How long does the recovery of corneal sensitivity in different corneal regions take after LASEK?
2023-12-14AliMirzajaniAriaBouyehFatemehKhezriEbrahimJafarzadehpurFaridKarimian
Ali Mirzajani, Aria Bouyeh, Fatemeh Khezri, Ebrahim Jafarzadehpur, Farid Karimian
1Rehabilitation Research Center, Department of Optometry,School of Rehabilitation Sciences, Iran University of Medical Sciences, Tehran 1449614535, Iran
2Ophthalmic Research Center, Research Institute for Ophthalmology and Vision Science, Shahid Beheshti University of Medical Sciences, Tehran 1983963113, Iran
Abstract
● KEYWORDS: refractive surgery; laser-assisted subepithelial keratectomy; corneal sensitivity; ablation depth;refractive error
INTRODUCTION
Refractive surgery using an excimer laser is one of the most common treatments for refractive errors; as a result, the number of people undergoing these surgeries has significantly increased recently[1].Several types of refractive surgeries demonstrated that laser-assisted subepithelial keratectomy (LASEK) could be considered a relatively new one in this category, which Camellin[2]introduced in 1999 for the first time.This surgical procedure combines some aspects of both laser-assistedin situkeratomileusis (LASIK)and photorefractive keratectomy (PRK), providing an improved benefit/risk ratio.It is precious in patients with thin corneas who would not qualify for LASIK surgery.LASEK is known for long-term stable results and the lack of serious complications, including infections, scars, recurrent erosions,or late-onset corneal haze formation[3].Therefore, some surgeons still prefer LASEK most of the time[4].
The cornea is a vein-free transparent optical tissue considered the most sensitive tissue of the human body, and the density of corneal nerve terminals is 300 times more than that of skin.The corneal nerves pathway originates from the long ciliary nerves of the ophthalmic branch of the trigeminal nerve.These nerves are myelinated while entering the limbus horizontally,and then they form the nerve bundles, which are only covered by Schwann cells and this lack of myelin in the central corneal axons is critical to maintaining corneal transparency[5].Initially,these nerves are located in the middle third of the stroma and then branch to the anterior surface of the cornea, forming a sub-basal sensory network[6]in which nerve endings are sent to epithelial cells and innervate them[7].
The epithelium and, to a lesser extent, endothelium need the natural sensitivity of the cornea to work properly.Corneal hypoesthesia can have adverse effects on the cornea, including the decreased wound-healing ability of the epithelium[8],reduced blink rate, and impaired mitotic rate of the cornea.Hence, a delayed healing process of epithelial ulcers can lead to neurotrophic keratitis, infectious keratitis[9], and severe dry eye[10].In LASEK, the alcoholic solution is used to remove the corneal epithelium, creating an epithelial flap that is replaced after laser ablation[11].LASEK can disrupt subepithelial nerve fiber bundles and nerves in the cornea’s anterior stroma[12].Refractive surgery complications have always been a critical issue; therefore, many studies have been conducted in this field.Corneal sensitivity is one of the most vital parameters affected by all types of refractive surgeries.Due to the importance of this issue, the recovery time of corneal sensitivity after various types of refractive surgeries has always been one of the most important questions discussed by researchers in recent years.A variety of methods to measure corneal sensitivity was available.The most common one is the Cochet-Bonnet aesthesiometer[13].
Few studies are available regarding the recovery of corneal sensation after the LASEK, and the results have been somewhat contradictory.For example, Hermannet al[12]reported this duration as 1mo, while Wuet al[14]and Horwath-Winteret al[15]reported it as 3mo.
Although refractive surgeries damage corneal nerve fibers,understanding the effects of these surgeries on corneal sensitivity and its recovery time is crucial.Some critical factors,such as the importance of corneal sensitivity, the prevalence of LASEK refractive surgery, the limited number of studies in this field, relatively small sample sizes in previous studies,uncertain results of them, and some defects related to their inclusion criteria (such as age range and using contact lenses before operation), provoked us to design and run the present study.The present study aimed to investigate the duration of the corneal sensitivity recovery process in different regions after LASEK and to discover the effects of ablation depth on it.
SUBJECTS AND METHODS
Ethical ApprovalBefore commencing the study, approvals were obtained from the Ethics Committee of Iran University of Medical Sciences (approval code: IR.IUMS.REC.1398.881),and the study was conducted according to the tenets of the Declaration of Helsinki.Informed consents were obtained from all subjects after an explanation of the nature of the study.This study was a quasi-experimental study that included cases aged 20 to 35 with an average of 22.26±3.8y, of which 34 (37.8%) were male and 56 (62.2%) were female.The current study was conducted at Negah Ophthalmology Hospital in Tehran, Iran, from September to December 2022.Inclusion criteria included myopia -1.00 to -7.00 diopters (D),astigmatism less than 2.00 D, having the necessary conditions for LASEK regarding thickness and other corneal parameters,and no history of wearing contact lenses and aged 20 to 35y(according to the fact that corneal sensation decreases with aging that could overshadow it)[16]that all of them were thoroughly examined by the project optometrist.In addition,candidates for LASEK refractive surgery who met the inclusion criteria were enrolled in this study after explaining the study principles, goals, and methods and obtaining informed written consent.The individuals then filled in the demographic information questionnaire, and their preoperative refraction was added to their forms based on their hospital records.Then, the project ophthalmologist examined the participants’ history of any ocular surgery or trauma, diabetes and connective tissue diseases, neurological diseases, corneal disease, and glaucoma history.If any of mentioned disorders were reported or subjects were reluctant to participate, they would be excluded from this study.
In the next step, on the day of the operation, before entering the operating room and using the eye drops, including anesthetic drops, the corneal sensitivity of the cases was measured with Cochet-Bonnet esthesiometer (Luneau Ophthalmology, Paris,France).Preoperative measurements were performed on 170 individuals.In the second time point of measurements, 140 of them continued the examinations 1mo after the operation.Subsequently, in the third time point of measurements, 90 participants attended for the third time 3mo after the operation,and their corneal sensitivity was measured.Therefore, in general, this study was performed on 90 right eyes of 90 participants.The preoperative refractive error ranged from-0.75 to -7.00 with an average of -3.63±1.5 D.The mean ablation depth was 60.34±21.6 μm ranging from 21 to 108 μm.The diameter of the ablation zone was the same for all individuals, equal to 6 mm.Besides, to investigate the effect of the ablation zone depth on the recovery of corneal sensitivity, the ablation depth was divided into three groups:low (21-50 μm), moderate (50-81 μm), and high (>80 μm)in which, there were 28, 46 and 16 eyes in each group,respectively.
Corneal EsthesiometerEsthesiometer is the most common instrument for measuring corneal sensitivity, which consists of a nylon monofilament with a diameter of 0.12 mm2but of variable lengths ranging from 5 to 60 mm.By changing the size of the thread from maximum to minimum, the pressure applied to the surface of the cornea changes from 5 to 180 mm/g·s, respectively.Notably, in esthesiometry, humidity and temperature could change the thread length.Consequently,the esthesiometer must be stored in the environmental conditions of the test site for 12h before the examination.The corneal sensitivity measurement in this design was performed according to the instructions in the manual so that while the person was sitting and looking straight ahead, the esthesiometer approached close to the cornea perpendicularly until the touch was made.Observing any curvature in the thread was a sign of its contact with the cornea’s surface.As Larson[17]pointed out in his study, while using this device, to compensate for the curvature of the thread due to its weight, the head of the esthesiometer should be held slightly upwards.Therefore, in this study, we moved the bottom of the esthesiometer body slightly downward because of the curvature in the thread and providing the perpendicular position.If the person could feel this touch, a positive response was considered, and the thread length was recorded as the preoperative corneal sensitivity.In contrast, if they did not feel the touch, the thread length was decreased, in 5 mm increments, until a positive response was acquired.In this device, as the length of the monofilament decreases, the amount of pressure on the cornea will increase.In the present study, measurements were repeated three times for each corneal region at each step, and their average was recorded as the region’s sensitivity.In cases where they could not control their reflexive blinking while esthesiometry,the upper eyelid was held by a hand.Besides, blinking was allowed between different measurements to prevent the eye from drying out.For each person, the esthesiometer thread was disinfected with 70% alcohol at the end of the measurement procedures according to the instructions in the manual to be ready for the subsequent measurement.
Corneal sensitivity was measured in five regions: central,superior, inferior, nasal, and temporal.Mid-peripheral regions were measured at a distance of 2 mm from the center (within the surgery zone).Correspondingly, based on the studies,because of the variability of the corneal sensitivity at different times of the day[18], all pre-and postoperative measurements were performed between two and 5p.m.In the current study,esthesiometry was performed at 3-time points, first in the preoperative time point and then 1 and 3mo after LASEK.Notably, all the clinical examinations and those three steps of esthesiometry were performed by the same skilled and experienced optometrist to prevent any possible bias in a stable environment with a temperature of 18℃ and a humidity of about 15%.
Statistical AnalysisAll data were analyzed using SPSS software version 26 (SPSS Inc., Chicago, Illinois, USA).Initially, descriptive analyses were performed.Then, in the analytical statistics section, Repeated Measure Analysis of Variance (Repeated Measure ANOVA) tests were performed to investigate the effects of time and corneal regions on the recovery of corneal sensitivity.Since Mauchly’s test of sphericity represented that the assumption of the equality of variances was violated for the duration and corneal regions parameters (χ2=91.01,P=0.000 andχ2=24.59,P=0.003 for duration and corneal regions, respectively), the Greenhouse-Geisser correction was used in the analysis of variance(ANOVA) test to adjust the degree of freedom.Also, paired samplet-test was used to compare preoperative corneal sensitivity with each of the postoperative examinations in 1 and 3mo after LASEK to determine the duration of corneal sensation recovery to its preoperative levels.In addition, to compare the sense of five measured corneal regions at each time point of measurement and to compare the effects of three different categories of ablation depth on reducing the sense of five measured corneal regions in 1mo after surgery, one-way ANOVA was used.Furthermore, in both mentioned cases, the LSD (post hoc) test was used to compare the values in pairs.
RESULTS
Investigating the primary and combined effects of time and corneal region on the recovery of corneal sensitivity revealed that time significantly affects the recovery of corneal sensitivity after LASEK (F=30.6,P<0.000), which means that corneal sensitivity is different in pre-and postoperative measurements.Besides, an interaction was found between time and corneal regions, which means that corneal sensitivity changes in different regions of the cornea are not the same,and a statistically significant difference was observed between them (F=8.64,P<0.000).
Comparison of the Mean Values of Three Measured Time Points in Five Different RegionsAccording to a statistically significant difference (P<0.05) was found comparing the level of corneal sensitivity in the preoperative time point to 1 and 3mo after the operation in all five corneal regions, meaning the corneal sensitivity in five regions,i.e., center, nasal, inferior,temporal, and superior at 1mo postoperatively did not reach its preoperative values yet, whereas no significant difference was found between the preoperative and 3mo postoperative time points (P>0.05; Table 1).This issue indicates that within 3mo after the operation, the process of improving corneal sensation was completed and reached the preoperative values.Notably,the highest level of corneal sensitivity in both before surgery and 3mo after surgery, when corneal sensitivity values returned to preoperative values in all regions, was related to the center of the cornea (Table 2).
Comparison of the Mean Values of Five Different Regions in Three Measured Time PointsThe investigation of the differences between the corneal sensation values of the five measured regions showed that in both preoperative and 3mo after the operation, when the corneal sensitivity almostreached the preoperative values, a significant difference was observed between corneal sensitivity at different points(F=3.58,P=0.007 for preoperative andF=3.83,P=0.004 for 3mo postoperative; Table 2).Also, comparing the values of these regions in each of these two times showed that the center of the cornea had a significantly higher sensitivity than the nasal, inferior, temporal, and superior mid-peripheral regions (P<0.05).Thus, no statistically significant difference was observed between the sensation of the nasal, inferior,and temporal regions (P>0.05).Notably, in both times, the highest sensation was related to the center of the cornea, and the lowest was related to the superior of the cornea.Also, in the second time point of corneal sensitivity measurement,1mo after the operation, no significant difference was found between the sensitivity of the five measured corneal regions(F=0.31,P=0.86).
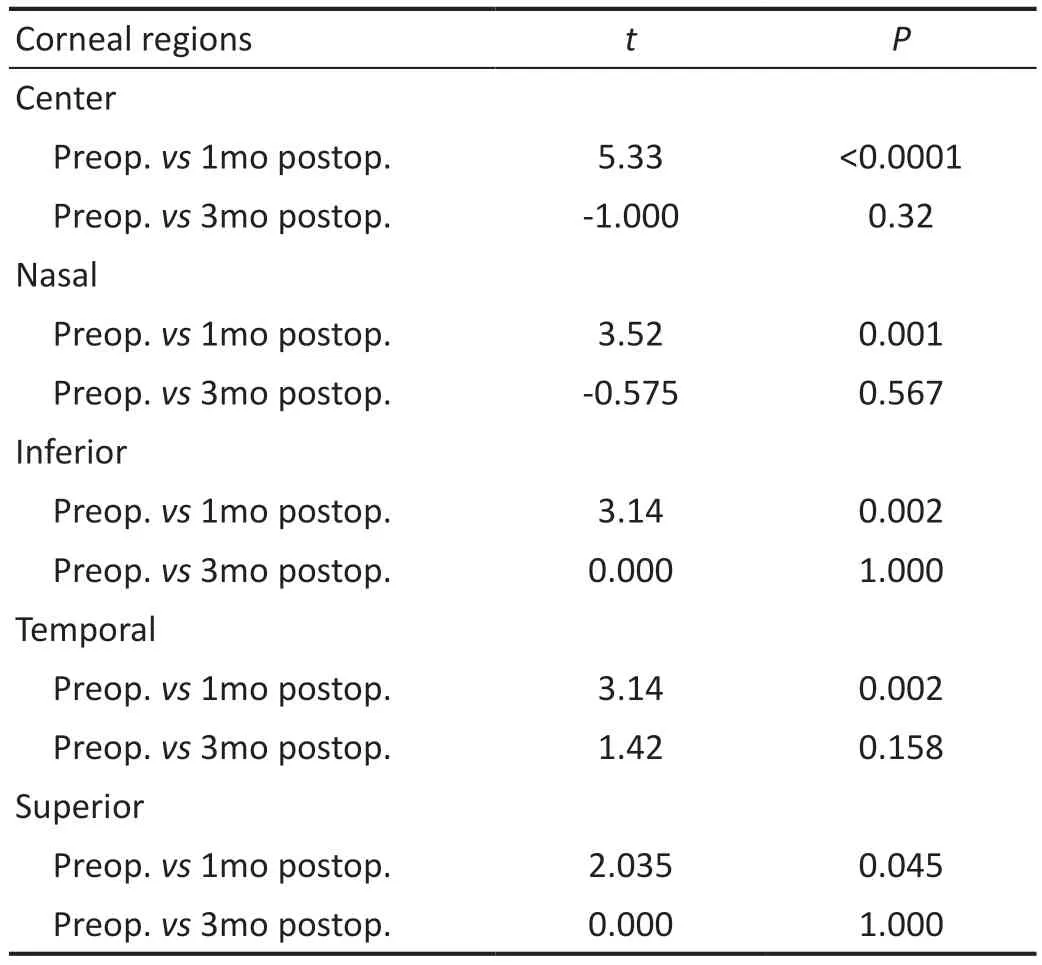
Table 1 Comparison between preoperative and 1 and 3mo postoperative corneal sensitivity in five different corneal regions

Table 2 Mean sensitivity of five corneal regions values in three measured time mean±SD
Comparing the sensation loss in five measured corneal regions 1mo after surgery showed a statistically significant difference between decreased corneal sensitivity in different corneal regions (P=0.000,F=7.35).Accordingly, a statistically significant difference was found between the amount of sensation loss in the center and other measured points of the cornea (P<0.05), and no significant difference was observed between corneal sensitivity reduction in nasal,inferior, temporal, and superior regions (P>0.05).Therefore,according to the results, the most corneal sensitivity reduction is related to the center of the cornea, and the highest amount of preoperative corneal sensitivity was also related to this region.
Effect of Ablation Depth on the Recovery of Corneal SensitivityThe investigation of the ablation depth effect on the recovery of corneal sensitivity at 1mo postoperatively represented that in terms of corneal sensitivity reduction among the three different groups of ablation depth, a statistically significant difference was found in the central region, as well as the temporal region of the cornea (F=13.65,P=0.000;F=7.81,P=0.001 for the central and temporal regions of the cornea,respectively), while in the other three regions of the cornea,i.e.,nasal, inferior, and superior regions, no statistically significant difference was found among the three different ablation depth categories (F=1.99,P=0.14;F=1.79,P=0.17;F=2.59,P=0.08 for nasal, inferior, and superior regions, respectively; Table 3).
DISCUSSION
The corneal sensation is one of the invaluable signs of corneal healthiness, so the problematic corneas are usually lower sensitive[5].Refractive surgeries, such as LASEK, directly affect the corneal nerves and the nerve terminals within the operation zone[19].Since the cornea is the body’s most sensitive tissue, it is vital to determine the recovery time of corneal sensation after various kinds of refractive surgeries.The extent of corneal sensation loss and its recovery duration depends on several factors, including the type of refractive surgery, the corneal manipulation zone, and the corneal nerve number in the operated region.
The results obtained from the present study contain some significant issues in which previous studies had contradictions with these results.In the present study, the post-LASEK corneal sensitivity was measured at five different regions,which has only been done in a few previous studies.In this regard, one of this study’s key findings, which had not been reported before, is that the sensitivity of the center of the cornea, which was more significant than other measured midperipheral points (nasal, temporal, superior, and inferior)before the surgery, had the most significant decrease 1mo after the surgery.Although 1mo after surgery, the amount of central corneal sensation was not significantly different from the four mid-peripheral points (P>0.05).However, 3mo after LASEK,when the central corneal sensitivity returned to its preoperative value, its sensitivity was significantly higher than other points.

Table 3 The average of decrease in corneal sensitivity with the standard deviation values in 1-month interval after operation in five corneal regions in three different groups of ablation depth and comparing the effect of ablation depth in reduction of corneal sensitivity in the five corneal regions
Since no significant difference was found between the reductions of corneal mid-peripheral points 1mo after surgery,previously, this issue has only been studied in the study of Herrmannet al[12].In their study, the same as this research,the corneal sensitivity of myopic individuals were examined in five different regions,i.e., center, nasal, inferior, temporal,and superior at a distance of 2 mm from the center in the preoperative and 1, 3, and 6mo after the operation.According to their findings, the sensation of different regions of the cornea 1mo after LASEK is the same, consistent with this study in this respect.However, they also reported that the sensation of different cornea regions was equal to each other 3 and 6mo after the operation, which contradicts the current study’s results.Reportedly, the extent of corneal sensitivity changes in the different regions of the cornea was not different from each other after LASEK.Remarkably, a significant decrease in the sensitivity of the central cornea after surgery could be justified because LASEK has been performed on individuals with myopia refraction.Hence, with the ablation of the central part of the cornea, the central nerves were affected more than other parts.
Nevertheless, in regards to the difference between the results of the two studies can illustrate that in the study of Hermannet al[12], no significant difference was found in the mean sensitivity of different regions of the cornea in the preoperative time point, which may be due to the history of wearing contact lenses by most of the individuals before the operation.Moreover, it could bring the sensation of different parts of the cornea closer to one another[20], while the present study did not include cases with a history of contact lens usage.On the other hand, this issue can be attributed to the difference between the number of samples and the types of sample selection.As in the study of Herrmannet al[12], 40 eyes of 20 cases were examined,which means that both eyes were evaluated.This issue can have overshadowed the results and statistical analytics and led to errors.In the present study, evaluations were performed on the right eyes of 90 patients to eliminate the effects of possible errors so that it could illustrate the differences between the improvement rates of corneal sensation in five corneal regions more clearly.Markedly, the least amount of corneal sensitivity before surgery and the least amount of changes in corneal sensitivity after surgery was related to the superior part of the cornea.This may be due to the effect of the upper eyelid because the upper part of the cornea has the most contact compared to the other parts of the cornea.Besides, this can lead to an increase in the threshold of nerve sensitivity and, as a result, intermittent desensitization of this area over time[18].
Some studies have rejected the relationship regarding the effect of ablation depth or amount of myopia refractive error before surgery on the recovery of corneal sensation in LASEK[12].In contrast, some have reported the existence of this relation significantly[14].Also, concerning similar studies on other types of refractive surgeries, various results have been mentioned in this field.Although some studies have shown that if the preoperative refractive error was in the low-medium range, the depth ablation would not interfere with determining corneal sensitivity recovery[21], some studies have shown a significant relation conversely[22].In general, this study’s results in response to this duality indicate that the ablation depth is effective on recovering corneal sensitivity in the temporal region and the center of the cornea.A close relationship was observed between the ablation depth and damage to the corneal nerves, primarily in these parts.To justify this issue, it could be considered that at the more significant depth of ablation, the intraepithelial nerves, the sub-epithelial plexus, and the deeper and larger trunks of the corneal nerves, which are just below the sub-epithelial plexus are also damaged.Consequently, it could lead to a further reduction in corneal sensation.The fact that the depth of ablation in the center of the cornea affects the recovery of corneal sensation, depends on the corneal ablation pattern in refractive surgery.In the present study, surgery was performed on myopic individuals.Therefore, more corneal tissue was photo ablated in the center of the cornea than in the mid-peripheral regions, and more corneal nerves were destroyed there.As a result, the corneal sensation in the center of the cornea is reduced to a greater extent than in the midperipheral regions.
Another significant evaluation of this study was related to the duration of corneal sensation recovery time when corneal sensitivity returned to its preoperative level.In the present study, corneal sensation reduced significantly 1mo postoperatively.Conversely, 3mo after the operation, the sensation of all five measured points of the cornea had returned to its preoperative values.These findings are consistent with the results of studies by Wuet al[14], Darwishet al[23], and Horwath-Winteret al[15].At the same time, it is different from the results of Herrmannet al’s study[12], which reported it 1mo or Leeet al[24], who reported six months.Notably, as mentioned earlier, 85% of their cases had used soft and hard contact lenses to justify the reason for the difference in the recovery of corneal sensitivity period in the present study compared to Herrmannet al’s study[12].Perhaps the allocated time for the washout of this effect was not enough in the study.Therefore, the measured amount of corneal sensitivity before the operation was less than the actual value.As a result, the operation returned to the preoperative underestimated values in a shorter period.On the other hand, concerning the study of Leeet al[24], which reported six months as the recovery period of corneal sensitivity, the reason for this difference can be attributed to the higher mean of preoperative refractive error in their research compared to the present study (-4.93±2.93 D in Leeet al’s study[12]compared to -3.63±1.5 D in the present study).As some studies have shown[25-26], and the results of this study confirmed, the amount and duration of corneal sensitivity reduction after refractive surgery can be related to the ablation depth.Since the amount of preoperative refractive error in Leeet al’s study[24]was more than in the present study,logically, the mean depth of ablation in their study has also been more than in the present study.So, the more extended period of corneal sensitivity recovery time in their study may be due to this fact.
Generally, due to the fact that variations of corneal sensitivity following LASEK are dependent on various factors, the small number of corneal sensitivity measurements cannot show nuances.Therefore, it is recommended that examinations with shorter time intervals be done in future studies.
In conclusion, according to the present study’s results on individuals with myopia and low astigmatism, corneal sensitivity decreases after LASEK, in which the most significant amount of corneal sensitivity reduction is related to the center of the cornea and reaches the preoperative levels within 3mo after surgery.Besides, the depth of ablation and the measured region of the cornea are two main factors that effectively investigate improving the corneal sensitivity after LASEK.
ACKNOWLEDGEMENTS
The authors wish to thank the participants and the staffof Negah Ophthalmology Hospital, Tehran, Iran for their cooperation.
Conflicts of Interest: Mirzajani A,None;Bouyeh A,None;Khezri F,None;Jafarzadehpur E,None;Karimian F,None.
杂志排行
International Journal of Ophthalmology的其它文章
- Dynamic tear meniscus parameters in complete blinking:insights into dry eye assessment
- Effects of diquafosol sodium in povidone iodine-induced dry eye model
- Morroniside ameliorates lipopolysaccharide-induced inflammatory damage in iris pigment epithelial cells through inhibition of TLR4/JAK2/STAT3 pathway
- Role of reactive oxygen species in epithelial-mesenchymal transition and apoptosis of human lens epithelial cells
- Electroacupuncture alleviates ciliary muscle cell apoptosis in lens-induced myopic guinea pigs through inhibiting the mitochondrial signaling pathway
- De novel heterozygous copy number deletion on 7q31.31-7q31.32 involving TSPAN12 gene with familial exudative vitreoretinopathy in a Chinese family
