Before treatment, there was no statistical difference in the MMSE score between the two groups (P>0.05),indicating that the two groups were comparable.After treatment, the MMSE scores in both groups increased(P<0.05), and the score in the observation group was higher than that in the control group (P<0.05).See Table 6.

Group n Before treatment After treatment Observation 46 26.15±1.93 27.78±1.441)2)46 26.41±1.81 27.13±1.441)Control
4 Discussion
In Chinese medicine, post-stroke constipation falls under the category of “stoke” and “splenic constipation”.Its etiology and pathogenesis are interrelated[16].The disorder of Qi, blood, Yin, and Yang generates wind internally, and vessels and collaterals in the brain block or blood overflows outside the vessels, resulting in hemiplegia.The dysfunction of Zang-Fu organs and uncontrolled transportation and transformation functions result in constipation.The spleen and stomach are the source of Qi and blood generation and transformation.The treatment of constipation after stroke should regulate the spleen and stomach.
The abdominal points were selected in the acupuncture treatment.Tianshu (ST35) locates 2 Cun next to the navel, where Qi movement crosses,manifesting the meaning of selecting local points.Meanwhile, Tianshu (ST25) is the Front-Mu point of the large intestine, which primarily treats the disease of six Fu organs, and regulates the transportation and transformation function of the intestine.Daheng (SP15)locates 4 Cun next to the navel.Fushe (SP13) locates 4 Cun below the navel and 4 Cun beside the anterior midline.Both points can promote the transportation and transformation of Qi, blood, and body fluids.Connecting EA to the above points can stimulate Qi of the spleen and stomach meridians, promote gastrointestinal motility, and strengthen gastrointestinal transportation and transformation.
The process of transforming food from intake to feces is very complicated, including being stored and fermented in the stomach, absorbed by the small intestine, reabsorbed by the colon, and finally discharged through the rectum.The change in colon function is the key factor in the occurrence of constipation[17].Anatomically, Tianshu (ST25), Fushe(SP13), and Daheng (SP15) are distributed in the abdominal area near the navel, and these regions are adjacent to the colon.Difficult defecation in constipation is mainly caused by transportation and transformation, secretion, and absorption dysfunctions of the large intestine.EA treatment stimulates the above points with acupuncture to achieve the effect of local stimulation, promoting gastrointestinal peristalsis and improving intestinal neuroendocrine function, thus improving the symptoms of constipation in stroke patients[18].
MTL is an orexigenic peptide[19]produced by enteroendocrine cells.It is associated with gastrointestinal dysfunction[20]and may lead to constipation when insufficient[21].This study found that after abdominal EA treatment, the flatus, defecation,and MTL level of patients in the observation group were significantly improved compared with those in the control group.
Recent research has found “brain-gut communication”[22], and these two influence each other in the anatomical structure and function and are closely related.Some scholars put forward the “abdomenbrain” theory[23], believing that the gastrointestinal tract was the second brain of the human body and could effectively improve patients’ brain symptoms by regulating gastrointestinal function.Acupuncture at abdominal points can not only treat topical diseases but also give feedback to the brain through the brain-gut axis, achieving the effects of regulating the brain and promoting the recovery of cerebral function.After receiving the stimulation signal, the brain can further play the role of the command and then regulate the peripheral nerve.These theories have been proved by clinical studies.For example, patients with constipation after stroke also often show senior nerve dysfunction of cognition and emotion[24], and the cognitive level can be effectively increased by improving post-stroke constipation.
Results of this study suggested that EA at abdominal points could effectively reduce the constipation score and improve constipation symptoms in stroke patients and had positive promoting effects on their psychological and physiological, which could improve their satisfaction and life quality and increase the serum MTL level and cognitive score.
This study proved that EA at abdominal points could improve intestinal function in stroke patients with constipation, and the change in intestinal function had certain relativity with cognitive improvements.However,due to the limitation of funds and time, the sample size of this study was small, and there were many shortcomings, such as a lack of syndrome differentiation classification of TCM and the detection of intestinal flora.We hope that more support can be obtained in future studies to optimize the trial’s design and provide references for further clinical studies.
Conflict of Interest
The authors declare that there is no potential conflict of interest in this article.
Acknowledgments
This work was supported by SUN Shentian Youth Talent Fund (孙申田青年人才基金, No.2020KY-03).
Statement of Informed Consent
Informed consent was obtained from all individual participants.
Received: 13 March 2023/Accepted: 16 June 2023
猜你喜欢
杂志排行
Journal of Acupuncture and Tuina Science的其它文章
- Effects of electroacupuncture at Baihui (GV20) and Yintang (GV29) on endoplasmic reticulum stress in depressive rats caused by chronic unpredictable mild stress
- Effects of acupuncture and moxibustion on PINK1/Parkin signaling pathway in substantia nigra of Thy1-αSyn transgenic mice with Parkinson disease
- Acupuncture compound anesthesia for traditional thyroidectomy: a systematic review and meta-analysis
- Effects of abdominal Tuina on behavioral function and 5-hydroxytryptamine 1A receptor/synapsin-1 in hippocampal CA1 region of rats with hypoxic-ischemic brain injuries
- Effects of auricular point sticking on labor pain and anxiety
- Clinical study of Tuina combined with functional training to improve the clinical symptoms and balance function in patients with meniscus injury
