Different approaches for treating myopic choroidal neovascularization: a network Meta-analysis
2023-12-14YaJunWuYuLiangFengJiaSongYangHuaFanWenShengLi
Ya-Jun Wu, Yu-Liang Feng, Jia-Song Yang, Hua Fan, Wen-Sheng Li
1Aier School of Ophthalmology, Central South University,Changsha 410000, Hunan Province, China
2Department of Ophthalmology, Shanghai Aier Eye Hospital,Shanghai 200235, China
3Shanghai Aier Eye Institute, Shanghai 200235, China
Abstract
● KEYWORDS: myopic choroidal neovascularization;aflibercept; bevacizumab; conbercept; laser treatment;ranibizumab; photodynamic therapy
INTRODUCTION
At present, myopia is a global public health problem[1],as the main cause of the uncorrected refractive error,which brings a huge economic burden every year[2].According to statistics, the direct cost of myopia per person per year is around $20 in the United States, while in Singapore it is as high as $199, and the per capita cost of contact lenses and refractive surgery is over $300.This shows that the economic burden brought by myopia cannot be underestimated[3].High myopia (HM) is defined as ametropia with a diopter (D) of≤-6 or more[4].Moreover, HM is associated with a significant increase in visual impairment and the significant increase in irreversible blindness[5].According to a Meta-analysis, nearly half of the world’s population could suffer from myopia by 2050, of which the HM population will be as high as 10%[6].Usually, if HM individuals have characteristic fundus pathological changes such as leopard-shaped fundus and chorioretinal atrophy (CRA), it is called pathological myopia(PM)[7], although there is no clear clinical definition of the latter.Furthermore, compared with ordinary myopia, HM significantly increases the risk of complications caused by PM significantly, such as retinal atrophy, retinal detachment (RD),cataract, glaucoma, myopic macular degeneration, and myopic choroidal neovascularization (mCNV)[8-10].
A complication of PM, mCNV affects approximately 5%-11% of PM patients, of which about 15% of cases involve both eyes[11].The disease mainly refers mainly to the formation of abnormal neovascularization under the retinal pigment epithelium or retina[12].The vision of patients who have not been treated for a long time will also be reduced significantly[13].Therefore, timely treatment of mCNV is very important.Currently, there are several effective treatments for mCNV, including retinal laser photocoagulation, photodynamic therapy (PDT), and intravitreal injection of anti-vascular endothelial growth factor (anti-VEGF) drugs,etc.All of them have been shown to be effective in the treatment of mCNV.Matsudaet al[14]found that, after laser treatment (LT), mCNV patients were followed up for 13-60mo, and, despite the phenomenon of laser photocoagulation scar enlargement in approximately 80% of patients, almost all patients had no vision loss and were well-controlled.Also, PDT, improved vision acuity in patients with mCNV during a one-year followup[15].
In addition, with the emergence of anti-VEGF drugs and successful application in many other retinal angiogenic diseases, anti-VEGF therapy has gradually become a common treatment for mCNV.Castellinoet al[16]found that, after 12mo of anti-VEGF treatment, the subretinal hyperreflexic exudation,subretinal effusion, and intraretinal cyst almost disappeared in 40 mCNV patients, and the best-corrected vision acuity(BCVA) was improved.Currently, commonly used anti-VEGF drugs include aflibercept, ranibizumab, bevacizumab, and conbercept (which was produced in China and was approved by the State Food and Drug Administration of China in 2017 for the treatment of mCNV).However, some patients still lost their central vision after anti-VEGF treatment, which might be related to macular atrophy[17].
Although there have been Meta-analyses on mCNV.They have been mainly traditional Meta-analyses comparing two treatment methods.For example, Huet al[18]compared the efficacy of intravitreal bevacizumab (IVB) and intravitreal ranibizumab (IVR) in the treatment of mCNV in a Meta-analysis and confirmed that both of them were effective treatment measures, although there was no statistical difference between the two treatments.Additionally, Wang and Chen[19]compared IVR/IVB combination with PDT treatment and found that anti-VEGF as a treatment for mCNV has better therapeutic effects.However, so far, no network Meta-analysis has compared comprehensively the various treatment methods and the four different anti-VEGF drugs.Therefore, the purpose of this study is to compare and rank the efficacy of several existing mCNV treatment methods, to obtain the best method of mCNV treatment and provide useful information for guiding clinical treatment of the disease.
MATERIALS AND METHODS
Protocol and RegistrationThis study has been pre-registered in the International Prospective Register of Systematic Reviews under the registration number PROSPERO (https://www.crd.york.ac.uk/prospero/): CRD42021287142.This network Metaanalysis was conducted and presented in accordance with the Preferred Reporting Items for Systematic Reviews and Meta-Analysis (PRISMA) guidelines[20].
Search StrategyIn order to obtain appropriate randomized controlled trials (RCTs) and retrospective articles as far as possible, we searched PubMed, Embase, Web of Science,Cochrane Library, and other databases, the retrieval time limit is from the establishment of each database to January 30,2023.The language of this article is limited to English, and the keywords searched are as follows, “myopia”, “choroid neovascularization”, “mCNV”, “pathological myopia”,“PM” ,“photodynamic therapy”, “PDT”, “anti-VEGF”,“bevacizumab”, “IVB”, “aflibercept”, “IVA”, “ranibizumab”,“IVR”, “conbercept”, “IVC”, “laser treatment”, “laser photocoagulation”, “mCNV”, “complications”, “chorioretinal atrophy”, “CRA”, “randomized controlled trials”, “RCT”,“retrospective studies”.
Inclusion and Exclusion CriteriaWe included and analyzed RCTs and retrospective studies respectively.These studies are comparative articles on different treatment methods for mCNV patients, mainly including the comparison of BCVA changes before and after treatment.
Inclusion criteria: 1) mCNV patients (CNV patients secondary to PM: refractive error more than equal to -6.0 diopter, or axial length greater than 26 mm) received treatment, regardless of race, region, occupation, and age; 2) The data were complete,including baseline BCVA and post-treatment BCVA; 3)Comparison of the efficacy of at least two treatment methods.Exclusion criteria: 1) Study subjects are not patients with CNV secondary to PM; 2) Single-arm study without a comparison of treatment measures; 3) Non-original articles such as summarization and experience summary; 4) Incomplete data or incomplete data cannot be obtained from the author.
OutcomeThe primary outcome was the mean change in BCVA after treatment from baseline, and the VA was logarithmic visual acuity (logMAR) converted from BCVA measurements.The secondary outcome measure was the change in foveal center thickness (FCT) on optical coherence tomography (OCT).Post-treatment CRA was as a secondary outcome indicator (only two retrospective studies include this data).
Literature Selection and Data ExtractionIn this study, two authors (Feng YL and Yang JS) independently read the title and abstract of the article according to the inclusion and exclusion criteria, exclude the articles that clearly do not meet the requirements, and then determine the final included literature by reading the content of the article in detail.If the two authors disagree in this process, they will consult or discuss and submit it to the third senior researcher for adjudication, Missing data were obtained by contacting the corresponding authors of the included literature.
Statistical AnalysisADDIS 1.16.8 (the Netherlands; http://www.drugis.org/index) and R version 4.3.1 (New Zealand;https://www.r-project.org/) software were used to analyze the data.The Cochrane Collaboration’s Review Manager Software(RevMan Version 5.3, Cochrane Community) was used to create quality evaluation figures.In this study, quantitative data and mean square deviation (MD) were used as the effect indicator, and the MD and standard deviation (SD) of each group of data were extracted for joint analysis.Point estimates and 95% confidence intervals (CI) of each effect indicator were given.χ2test (α=0.1) was used to analyze the heterogeneity among the included studies, andI2was used to determine the heterogeneity.If the heterogeneity among the results was small, the fixed-effect model was used for Metaanalysis.Otherwise, if the heterogeneity among the results was large, the random-effect model was used for Meta-analysis after excluding the influence of obvious clinical heterogeneity,andP<0.05 between each group was considered statistically significant.ADDIS software was used to calculate the potential scale reduction factor (PSRF) to diagnose the convergence degree of the model.Set the initial value of 4 Markov chains,the initial value of the model is 2.5, refine the iteration step size by 10, adjust the number of iterations by 20 000 times,and simulate the number of iterations by 50 000 times.Only when the PSRF value tends to 1 indicates that the convergence of the model is satisfactory.
The R software calls “RJAGS”, “GEMTC” program package to establish the Bayesian model, and calls “Network” program package to draw the evidence Network diagram of each intervention.The straight line indicates that there is direct comparison evidence between the two interventions, and the wireless connection lacks direct comparison evidence.The thicker the line, the more studies that directly compared the two interventions.The optimal probability ranking curve(SUCRA) value was calculated, the ranking map was drawn to predict the ranking of therapeutic effects of various measures,and the forest map for direct comparison was drawn.For the study of generating Node Split nodes, the Node Split model was first used to test the consistency of direct comparison and indirect comparison.P>0.05 indicated good consistency and the consistency model was used for analysis.Instead, adopt the inconsistency model.
RESULTS
Flow Chart and Characteristic Table
Literature search resultsWe preliminarily searched 763 articles, deleted 61 duplicate articles, 617 non-comparative original articles were deleted, excluded 56 articles by reading the title and abstract, excluded 13 articles after reading the full text, and finally included 16 articles that met the criteria(Figure 1).

Figure 1 Flow chart of literature search and screening CNV:Choroidal neovascularization; RCT: Randomized controlled trial.
Basic characteristics of the included studyA total of 16 articles were included, including 8 RCTs and 8 retrospective studies, involving 1072 eyes.The following is the characteristic table of the original literature (Table 1)[21-36].Figure 2 depicts the quality of the included studies in the Meta-analysis;Overall, RCTs were of better quality than retrospective studies.Evidence Network DiagramFigure 3A shows the network diagram of 6 different mCNV treatment methods in the BCVA results of RCTs, a total of 6 interventions including IVA, IVR, IVB, PDT, LT, and sham-combined IVA were involved in the network Meta-analysis; Figure 3B shows the network relationship diagram of different treatment methods for mCNV in the BCVA results from retrospective studies, the network Meta-analysis involves 7 interventions: IVA, IVR,IVB, IVC, IVB or IVR treatment, PDT treatment alone, and PDT combined with IVB or IVR treatment; Figure 3C shows a network diagram of 4 different treatments(IVB, IVR, IVA,PDT) in RCTs of FCT results.Figure 3D shows a network diagram of 5 different treatments (IVA, IVB, IVC, IVR, PDT)in the FCT results of retrospective studies; The line thickness in the figure is positively correlated with the number of studies directly comparing the two interventions.
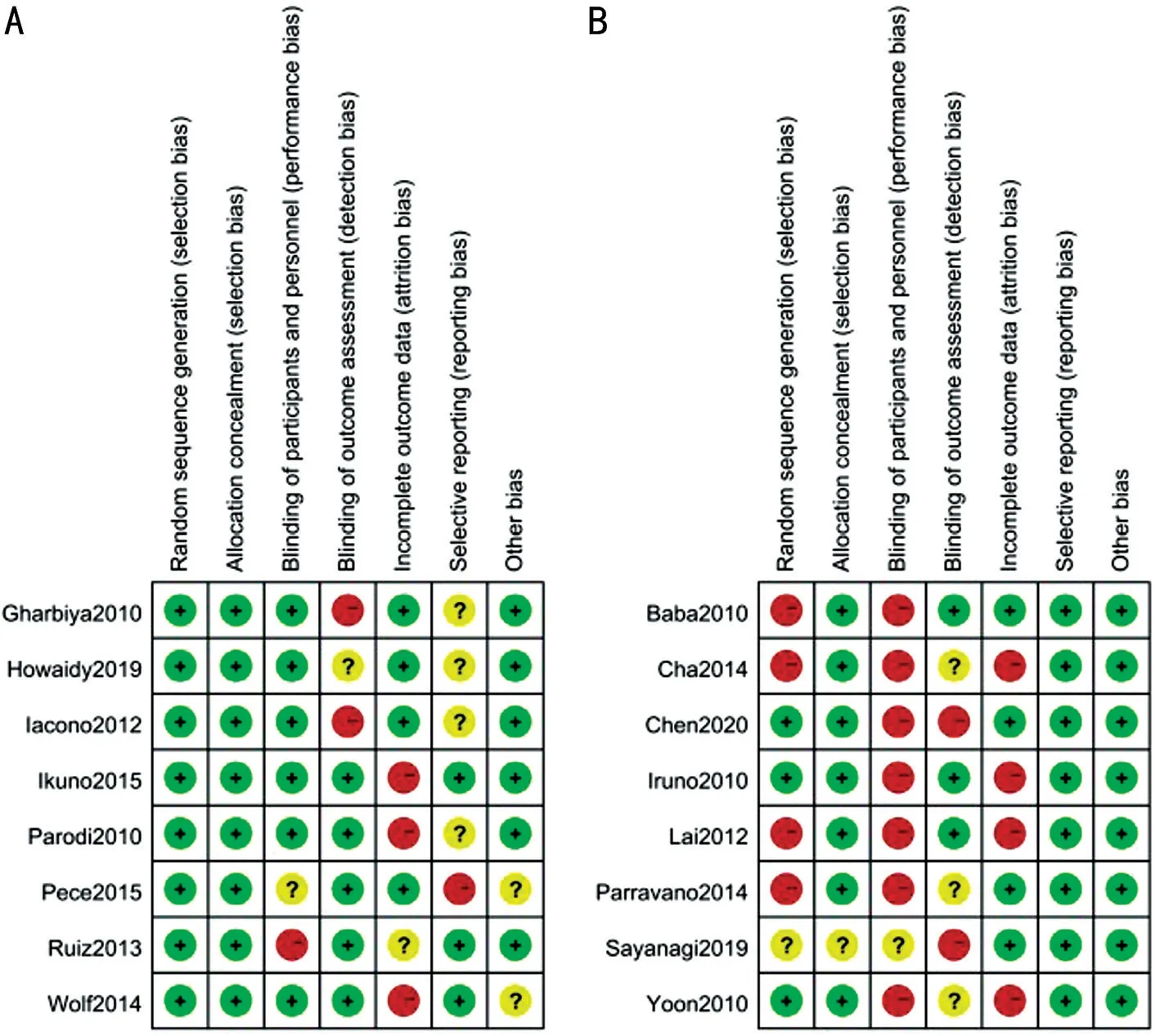
Figure 2 Quality evaluation figures A: RCTs; B: Retrospective studies.RCT: Randomized controlled trial.

Figure 3 Network diagram of different interventions A: A network diagram of different treatment methods improving BCVA results in RCTs;B: A network diagram of different treatments improving BCVA outcomes in retrospective studies; C: A network diagram of different treatment methods improving FCT outcomes in RCTs; D: A network diagram of different treatments improving FCT outcomes in retrospective studies.ShamIVA: IVA treatment followed by sham treatment; IVBIVR: Patients undergoing IVB or IVR treatment; PDTIVBIVR: Patients receiving PDT combined with IVB or IVR treatment.RCTs: Randomized controlled trials; FCT: Foveal center thickness; BCVA: Best-corrected vision acuity; IVA:Intravitreal aflibercept; IVB: Intravitreal bevacizumab; IVR: Intravitreal ranibizumab; IVC: Intravitreal conbercept; PDT: Photodynamic therapy;LT: Laser treatment.
Convergence and Stability Evaluation Results of the Study were IncludedThe convergence diagnosis diagram and trajectory density diagram are drawn to evaluate the convergence and stability of the model.Before 50 000 iterations of the model, the convergence diagnosis diagram and trajectory diagram have converged.The density diagram is a curve with a normal shape and smooth distribution, and the bandwidth value approaches 0, suggesting that the convergence degree of the model is satisfactory and the stability is good.
Network Meta-Analysis
Randomized controlled trials
Results of BCVA changesIn the 8 articles included, the changes in BCVA in patients were described.In the included study, a significant increase in BCVA from baseline after most treatments were observed.A comprehensive analysis was carried out using Addis and R software.The results of network Meta-analysis showed that: BCVA improvement after IVB and IVR treatment was better than PDT [MD=0.18, 95%CI (0.02,0,40), MD=0.18, 95%CI (0.01, 0.42)].There was no statistical significance in the comparison of postoperative hospital stay between other closure methods (Table 2).
Node analysis showed that allP>0.05, reflecting that there was no statistical inconsistency between the results of direct comparison and indirect comparison (Table 3).
The degree to which six treatment methods improve BCVA was ranked.The darker the color, indicating the best treatmenteffect.The probability of IVA and IVR ranking first is similar,with 0.39 and 0.40, respectively.IVB ranks third, and Sham/IVA and PDT may have the worst efficacy.Combining Figure 3 and Table 4, it can be concluded that the ranking result may be IVR, IVA, IVB, LT, PDT, Sham/IVA (Figure 4 and Table 4).

Table 1 Characteristics of the table
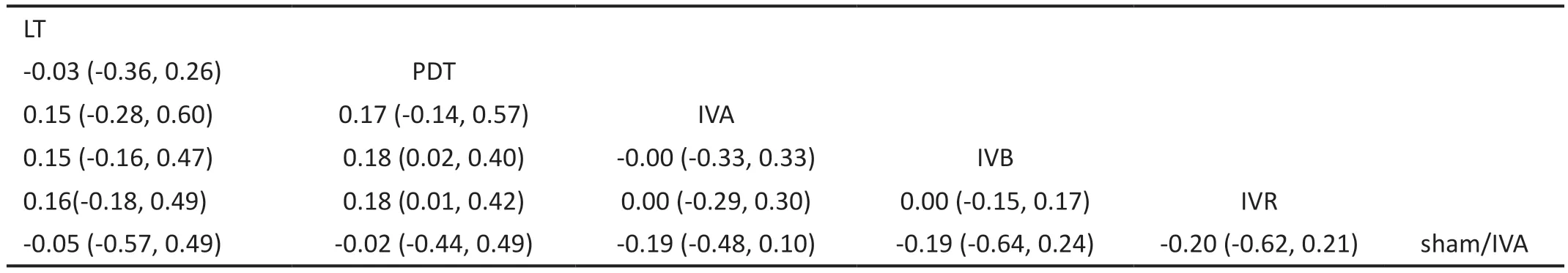
Table 2 Different treatment methods improve the results of a Meta-analysis of BCVA mesh (RCTs)
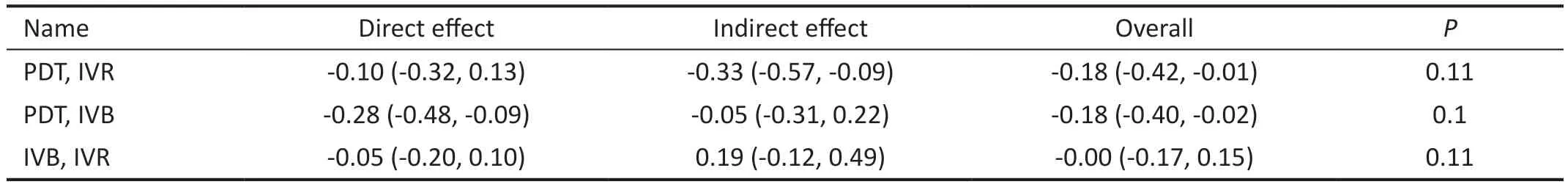
Table 3 The consistency of direct comparison and indirect comparison of various treatment methods with BCVA change as the node (RCTs)
Results of foveal center thickness changesAmong all RCTs, there are 5 articles involving the change of FCT results,including IVB, IVA, IVR, and PDT.We extracted the data on FCT changes before and after mCNV treatment and found that these treatment methods have no statistical difference in reducing FCT (Table 5).
IVA has the darkest parts and the largest value in rank 1,indicating the best treatment effect, while PDT has the lightest parts and the largest value in rank 4, indicating the worst treatment effect.Thus, the results of the comparison and ranking of the effects of these four treatment methods show that IVA may have the best effect, followed by IVR and IVB,and PDT may have the worst effect (Figure 5 and Table 6).
Retrospective Studies
Results of BCVA changesThe 8 included articles described BCVA changes after 12mo treatment.Addis combined with R software was used for comprehensive analysis, Mesh Meta results showed no statistical difference among all treatments(Table 7).
The node analysis method shows that the direct comparison results are consistent with the indirect comparison results(P>0.05; Table 8).
IVA or IVC have the darkest color and the same proportion in rank 1, both of which are 0.38, indicating the best treatment effect, while PDT has the brightest parts, with a maximum proportion of 0.44 in rank 7, indicating the worst treatment effect.So, the order of increasing the probability of BCVA in mCNV patients may be IVA, IVC, IVR, IVB, IVB/IVR, PDT with IVB/IVR, PDT (Figure 6, Table 9).
Results of foveal center thickness changesA total of 4 retrospective studies involved the changes in FCT results,including IVC, IVB, IVA, IVR, and PDT.We found that these treatment methods had no statistical difference in reducing FCT (Table 10).
Combining the rank Table 11 and Figure 6, it can be seen that IVA has the darkest parts, and has a proportion of 0.74 in rank 1, indicating the best treatment effect, but IVB has the lightest part and a proportion of 0.53 in rank 5 (only two articles[27,33]compared PDT and IVB for FCT, and the results of the two articles were opposite, which may be the main reason for this result).The results of the comparison and ranking of the effects of these five treatment methods show that IVA may have the best effect, followed by IVR, IVC, PDT, and IVB (Figure 7,Table 11).
Results of chorioretinal atrophyBabaet al[33]and Parravanoet al[36]respectively explored the CRA differences between PDTvsIVB and PDTvsIVR.The evaluation of the CRA results after PDT, IVB, and IVR treatment in these two articles showed that although there was no statistical difference among the three methods, the CRA after PDT treatment was the highest, while the CRA after IVB treatment was even smaller than IVR, which means that PDT may be the least effective in improving CRA, while IVB may be the best (Figure 8 and Table 12).
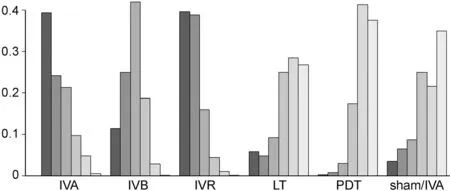
Figure 4 Effect ranking diagram of different treatment methods to improve BCVA (RCTs) The deeper the color on behalf of the treatment the better the results.RCTs: Randomized controlled trials;BCVA: Best-corrected vision acuity; IVA: Intravitreal aflibercept;IVB: Intravitreal bevacizumab; IVR: Intravitreal ranibizumab; PDT:Photodynamic therapy.
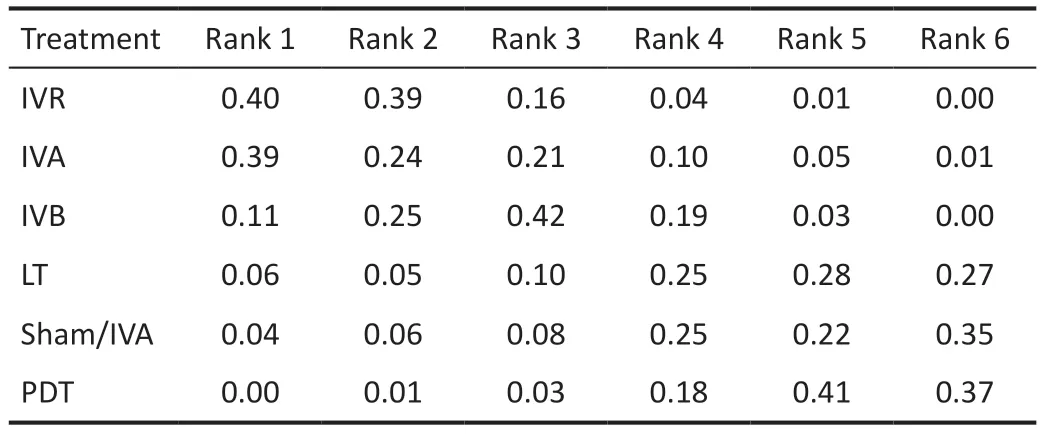
Table 4 Ranking table of the effects of different treatment methods on improving BCVA (RCTs)
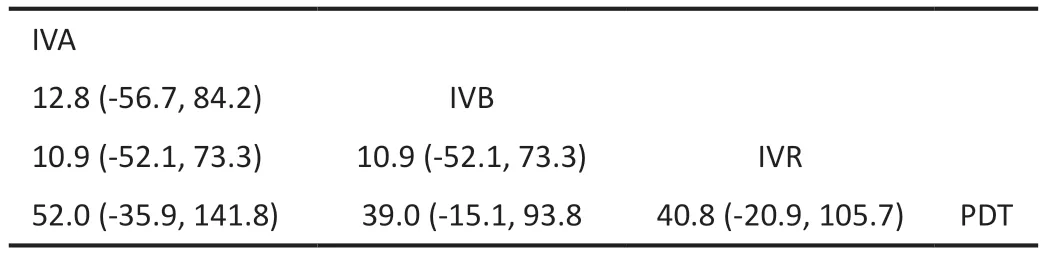
Table 5 Different treatment methods improve the results of a Metaanalysis of FCT mesh (RCTs)

Table 6 Ranking table of the effects of different treatment methods on improving FCT (RCTs)
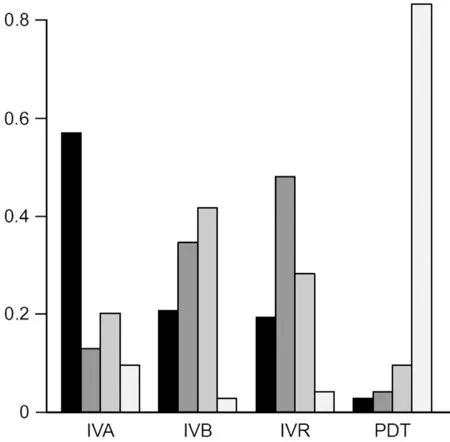
Figure 5 Effect ranking diagram of different treatment methods to improve FCT (RCTs) The deeper the color on behalf of the treatment the better the results.RCTs: Randomized controlled trials;FCT: Foveal center thickness; IVA: Intravitreal aflibercept; IVB: Intravitreal bevacizumab; IVR: Intravitreal ranibizumab; PDT: Photodynamic therapy.

Figure 6 Effect ranking diagram of different treatment methods to improve BCVA (retrospective studies) The deeper the color on behalf of the treatment the better the results.IVBIVR refers to patients undergoing IVB or IVR treatment; PDTIVBIVR refers to patients receiving PDT combined with IVB or IVR treatment.BCVA: Best-corrected vision acuity; IVA: Intravitreal aflibercept;IVB: Intravitreal bevacizumab; IVR: Intravitreal ranibizumab; IVC:Intravitreal conbercept; PDT: Photodynamic therapy.
DISCUSSION
Other Meta-analyses only compared the difference in efficacy between different anti-VEGF drugs or the difference between anti-VEGF drugs and other mCNV treatments.The biggest feature of our study is that RCTs and retrospective studies were used to compare the efficacy of all the mCNV treatments separately, which is more comprehensive.

Figure 7 Effect ranking diagram of different treatment methods to improve FCT (retrospective studies) The deeper the color on behalf of the treatment the better the results.FCT: Foveal center thickness; IVA: Intravitreal aflibercept; IVB: Intravitreal bevacizumab;IVR: Intravitreal ranibizumab; IVC: Intravitreal conbercept; PDT:Photodynamic therapy.

Figure 8 Comparison of CRA results after treatment with different methods (retrospective studies) The deeper the color on behalf of the treatment the better the results (IVB has the darkest parts,indicating the best treatment effect, while PDT has the lightest parts,indicating the worst treatment effect).CRA: Chorioretinal atrophy;IVB: Intravitreal bevacizumab; IVR: Intravitreal ranibizumab; PDT:Photodynamic therapy.
In fact, to compare the efficacy of different anti-VEGF drugs,PDT, LT, and even several combination therapy methods, we tried initially to include only RCTs.However, owing to the lack of statistically significant results after the combination of all appropriate RCTs, and considering the limited current RCTs, we therefore, also conducted the same network metaanalysis on retrospective articles to find the most suitable clinical treatment method for mCNV, and the results were similar to RCTs.This is the first article to compare the efficacy of different mCNV treatment methods in RCTs and retrospective studies, involving 16 articles.The results of both RCTs and retrospective studies showed that anti-VEGF therapy might be the best choice after a long-term treatment follow-up of approximately 12mo.According to the sequencing results,because most of the results showed no statistical significance,we could only find the best possible treatment.The results ofRCT and retrospective studies show that, among anti-VEGF drugs, IVA might have the best effect in restoring the structure and function of mCNV patients, especially in improving FCT.However, owing to the lack of statistical significance,this result is only a possible reference, and more original and higher-quality data are needed to further confirm this result.

Table 7 Different treatment methods improve the results of a Meta-analysis of BCVA mesh (retrospective studies)

Table 8 The consistency of direct comparison and indirect comparison of various treatment methods with BCVA change as the node(retrospective studies)

Table 9 Ranking table of the effects of different treatment methods on improving BCVA (retrospective studies)

Table 10 Different treatment methods improve the results of a meta-analysis of FCT mesh (retrospective studies)
mCNV is one of the complications of myopia, accompanied with severe loss of vision[37].Patients without timely treatment will have very poor vision[38].Previously, LT has been used to treat CNV, but it is limited to extrafoveal mCNV and is not applicable to subfoveal mCNV.This treatment is prone to laser scar expansion and disease recurrence[39-40].In our study, there is only one article involving LT[26], and owing to the small sample size, it only shows that the degree of vision decline of patients is less than following PDT treatment, which has no great advantage in improving visual acuity.In fact, LT can stabilize vision in the treatment of macular diseases, but it seems to be ineffective in improving vision.Kozaket al[41]used LT to treat patients with diabetes macular edema.After 3mo, they found that the vision of all patients remained stableand did not decline, but also did not improve, which is similar to our research results.However, this is not a treatment for mCNV, and because there are so few original articles, we have not found any new articles confirming that LT can improve vision when used to treat mCNV, but it can at most stabilize vision.

Table 11 Ranking table of the effects of different treatment methods on improving FCT (retrospective studies)

Table 12 Effects of different treatment methods on alleviating CRA(retrospective studies)
Moreover, the first treatment method available for mCNV is PDT.In fact, as early as 2001, a clinical study[15]of mCNV treated 81 eyes with PDT and 39 eyes with glucose for sham treatment for 12mo.Compared with the control group, the visual acuity of mCNV patients treated with PDT tended to be stable or even improved, and there were no obvious adverse reactions, which proved that PDT can be used as an effective treatment for mCNV.However, when followed up to 24mo, the visual acuity of the PDT treatment group was no longer improved significantly compared with the placebo control group, which can be said to be mainly manifested as stable visual acuity, which might be caused by PDT treatment exacerbating the development of CRA in myopia patients[42].Also, all the articles included in our study that involved PDT treatment were followed up for 12mo, but there were different evaluations on their efficacy.Some study results showed that the BCVA of mCNV patients improved, whereas others decreased.We speculated that this was related to the small sample size.After all, studies[28,35-36]with a large sample size
all showed that BCVA could be improved after 12mo of PDT treatment, which could mean that longer treatments are more effective in restoring vision.Besides, the CRA differences between PDTvsIVB and PDTvsIVR was discussed in Babaet al[33]and Parravanoet al[36]respectively, indicating that the occurrence of CRA after anti-VEGF treatment is better than that of PDT, and the difference is statistically significant.So we compared the efficacy of IVB, IVR, and PDT in improving CRA in patients with mCNV, and found that IVB may have the best treatment effect, while PDT treatment had the worst effect on improving CRA.Although the statistical results of this mesh meta-analysis are not statistically significant, this may mean that anti-VEGF is the best choice in improving BCVA,FCT, and CRA.
Intravitreal injection of anti-VEGF drugs is considered the first-line treatment of mCNV[43].Maoet al[44]used OCTA to investigate the changes in macular vascular density and foveal avascular zone (FAZ) area in mCNV patients after anti-VEGF treatment.They found that although anti-VEGF treatment could not completely eliminate the lesion area, but macular vascular density and FAZ decreased.Unlike our study, this study confirms the positive therapeutic effect of anti-VEGF on mCNV by starting from the structural improvement of the retina and choroid.In our study, we focused on the differences in retinal and choroid function improved by four common anti-VEGF drugs.Conbercept is a new anti-VEGF drug from China, and, like aflibercept, it is a soluble receptor protein.The difference is that conbercept contains mainly the extracellular domain 2 of VEGF receptor 1 and the extracellular domains 3 and 4 of VEGF receptor 2, which are fused with the Fc part of human immunoglobulin G1[45], whereas aflibercept only contains the extracellular domain 2 of human VEGF receptor 1[46].The efficacy and safety of IVC in the treatment of mCNV has been verified.In a retrospective study in China, 34 mCNV eyes were treated with conbercept and followed up for 12mo.The logMAR BCVA of the patients increased by 4.12±2.69 on average without complications or adverse events[47].As with other anti-VEGF drugs, it can be used as a long-term therapeutic agent for mCNV, although its application is limited at present, especially outside of China.Furthermore, aflibercept has been used previously for the treatment of mCNV, which has also been demonstrated a significant therapeutic effect.Di Antonioet al[48]performed IVA treatment on 15 eyes of mCNV patients and finally found that the patients not only showed improved BCVA but also reduced central retinal thickness significantly, as well as having decreased levels of VEGF and placental growth factor (PIGF).In addition, bevacizumab is a humanized monoclonal antibody (IgG1) targeting VEGF-A to inhibit angiogenesis, and is composed mainly of an Fab region that binds to the target and an Fc region that performs an effector function[49].Fothurmore, ranibizumab is also a humanized monoclonal antibody fragment, but it only contains an Fab fragment, which can also inhibit VEGF-A and prevent the formation of new blood vessels[50].As one of the most commonly used anti-VEGF drugs, ranibizumab,and bevacizumab are used commonly to compare efficacy with each other, but they are considered currently to have the same efficacy in improving visual acuity in mCNV patients without statistical difference[18].Thus, the four kinds of VEGF drugs can effectively inhibit the formation of new blood vessels, effectively providing hope for the treatment of mCNV,however, which drug is best is yet not to be concluded.
In this study, we concluded that in the treatment of mCNV,IVB and IVR are superior to PDT treatment in RCTs.However, combining RCTs and retrospective studies, we found no statistical difference between the four anti-VEGF drugs in improving BCVA, FCT, and CRA.We think this may be due to the fact that these drugs do have the same effect in treating mCNV, or due to factors such as insufficient quantity, data and quality of the original articles, and the treatment time is not long enough.
There are several deficiencies in our study.First, we want to compare the long-term efficacy of different treatments,so we chose 12mo as a follow-up time.However, only the data in retrospective studies met these time conditions of time unification.In the RCTs, there are still two studies with BCVA results followed up for 3 and 19mo, respectively, so,the lack of prolonged treatment might be the reason why the BCVA in mCNV patients did not improve significantly after anti-VEGF treatment compared with other treatments in our results.As for the results of FCT, the data in most articles do not meet the follow-up time of 12mo.Second, we mainly selected the reduction of logMAR BCVA, and FCT as the outcome index, because most of the included articles only included these indexes, and the changes in BCVA and FCT are the most important indexes to evaluate the efficacy of mCNV.We tried to include the number of anti-VEGF injections as the outcome index, but the data included in the study are difficult to meet the extraction of this index.Third, there are too few studies included in this study and the sample size is not large, especially for articles containing LT, there is only one article, which is why most of the results in this study are not statistically significant.In the future, we hope that there will be more appropriate studies, and we will update the data in time to provide more reliable results.
In conclusion, compared to PDT, anti-VEGF is the most effective drug for mCNV patients.Aflibercept may be more effective in improving FCT, while bevacizumab may be better in improving CRA, but this is only a possible conclusion as there is no statistically significant difference in the therapeutic efficacy of the four different anti-VEGF drugs.These conclusions require higher quality and larger sample studies to confirm.
ACKNOWLEDGEMENTS
Authors’ contributions:Wu YJ, writing and modifying manuscripts; Feng YL and Yang JS, independent screening of literature; Fan H, data statistics and chart making; Li WS, the design of the study and guiding the revision of manuscript
Foundation:Supported by 2023 Research Fund of Aier Ophthalmology Research Institute (No.AEI202310LC01).
Conflicts of Interest: Wu YJ,None;Feng YL,None;Yang JS,None;Fan H,None;Li WS,None.
杂志排行
International Journal of Ophthalmology的其它文章
- Dynamic tear meniscus parameters in complete blinking:insights into dry eye assessment
- Effects of diquafosol sodium in povidone iodine-induced dry eye model
- Morroniside ameliorates lipopolysaccharide-induced inflammatory damage in iris pigment epithelial cells through inhibition of TLR4/JAK2/STAT3 pathway
- Role of reactive oxygen species in epithelial-mesenchymal transition and apoptosis of human lens epithelial cells
- Electroacupuncture alleviates ciliary muscle cell apoptosis in lens-induced myopic guinea pigs through inhibiting the mitochondrial signaling pathway
- De novel heterozygous copy number deletion on 7q31.31-7q31.32 involving TSPAN12 gene with familial exudative vitreoretinopathy in a Chinese family
