Observation of peripheral refraction in myopic anisometropia in young adults
2023-12-14YuQinDuYueHuaZhouMingWeiDingMingXuZhangYuJuanGuoShanShanGe
Yu-Qin Du, Yue-Hua Zhou, Ming-Wei Ding, Ming-Xu Zhang, Yu-Juan Guo,Shan-Shan Ge
1Eye School of Chengdu University of TCM, Ineye Hospital of Chengdu University of TCM, Chengdu 610036, Sichuan Province, China
2Beijing Ming Vision and Ophthalmology, Beijing 100010,China
Abstract
● KEYWORDS: myopia; anisometropia; peripheral refraction; multispectral refractive topography; axial length
INTRODUCTION
Myopic anisometropia refers to the difference (≥1 D)in the equivalent spherical diopter between the two eyes of patients with myopia[1].Studies have shown that the frequency and severity of anisometropia escalate with aging and the presence of myopia[2-3], and anisometropia serves as a biomarker for the decreased level of optically controlled ocular growth[4].Anisometropia can lead to a difference in the size of binocular retinal imaging, leading to binocular visual dysfunction such as visual fatigue, amblyopia, and stereopsis dysfunction[5-6].At present, it is believed that myopic anisometropia has differences based on eye structure and binocular development[7].
In recent decades, peripheral refraction has become a popular research topic in myopia prevention and control.Animal experiments and clinical studies suggest that the refractive state in the peripheral retina is strongly associated with the development of myopia[8-9].Multispectral refractive topography(MRT) can quantify the peripheral defocus value of the retina within 53° by successively collecting fundus images with different wavelengths of single spectral light and combining them using a computer algorithm.This method has been found to be accurate, reliable, and reproducible[10-11].
However, few studies have demonstrated differences in refractive status at different retinal eccentricities between more and less myopic eyes in patients with myopic anisometropia.Therefore, the aim of this research was to 1) examine the binocular difference in peripheral refraction of the retina in adult patients with myopic anisometropia with different eccentricity ranges, 2) to explore the correlation between common ocular biometric measurements and peripheral retinal defocus.Our findings may provide a source of reference and theoretical foundation for the selection of personalized optical correction methods for myopic anisometropia and aid in the regulation and management of myopia in teenagers in clinic settings.
SUBJECTS AND METHODS
Ethical ApprovalThis study meets the guidelines of the Declaration of Helsinki and received ethics approval from the Ethics Committee of the In eye Hospital of Chengdu University of TCM (No.2022yh-022).All the participants signed written informed consent.
General InformationIn this cross-sectional clinical study we collected the information of 130 patients with myopia who were seen at In eye Hospital of Chengdu University of TCM between October 2022 and January 2023.The criteria for inclusion were as follows: 1) aged between 18 and 40 years old; 2) binocular myopia; 3) degree of cylindrical mirror ≤3.00 D; 4) stopped using soft contact lenses for at least 2wk and rigid gas breathable contact lenses for 4wk before examination; 5) no history of refractive surgery and corneal diseases.The criteria for exclusion were as follows: 1)participants with eye or major systemic diseases; 2) corrected distance visual acuity <20/25.
Anisometropia is defined as a refractive error difference of at least 1.0 D between the two eyes.Participants were divided into anisometropia and non-anisometropia groups accordingly.In each group, eyes with higher myopic refractive error are referred to as “more myopic eyes” and eyes with lower myopic refractive error are referred to as “less myopic eyes”.
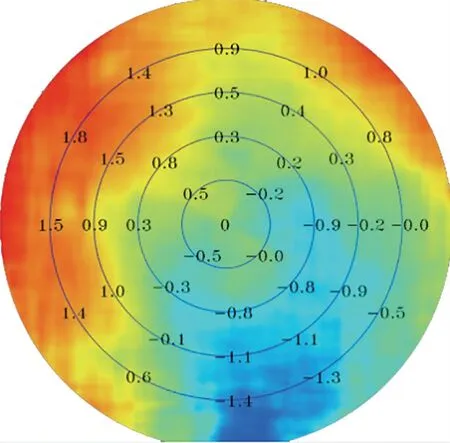
Figure 1 Retinal refraction difference values (RDVs) Results of multispectral refractive tomography: The innermost circle corresponds to RDV-0-10; the first annular region corresponds to RDV-10-20; the second annular corresponds to RDV-20-30; the third annular region corresponds to RDV-30-40; and the fourth annular corresponds to RDV-40-53.Positive RDVs indicate hyperopic defocus,while negative values indicate myopic defocus.
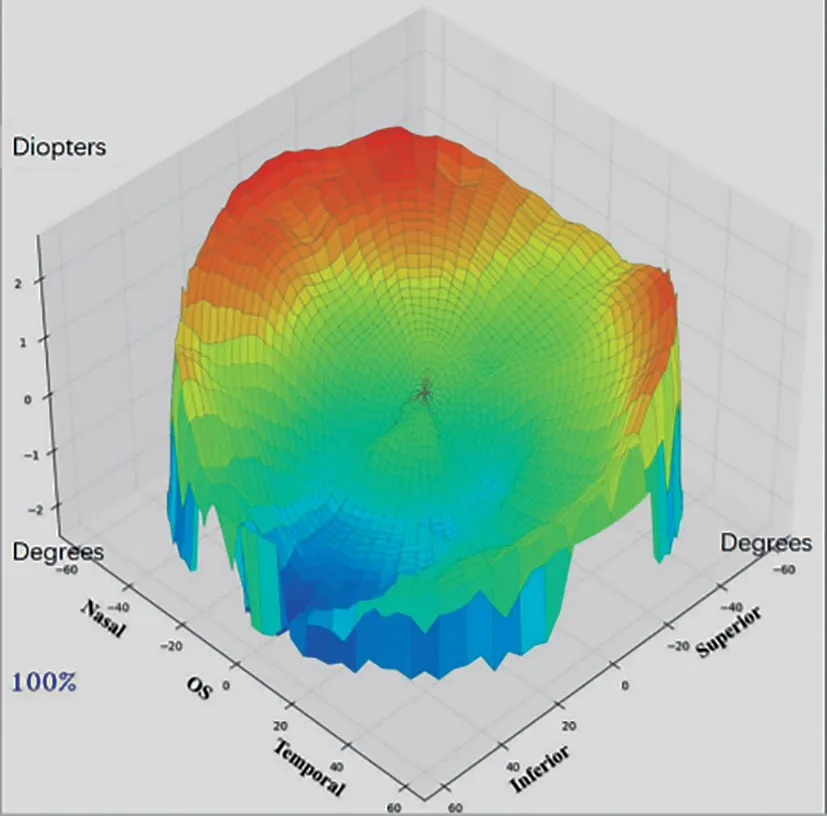
Figure 2 Three-dimensional image of a lefteye showing the relative fraction status of the retina The red area represents hyperopia defocus and the blue area represents myopia defocus.
ExaminationsEach patient underwent visual acuity,intraocular pressure, and the anterior segment of the eye examination.The central corneal thickness (CCT) and axial length (AL) were measured by optical biometry (LS900,Haag-Streit AG, Switzerland).Corneal topography (TMS-4,Tomey, Japan) was used to evaluate the binocular topography,and the surface asymmetry index (SAI), surface regularity index (SRI), steep keratometry (Ks), flap keratometry (Kf),and corneal astigmatism (CYL=Ks-Kf) were recorded.The retinal refraction difference value (RDV) was measured using multispectral refractive topography (MRT, MSI C2000, ShengDa TongZe, ShenZhen, China) at five retinal eccentricities (Figures 1 and 2).From the fovea into 53 degrees(RDV-0-10, RDV-10-20, RDV-20-30, RDV-30-40 and RDV-40-53), the retinal total refraction difference value (TRDV)of 53 degrees, and four regions, including RDV-S (RDV-Superior), RDV-I (RDV-Inferior), RDV-T (RDV-Temporal),and RDV-N (RDV-Nasal).Positive RDV values indicate hyperopic defocus, while negative values indicate myopic defocus.All examinations were performed during the 8:30a.m.to 11:30a.m.time period to avoid diurnal variations in measurements.Examination of spherical equivalent (SE) using cycloplegic refraction.In this study, the refractive power of the participants was measured through computerized optometry,retinoscopy, and subjective optometry.The 0.5% compound tropicamide was utilized for cycloplegias.The SE was calculated as SE=diopter sphere (DS) + 1/2 diopter cylinder(DC).
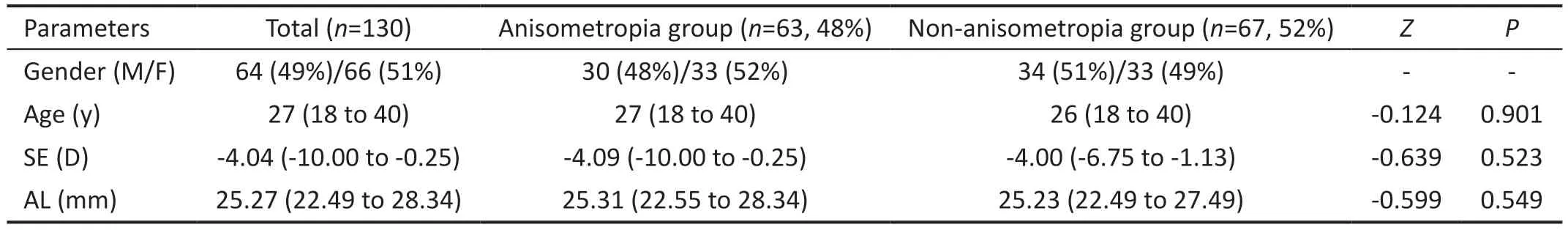
Table 1 The baseline parameters between the anisometropia group and non-anisometropia group

Table 2 The baseline parameters between the less myopic eyes and the more myopic eyes
Sample SizeIn this study, the sample size was calculated using power analysis.We assumed a moderate correlation(Spearman’sr=0.3) between the correlation indicators, a power (1-β) of 90%, and a significance level (α) of 0.05.The minimum sample size was calculated as 112 subjects(anisometropia group, 56; non-anisometropia group, 56).
Statistical AnalysisSPSS 23.0 (version 23.0, SPSS Inc.,Chicago, IL, USA) was used for statistical analysis.Data were analyzed for normality using the Shapiro-Wilk test.For data that were not normally distributed, the Mann-WhitneyUtest was employed to evaluate age, SE, and AL between the anisometropia group and non-anisometropia group, and expressed as median (25thto 75thquartile).If the data were normally distributed, the paired t-test was used to compare binocular baseline and retinal peripheral defocus data between groups.Otherwise, the Wilcoxon rank-sum test was employed.The results are presented as mean±standard deviation (SD).Spearman’s correlation analysis was utilized to examine the relationships between AL, CCT, Ks, Kf, CYL, SRI, SAI,and RDV.The eyes of all participants were included in the correlation analysis.AP-value of<0.05 was deemed to be statistically significant.
RESULTS
Baseline Parameters Between the Two GroupsIn this study, a total of 145 participants were enrolled, of which 15 patients had unsatisfactory images.Hence, 130 participants were eventually enrolled in the study.The anisometropia group included 63 participants (126 eyes), and the non-anisometropia group included 67 participants (134 eyes).The median age in the anisometropia group was 27 (18 to 40)y and it was 26 (18 to 40)y in the non-anisometropia group.The median SE and AL in the anisometropia group was -4.09 (-10.00 to-0.25) D and 25.31 (22.55 to 28.34) mm, and it was -4.00(-6.75 to -1.13) D and 25.23 (22.49 to 27.49) mm in the nonanisometropia group (Table 1).
Binocular Refraction and Ocular Biometric Parameters at BaselineIn the myopic anisometropia group, the differences in SE and AL in the 63 patients’ eyes were statistically significant (Z=-6.906,t=13.072;P<0.001; Table 2), and the SE and AL in more myopic eyes were greater than those in less myopic eyes.There was no significant difference in Ks, Kf,CCT, CYL, SRI, and SAI between the more and less myopic eyes (P>0.05; Table 2).The difference in binocular diopters of the myopic anisometropia group was 2.29±1.25 D.In the non-anisometropia group, the differences in SE and AL in the 67 patients’ eyes were also statistically significant (t=-11.848,3.516;P<0.001;Table 2), and the SE and AL in the more myopic eyes were greater than those in the less myopic eyes.Additionally, there was no significant difference in Ks, Kf,CCT, CYL, SRI, and SAI between the higher and lower eyes(P>0.05; Table 2).The difference in binocular diopters of the non-anisometropia group was 0.26±0.18 D.
RDVs Under Different Eccentricity Ranges in the Anisometropia Group and Non-anisometropia GroupIn the myopic anisometropia group, the RDVs of 63 patients with different eccentricities were compared.The TRDV, RDV-20-53, RDV-S, and RDV-T of the more myopic eyes were significantly higher than those of the less myopic eyes, and the differences were all statistically significant (P<0.05; Table 3,Figure 3).In the myopic non-anisometropia group consisting of 67 patients, there was no significant difference in any of the RDVs between the more and less myopic eyes under different eccentricities (P>0.05; Table 3, Figure 3).
Relationship Between RDVs at Different Eccentricities,Myopic Diopters, and Ocular Biological ParametersSpearman’s correlation analysis showed that SE was negatively correlated with TRDV (r=-0.205,P=0.001), RDV-20-53 (r=-0.281, -0.183, -0.176,P<0.05), RDV-S (r=-0.251,P<0.001), and RDV-T (r=-0.230,P<0.001).The AL was positively correlated with RDV-20-30 (r=0.164,P=0.008)and RDV-T (r=0.160,P=0.010).The CYL was negatively correlated with RDV-10-30 (r=-0.147, -0.180,P<0.05), and SRI was negatively correlated with RDV-0-20 (r=-0.190,-0.170,P<0.05).Ks, Kf, CCT, and SAI were not correlated with the RDV (P>0.05; Figure 4).
DISCUSSION
Anisometropia is a worldwide public health problem.The prevalence of anisometropia has been estimated to vary between 1.6% and 35.3% across different age groups and nations[12], and several studies have demonstrated that the prevalence of anisometropia is higher in children and adolescents, and it may be associated with the development of myopia.However, this is relatively stable in adulthood,which may be related to the stability of the adult refractive state[13].The causes of anisometropia are related to the different growth rates of the binocular axial length in the process of binocular emmetropia in childhood[1].Additionally, the degree of anisometropia is positively correlated with the diopter of myopia and the difference in binocular axial length, thus, with the increase in myopia diopter, the amount of anisometropia also increases[14-15].
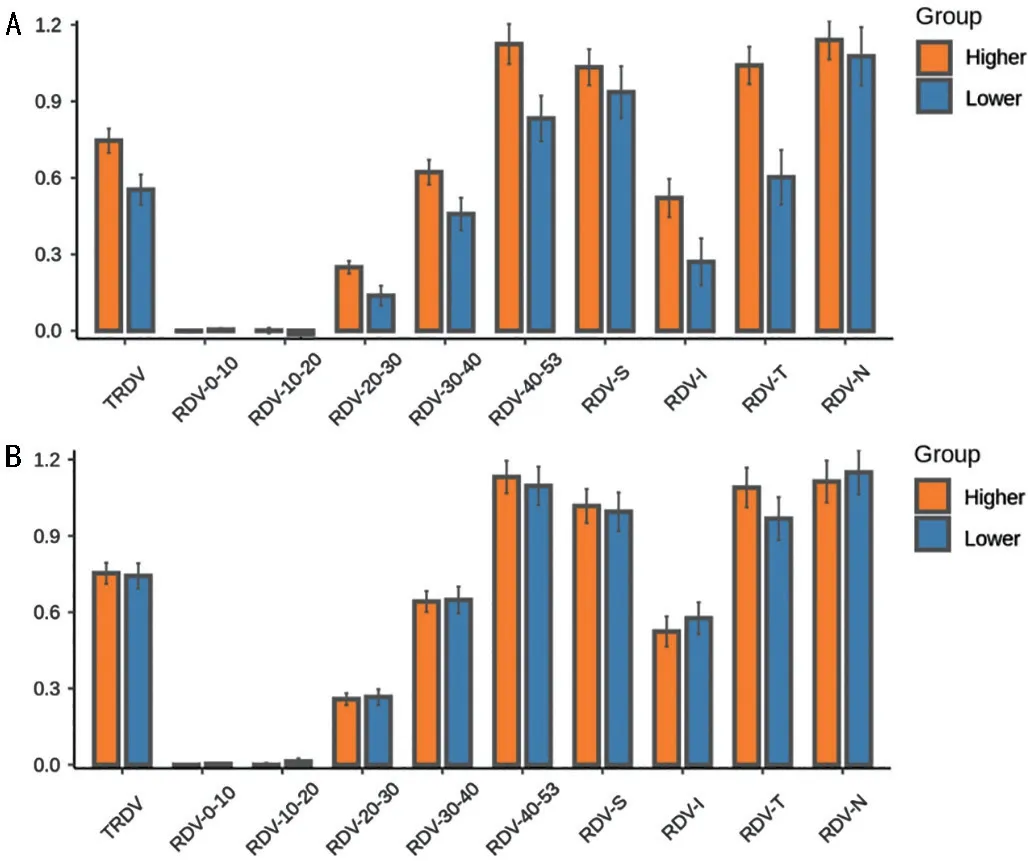
Figure 3 Comparison of RDVs in the myopic anisometropia group(A) and non-anisometropia group (B) under different eccentricities between the more and less myopic eyes RDV: Refraction difference value; RDVs at five retinal eccentricities, from the fovea to 53 degrees recorded as RDV-0-10, RDV-10-20, RDV-20-30, RDV-30-40, and RDV-40-53.TRDV: Total RDV; RDV-S: RDV-superior; RDV-I: RDV-inferior;RDV-T: RDV- temporal; RDV-N: RDV-nasal.
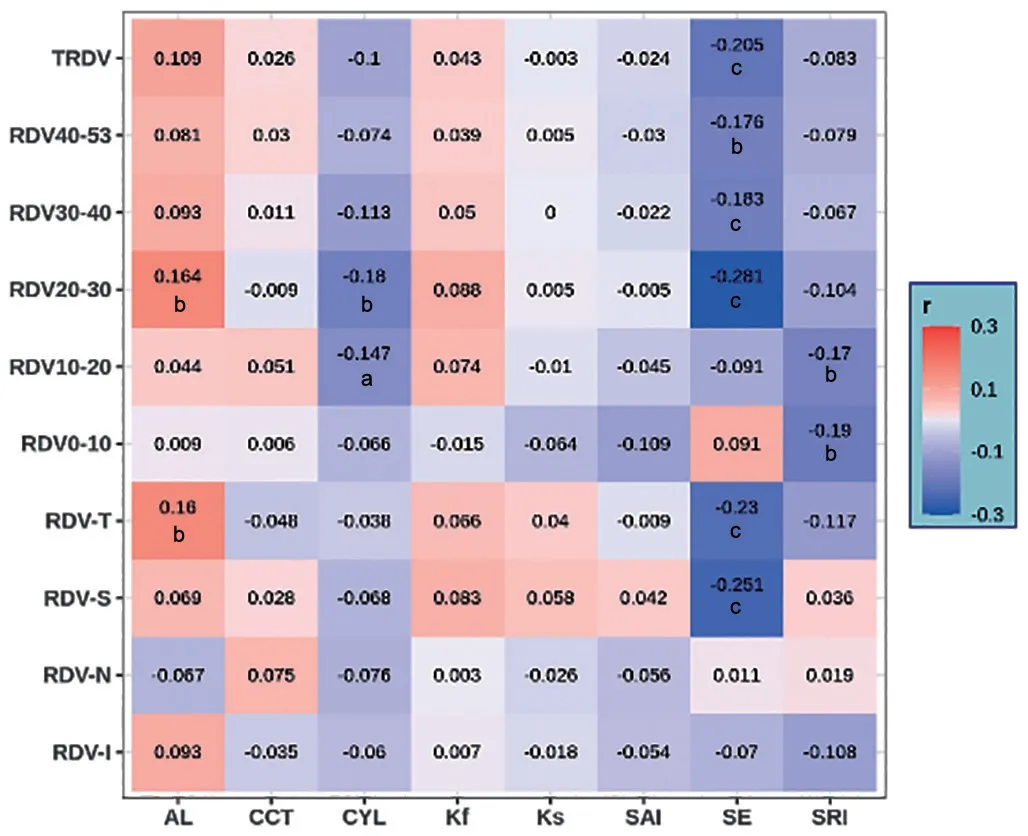
Figure 4 Correlation analysis of RDV with diopter and ocular biometric parameters under different eccentricities (Spearman’s correlation analysis) RDV: Refraction difference value of the retina;RDVs at five retinal eccentricities, from the fovea to 53 degrees recorded as RDV-0-10, RDV-10-20, RDV-20-30, RDV-30-40, and RDV-40-53; TRDV: Total RDV; RDV-S: RDV-superior; RDV-I: RDV-inferior;RDV-T: RDV-temporal; RDV-N: RDV-nasal.AL: Axial length; CCT: Central corneal thickness; CYL: Corneal astigmatism; Kf: Flap keratometry;Ks: Steep keratometry; SAI: Surface asymmetry index; SE: Spherical equivalent; SRI: Surface regularity index.aP<0.05, bP<0.01, cP<0.001.
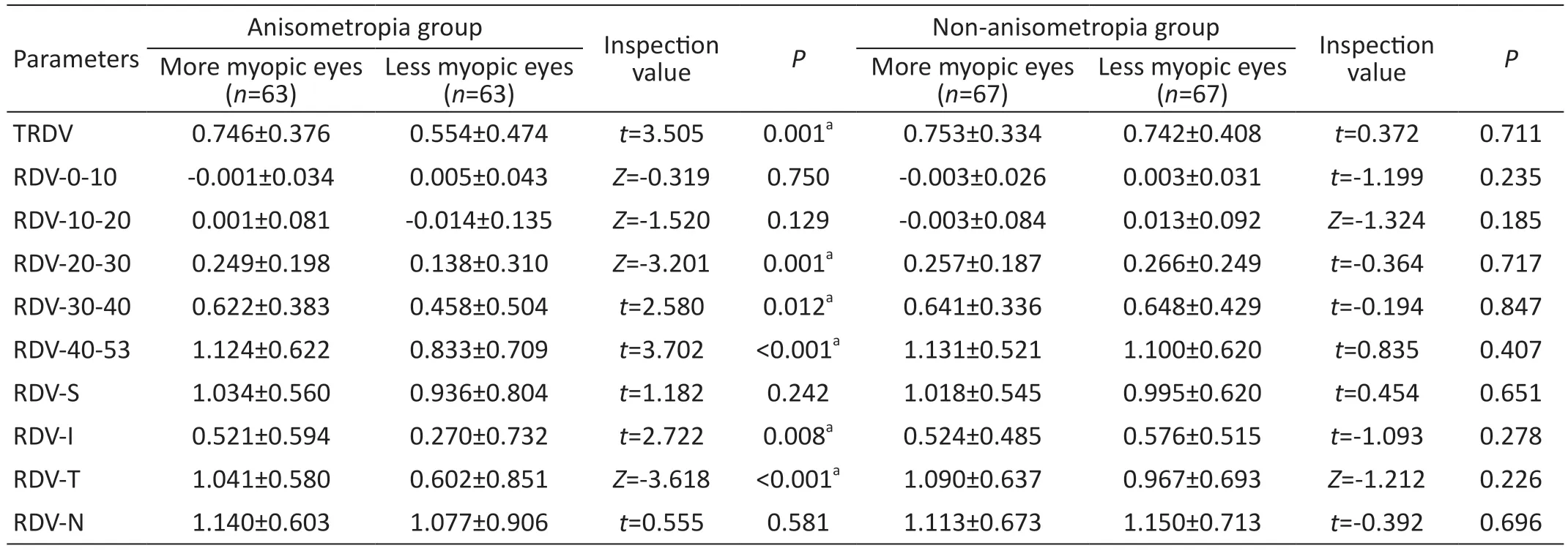
Table 3 Comparison of RDVs between the less myopic eyes and the more myopic eyes
Peripheral defocus refers to the refractive error state of the peripheral retina; the optics of the eye and the shape of the retina both contribute to the peripheral refraction of the retina[16].Defocus of the peripheral retina also plays a significant role in controlling the growth of the eye and it may be related to defocusing-induced changes in choroidal thickness[17].Benavente-Pérezet al[18]used +5 D and -5 D bifocal contact lenses were used to induce hyperopia and myopic defocus on the peripheral retina of marmosets,respectively, and found that modifying the refractive state and eye growth can be achieved by manipulating peripheral retinal defocus.Smithet al[9]also found that when the defocused signals around the retina and the center contradict, the defocused signals around the retina occupy a dominant position in the process of eye growth and development.Wallman and Winawer[19]pointed out that the refractive state of the peripheral retina exerts a stronger influence on ocular growth and refractive development than the refractive state of the macular central fovea, primarily because there are more optic nerve fibers in the peripheral retina than in the central region.When the retina receives visual signals both from the central and peripheral retina, signals from the numerous neurons in the peripheral retina may suppress the signals from the central retina, thereby directly influencing refractive development and ocular growth.In addition, Zhonget al[20]labeled focussensitive retinal neurons (bipolar cells and amacrine nerve cells ) with immunocytochemical markers after altering the quality of visual images in infant monkeys and found that visual neurons are more susceptible to hyperopic defocus than myopic defocus signals.It is inferred that differences in the distribution and sensitivity of these visual neurons may be important factors in the different responses of the retina to peripheral defocus in different regions, with different impacts on ocular growth.Understanding the relationship between central refraction and peripheral retinal defocus has important implications for the control of myopia.
It has been shown that the refractive condition of the peripheral retina varies with central refraction, that myopic children and adults usually show more hyperopic defocus in the peripheral retina, and that the degree of hyperopic defocus in the peripheral retina increases with axial myopia[21-23].Findings of the current study are similar to those of the aforementioned studies.Specifically, we discovered that the myopic eyes in both groups were relatively hyperopic defocused in the range of 20-53 retinal eccentricity, and the value of RDV increased with the increase in eccentricity;in this study, a negative correlation was also found between SE and TRDV, RDV-20-53, RDV-T.Zhenget al[21]found a positive correlation between AL and RDV-20-45 through MRT in 241 young patients with myopia and found that AL is an independent risk factor for retinal defocus within the range of 20-35 eccentricity.In our study, we found that AL was positively correlated with RDV-20-30 in patients with myopic anisometropia.We speculated that the retinal defocus of 20-30 eccentricity range may stimulate the growth of AL, which is a crucial element that impacts the emergence and progression of myopia.
In the myopic anisometropia group in the present study,the TRDV, RDV-20-53, RDV-S, and RDV-T of the more myopic eyes were significantly higher than those of the less myopic eyes.This is evidenced by the absence of a significant difference in peripheral retinal defocus between the more and less myopic eyes under different eccentricities in the nonanisometropia group.The results showed that when the diopter difference of both eyes was greater than 1.0 D, the difference in peripheral retinal defocus was different in both eyes.Conversely, when the difference in binocular diopter was less than 1.0 D, the difference in binocular retinal defocus was not significant.Clinical studies have found that orthokeratology,defocus soft, defocus frame, and multifocal soft lenses reduce the defocus of peripheral hyperopia through refractive correction and thus control the progress of myopia[24-28].Personalized selection and customization of binocular myopia prevention and control tools are particularly important.Due to the significant difference in peripheral retinal defocus in both eyes of patients with myopic anisometropia, is it possible to customize myopia control tools based on the original peripheral retinal values of more and less myopic eyes to better help teenagers with myopic anisometropia in myopia control.This will be the direction of future research.
There was a negative correlation between CYL and RDV-10-30, suggesting that with the increase of corneal astigmatism,the value of retinal defocus in the range of 10-30 eccentricity will also increase.The SRI is used to evaluate the refractive power distribution of 256 radial lines within the diameter of 4 mm in the central area of the cornea.It is mainly used to assess the regularity of the cornea.The more regular the corneal surface, the lower the SRI.There was a negative correlation between SRI and RDV-0-20 in the present study,suggesting that the regularity of the central corneal region has a certain impact on the retinal defocus in the range of 0-20 eccentricity.Therefore, the diopter and corneal morphology of the eye may affect the peripheral defocus of the retina.Due to the limitations of sample size and diopter distribution in this study, a complex regulatory relationship may exist between myopia, corneal morphology, and retinal peripheral refraction;thus, further studies with a larger sample size and longer duration are needed.Moreover, due to the small sample size,further grouping was not carried out according to the severity of anisometropia.
In conclusion, patients with myopia show peripheral hyperopic defocus, and the peripheral retinal defocus values of both eyes in myopic anisometropia patients are significantly different.These results serve as a reference and theoretical foundation for the selection of personalized optical correction methods for myopic anisometropia in clinic settings.They also provide new ideas for behavioral interventions for myopia prevention and control in adolescents with myopic anisometropia.
ACKNOWLEDGEMENTS
Conflicts of Interest: Du YQ,None;Zhou YH,None;Ding MW,None;Zhang MX,None;Guo YJ,None;Ge SS,None.
杂志排行
International Journal of Ophthalmology的其它文章
- Dynamic tear meniscus parameters in complete blinking:insights into dry eye assessment
- Effects of diquafosol sodium in povidone iodine-induced dry eye model
- Morroniside ameliorates lipopolysaccharide-induced inflammatory damage in iris pigment epithelial cells through inhibition of TLR4/JAK2/STAT3 pathway
- Role of reactive oxygen species in epithelial-mesenchymal transition and apoptosis of human lens epithelial cells
- Electroacupuncture alleviates ciliary muscle cell apoptosis in lens-induced myopic guinea pigs through inhibiting the mitochondrial signaling pathway
- De novel heterozygous copy number deletion on 7q31.31-7q31.32 involving TSPAN12 gene with familial exudative vitreoretinopathy in a Chinese family
