Peripapillary and macular vascular densities in healthy, ocular hypertensive, and different stages of glaucomatous eyes
2023-12-14CanerztrkSirelGrGngrmitEkioluAlmilaSarglSezenzMeriolak
Caner ztrk, Sirel Gr Gngr, mit Ekiolu, Almila Sargl Sezenz, Meri olak
1Department of Ophthalmology, Minister of Health Hitit University Erol Olçok Education and Research Hospital,Çorum 19030, Turkey
2Department of Ophthalmology, Başkent University, Faculty of Medicine, Ankara 06170, Turkey
3Department of Biostatistics, Başkent University, Faculty of Medicine, Ankara 06300, Turkey
Abstract
● KEYWORDS: glaucoma; optical coherence tomography angiography; vascular density; early diagnosis
INTRODUCTION
Glaucoma, which is an irreversible optic neuropathy with progressive loss of retinal ganglion cells (RGC), can be asymptomatic until the late stages[1].Although different pathways are responsible for the development of glaucoma,importance of vascular pathway has been emphasized in recent years[2-3].
Optical coherence tomography (OCT) is a noninvasive method in the detection of early glaucomatous structural damage[4].Retinal nerve fiber layer (RNFL) and ganglion cell analysis(GCA) have similar accurate diagnostic capacities[5-6].Optical coherence tomography angiography (OCTA) is a more recent method that provides retinal and choroidal structural information and evaluates blood flow in a fast and noninvasive way[7-9].
Prior studies have shown that peripapillary and macular vascular densities (VDs) are decreased in glaucomatous eyes[10-11].We have investigated vascular changes in healthy participants, and patients with ocular hypertension (OHT),preperimetric glaucoma (PPG), early-stage glaucoma (EG),moderate-stage glaucoma (MG), and advanced-stage glaucoma(AG).Subgroup analyses were performed to evaluate the role of OCTA in the early diagnosis of glaucoma.Correlations between OCTA and other structural and functional tests were investigated.The area under the receiver operating characteristic (AUC) analyses were done between the healthy participants and glaucoma groups to evaluate the diagnostic capacity of OCTA parameters.Also, AUC analyses were done among the glaucoma groups to show the discriminating power of the OCTA parameters.
SUBJECTS AND METHODS
Ethical ApprovalThis cross-sectional study was approved by the local ethics committee of Başkent University (Approval number: KA 19/252) and adhered to the tenets of the Declaration of Helsinki.Written consent was obtained from all participants that were examined between January 2018 and June 2019.Participants did not receive any stipend.
MethodsBest corrected visual acuity, gonioscopy, slit-lamp biomicroscopy, Goldmann applanation tonometry, visual field (VF) test, OCT and OCTA were performed.Exclusion criteria were previous diagnosis of optic nerve and retinal vascular pathologies, myopia, and hyperopia of 6 diopters or more, media opacities preventing quality of imaging,age younger than 18y or older than 90y, any ocular disease except glaucoma, and any previous ocular surgeries except uncomplicated cataract and glaucoma surgeries.
Visual fieldVF examinations were performed by Humphrey Field Analyzer II (Carl Zeiss Meditec, Dublin, CA, USA)using the 24-2 threshold test Swedish Interactive Threshold Algorithm standard strategy.Tests with false positive, false negative, and fixation loss rates of below 20% were included in the study.The mean deviation (MD) and pattern standard deviation parameters were recorded.
Optical coherence tomographyOCT images were obtained using Cirrus HD spectral domain OCT (Carl Zeiss Meditec,Dublin, CA, USA).Mean retinal nerve fiber layer thickness(RNFLT), superior, inferior, temporal, nasal RNFLT (S-RNFLT,I-RNFLT, T-RNFLT, N-RNFLT), and macular GCA (measured as ganglion cell layer+inner plexiform layer) were calculated.Images with a signal strength of <6/10 were excluded.
Optical coherence tomography angiographyThe OCTA imaging system Avanti RTVue-XR (Optovue, Fremont, CA,USA), which uses a split-spectrum amplitude-decorrelation angiography algorithm, was used to distinguish the movement of erythrocytes in the blood vessels.The contrast between the decorrelation of the blood flow and static tissue extracts flow signals for angiography[12].Retinal vascular structures were segmented automatically by AngioVue software.Images with under 6/10 signal strength, motion artifacts, fixation losses, and segmentation errors were excluded.
Peripapillary OCTA images were obtained with a 4.5×4.5 mm2diameter peripapillary scan centered on the optic disc.The device makes measurements using 2 and 4 mm diameter rings based on the disc center.The region inside the 2 mm area is considered the intrapapillary area, and the area between the two rings is considered as the peripapillary area.RNFL vascular network was calculated using VD of radial peripapillary capillary (RPC), which was automatically calculated from internal limiting membrane to outer border of the RNFL.Whole image peripapillary vascular density (WIPPVD) was calculated from the 4.5×4.5 mm2area.Intradisc vascular density (IDVD) measurement was obtained from the inner 2 mm diameter ring.Other evaluated parameters from the peripapillary area were peripapillary VD (PPVD), superior and inferior hemisphere peripapillary VD (SH-PPVD, IHPPVD), and superior, inferior, nasal and temporal peripapillary VDs (S-PPVD, I-PPVD, N-PPVD, T-PPVD).
The device uses three fovea-centered rings for macular OCTA scans.The innermost 1 mm diameter ring represents the fovea.The area between the inner 1 mm diameter ring and the middle 3 mm diameter ring indicates the parafoveal region, and the area between the 3 mm diameter ring in the middle and the outermost 6 mm diameter ring indicates the perifoveal region.Since the ganglion cells are mostly located in the parafoveal area and the superficial plexus is responsible for blood flow supply in these cells, VDs of the superficial plexus in the parafoveal area were examined.To evaluate the superficial capillary plexus, an area between the upper limit of internal limiting membrane and the lower limit of 10 μm below the inner plexiform layer is automatically created by the OCTA device.The whole image macular VD (WI-MVD) was calculated from the 6×6 mm2area.Other evaluated parameters were parafoveal VD (PFVD), superior and inferior hemisphere parafoveal VD (SH-PFVD, IH-PFVD), superior, inferior,nasal, and temporal parafoveal VDs (S-PFVD, I-PFVD,N-PFVD, T-PFVD).
SubjectsAll subjects were divided into six groups.Healthy participants were required to have normal VF tests (pattern standard deviation within the 95% confidence limits and glaucoma hemifield test result within normal limits),intraocular pressure (IOP) <21 mm Hg, intact neuroretinal rims, normal GCA test results, and normal OCT test results,defined as an RNFLT within the 95% confidence interval (CI).OHT patients were defined as having IOP>21 mm Hg with normal VF and OCT test results.PPG patients were defined as having IOP>21 mm Hg, decreased RNFLT on OCT imaging to outside the 95%CI of the normal distribution without any VF defect.Other glaucomatous patients were divided into groups according to VF test results.In this classification, EG was defined as MD>-6 dB, MG as MD between -6 to -12 dB,and AG as MD<-12 dB.Only one eye from each subject was included in the study.If both eyes were eligible, one eye was chosen randomly.
Statistical AnalysisIBM Statistical Package for the Social Sciences version 25.0 (SPSS ver.25.0) was used for statistical analysis.The variables were investigated using Kolmogorov-Simirinov method to determine wheter or not they are normally distrubuted.Continuous variables were presented as means±standard deviation (SD).Kruskal Wallis variance analysis was used for the comparison of the clinical and demographic characteristics of the participants.For the comparison of RNFLT and VD among the groups, analysis of covariance (ANCOVA) was used to control for possible age and IOP related changes.The Mann-WhitneyUtest was performed to test the significance of pairwise differences.Spearman correlation test was used to find the correlation between measurements and AUC were calculated to show the diagnostic accuracy and discriminating power of parameters.P<0.05 was considered statistically significant.
RESULTS
There were 29 eyes in healthy controls, 44 eyes in OHT, 32 eyes in PPG, 35 eyes in EG, 36 eyes in MG, and 35 eyes in AG groups.Table 1 summarizes the clinical and demographic features of the participants.Significant differences were detected in the mean age and IOP between the groups (P=0.001 andP<0.001, respectively).The only significant difference in the mean age was seen between OHT and AG groups(P=0.004), while no significant difference was seen among other groups (P>0.05).Subgroup analysis was done for IOP values, and the significant difference was attributed to the higher IOP values of the OHT group (P=0.03).There was no significant difference between the groups in gender, systolic and diastolic blood pressure, pulse rate and frequency of diabetes mellitus and hypertension (allP>0.05).
The age and IOP adjusted RNFLT, GCA, MD, peripapillary and macular VD measurements are shown in Tables 2 and 3.Significant differences were found in all parameters among the groups (P<0.001).As expected, RNFLT was found to be higher in healthy participants and OHT groups compared to other groups and RNFLT and GCA decreased with the severity of the disease.Both peripapillary and macular VD parameters decreased with the severity of the glaucoma.
Healthy participants, PPG and EG groups were evaluated separately to determine whether there was a change in RNFLT, peripapillary and macular VDs in the early stages of the disease (Table 4).Mean and sectorial RNFLT values were significantly lower in PPG and EG groups compared to the healthy participants group (P<0.05) and no significant difference was found between PPG and EG groups (P>0.05).Moreover, significant differences were found between healthy participants and PPG groups for all peripapillary VD measurements except IDVD.When healthy participants and EG groups were analyzed for the peripapillary VDs, significant differences were found in all parameters, except IDVD.Macular VD analysis indicated significant differences between the healthy participants and PPG groups only for WI-MVD.When healthy participants and EG groups were compared, all macular VD parameters were significantly lower in the EG group (P<0.05).There was no significant difference in RNFLT between the PPG and EG groups, however WI-PPVD, PPVD,SH-PPVD, IH-PPVD, N-PPVD, and S-PPVD values, and all macular VD parameters, except N-PFVD, were found to be significantly lower in the EG group than in the PPG group(P<0.05).Correlations between peripapillary VDs, macular VDs, and mean RNFLT, mean GCA, and MD are shown in Table 5.The correlations between mean GCA and peripapillary VDs (WIPPVD and PPVD) were found to be significant in all groups.The evaluation of correlations between the mean RNFLT and peripapillary VDs (WI-PPVD and PPVD) showed that WI-PPVD had significant correlations in all groups, except the healthy participants and OHT groups and PPVD had significant correlations in all groups, except the AG group.WIMVD was correlated with mean GCA in all groups, except healthy participants and with mean RNFLT in all groups,except healthy participants and AG groups.Although PFVD was correlated with mean GCA and mean RNFLT in some groups, these correlations were not as strong as other VDs correlations.Correlations between MD and peripapillary VDs(WI-PPVD and PPVD) were found to be significant in OHT,MG, and AG groups.WI-MVD was correlated with MD in OHT and MG groups and PFVD was correlated with MD only in the OHT group.

Table 2 RNFLT, GCA and MD measurements of the groups mean±SD
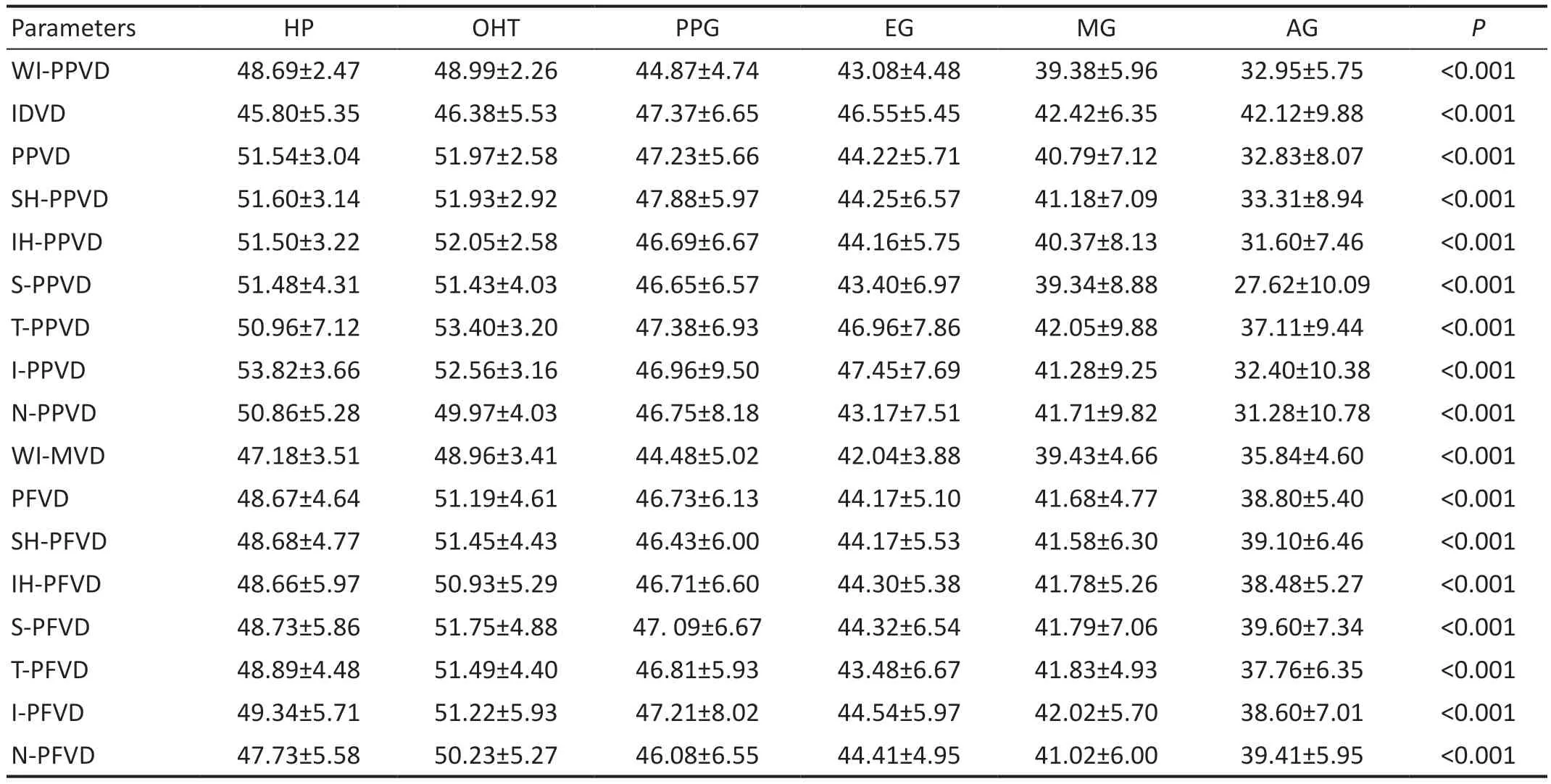
Table 3 Peripapillary and macular vascular density measurements of the groups mean±SD
The AUC analyzes were done to evaluate diagnostic capacities of the OCT and OCTA parameters to distinguish the other groups from healthy participants (Figure 1, Table 6).WI-PPVD had the highest diagnostic capacity in EG, MG and AG groups(AUC=0.865, 0.929, 0.986, respectively).The diagnostic capacities of WI-PPVD and PPVD were similar to RNFLT and GCA.Also AUC analyses were done to discriminate the respective next stage of the disease (OHTvsPPG, PPGvsEG,EGvsMG, MGvsAG).OCTA parameters can significantly discriminate PPG eyes from OHT eyes and AG eyes from MG eyes.
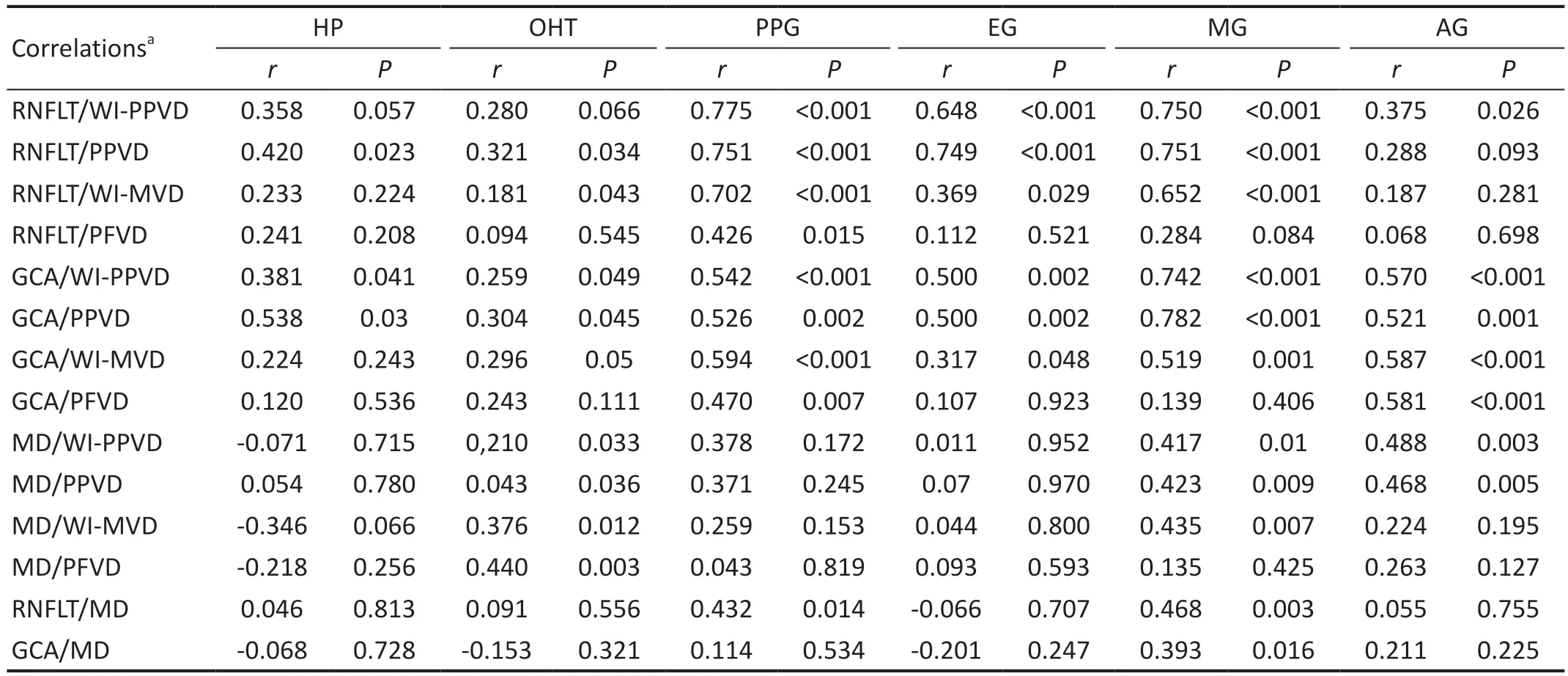
Table 5 Correlations between peripapillary VDs, macular VDs and RNFLT and GCA and visual field MD
DISCUSSION
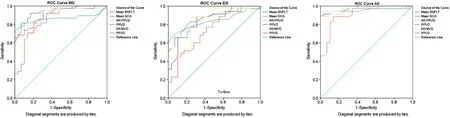
Figure 1 Receiver operator curve analyses for differentiating EG, MG, and AG eyes from healthy control eyes RNFLT: Retinal nerve fiber layer thickness; GCA: Ganglion cell analysis; WI: Whole image; PPVD: Peripapillary vessel density; MVD: Macular vessel density; PFVD: Parafoveal vessel density; EG: Early-stage glaucoma; MG: Moderate-stage glaucoma; AG: Advanced-stage glaucoma.
In the present study, we investigated the peripapillary and macular VDs of patients with different stages of glaucoma;correlation of these VDs with OCT and VF test results; and diagnostic abilities of the VD, RNFLT, and GCA parameters.In this study, the glaucomatous groups were divided according to the VF test results as EG, MG and AG.Healthy participants,OHT, and PPG were also the other groups of the study.Significant differences were detected in age and IOP between the groups.In pairwise comparisons, the only significant difference in the mean age was found between AG and OHT groups.As glaucoma progresses over the years, advanced disease is expected to be more common in elderly patients.Additonally, in the pairwise comparisons OHT group has higher IOP values than other groups.OHT patients do not have any structural or functional glaucomatous defects despite the fact that they have high IOP values.Therefore, IOP values of OHT patients are usually monitored without treatment and even if antiglaucomatous treatment is applied, it is done without the intent of lowering the IOP as low as in glaucoma patients.
Previous studies have shown that OCT can detect glaucomatous defects[4,13-14].Consistent with previous studies, we found that the RNFL and GCA thickness decreased with the severity of disease.
Decreased peripapillary VD in glaucoma patients was reported in previous studies[15-17].Geymanet al[17]reported that VD decreased, as glaucoma severity increased.Yarmohammadiet al[18]reported that each 1% decrease in PPVD was associated with 0.64 dB loss in MD and that each 1% decrease in WI-PPVD was associated with 0.66 dB loss in MD.Previous studies have shown that RGCs are mostly located in the macular area[19-20].So macular VDs have been examined to evaluate the role of the macular vascular damages in glaucomatous eyes,however, contradictory results have been reported.Bojikianet al[21]showed that macular VDs were lower in glaucomatous eyes than in healthy eyes and vascular damage was correlated with the disease severity.Trioloet al[10]analyzed healthy participants, patients with suspected glaucoma, and patients diagnosed with glaucoma and reported a significant decrease in peripapillary VD parameters in glaucomatous eyes compared to other groups, but no significant difference in macular VD across groups.In our study, peripapillary and macular VD parameters were lower in glaucomatous groups and all parameters of peripapillary and macular VDs demonstrated a stepwise decrease through worsening glaucoma stage.
In subgroup analyses, RNFLT, peripapillary and macular VDs of healthy participants, PPG and EG groups were evaluated to determine whether there was a change in the early stages of glaucoma.WI-MVD, mean and sectorial RNFLT except T-RNFLT, all peripapillary VD parameters except IDVD, were significantly lower in the PPG group compared to the healthy participants.When the EG group and healthy participants were compared, all peripapillary VD parameters except IDVD, mean and sectorial RNFLT and all macular VD parameters were lower in the EG group compared to the healthy participants.Both peripapillary and macular VDs decrease in the early stages of the disease as in RNFLT.Transition from PPG to EG is important because functional loss begins in the EG group with the VF defect.Therefore, we compared the PPG and EG groups separately.There was no significant difference in RNFLT values between PPG and EG groups but all macular VDs except the N-PFVD and all peripapillary VDs except IDVD, T-PPVD and I-PPVD were found to be lower in the EG group compared to the PPG group.
Chunget al[22]investigated correlations between VDs and RNFLT, GCA, and MD in glaucomatous eyes.Peripapillary VD had higher correlation (r=0.772, 0.701, and 0.631 respectively,P<0.001) than parafoveal VD (r=0.443, 0.474,and 0.453 respectively,P<0.001).Trioloet al[10]reported that although there was a correlation between RNFLT and peripapillary VD, no significant correlation was found between GCA, mean RNFLT, and macular VD (allP>0.05) in glaucoma suspects and glaucoma patients.In their glaucoma group, a highly significant correlation was seen between mean peripapillary VD and MD (r=0.675,P<0.001), but no significant correlation was found between macular VD and MD.Shinet al[23]investigated the association between progressive PPVD loss and VF progression in glaucoma patients and found that the rate of VD loss was significantly associated with VF progression both in early and moderate to advanced glaucoma.In our study, PPVDs were significantly correlated with MD in OHT, MG and AG groups, but no significant correlations were found in PPG and EG groups.In our study, IOP values of the OHT group were higher than EG and PPG groups.Chiaraet al[24]reported a significant decrease in PPVD parameters in OHT eyes compared to normal eyes.They suggested that the optic nerve nutrition would be impaired due to high IOP and therefore VD would decrease.High IOP may affect the VF indices similarly by disrupting the optic nerve nutrition.This situation can be clarified in future studies with OHT patients whose IOP decreased with treatment and who were followed without IOP reduction.The reason why no significant correlation between the PPVD and MD was found in the PPG and EG group, may be the earlier onset of vascular and structural damage than the VF defect.In our study, peripapillary and macular VDs were significantly correlated with mean RNFLT and mean GCA in most disease groups.RPCs nourish the RNFL and RGC axons.WI-PPVD and PPVD are RPC network-related parameters.In our study,peripapillary VDs were correlated with mean RNFLT and mean GCA more than macular VDs.These stronger correlations of WI-PPVD and PPVD can be attributed to their associations with RPC.Correlation between VD parameters and RNFLT decreases in the AG group and this result was attributed to the floor effect of RNFLT.While there is no more RNFL loss due to the floor effect in the AG group, VD decreases as the disease progresses.Additionally, there were no significant correlations between MD and RNFLT and GCA indices in the AG group,but significant correlations were found between MD and VD values.Therefore, VD parameters may be used in the followup of advanced disease.
Diagnostic abilities of the RNFLT, GCA, and VD parameters have been compared in previous studies.Raoet al[25]reported that the mean RNFLT (AUC=0.95) had the best diagnostic efficacy, followed by neuroretinal rim area (AUC=0.94),and mean GCA and WI-PPVD (AUC=0.93).The AUC of PPVD, IDVD, WI-MVD, and PFVD were 0.85, 0.77, 0.73,and 0.70, respectively, which were significantly lower than RNFLT, GCA, and WI-PPVD parameters.Yarmohammadiet al[26]reported that AUC was highest for WI-PPVD (0.94),followed by RNFLT (0.92) and PPVD (0.83).Our results are in good agreement with these previous studies that showed that WI-PPVD differentiates glaucomatous and healthy eyes as well as RNFLT and GCA.In our study, WI-PPVD had the highest diagnostic accuracy for discriminating between healthy controls and EG, MG, and AG groups.Previous studies have shown that diagnostic abilities of the VDs increased as the glaucoma severity increased from an early stage to advanced stage disease[22,27].Consistent with previous reports, the highest diagnostic abilities of the VD, RNFLT, and GCA were seen in the AG group as expected.Moreover, in the AG group,diagnostic capacity of WI-PPVD (0.986) and WI-MVD (0.967)were higher than mean RNFLT (0.958) and mean GCA (0.956),probably due to the floor effect.Therefore, in AG group OCTA may be more useful than OCT in follow-up.In our study, OCTA had a similar diagnostic ability to OCT in early diagnosis of the glaucoma.When differentiating EG eyes from healthy control eyes, WI-PPVD (0.865) had higher diagnostic ability than the mean RNFLT (0.860) and WI-MVD (0.839)had higher diagnostic ability than mean GCA (0.828).These results shows the benefit of OCTA in the diagnosis of the early stages of glaucoma.Also, WI-PPVD (0.860) had higher discriminating power than the mean RNFLT (0.740) and WIMVD (0.790) had higher discriminating power than mean GCA (0.721) in discriminating AG eyes from MG eyes.When VF progression is suspected or VF test is unreliable in MG and AG patients, evaluation of OCTA data may be useful to show the glaucoma progression.Generally, macular VDs had lower diagnostic abilities compared to the peripapillary VDs.
Our study has several limitations.Patients with diseases that may affect peripapillary and macular VD, such as diabetic retinopathy, hypertensive retinopathy, poorly controlled diabetes and arterial hypertension, and age-related macular degeneration were excluded.Since the exclusion of patients with diabetes mellitus and hypertension without retinopathy would have reduced the number of patients too much, these patients were not excluded.Additionally, possible effects of different antiglaucomatous medications on VD were ignored.
In conclusion, this study showed that peripapillary and macular VDs decrease with the severity of glaucoma.VD parameters were found to be lower in EG and PPG groups than in healthy participants.Moreover, while there was no significant difference in structural tests between PPG and EG groups,VD parameters were lower in the EG group than in the PPG group.High correlations were also determined between OCT parameters and PPVDs.Therefore, we showed that OCTA can provide an early diagnosis of glaucoma and this is the strongest part of our study.Additionally statistically significant correlations were found between MD and VD values.Since OCT is not useful in the patient follow-up of the AG group due to the floor effect, OCTA may be used instead.WI-PPVD and WI-MVD had similar diagnostic accuracy as OCT parameters.Moreover, WI-PPVD had the highest diagnostic accuracy for discriminating between healthy participants and EG, MG, and AG groups.Diagnosis of glaucoma can be challenging due to the tilted optic disc and peripapillary atrophy in highly myopic eyes[28].OCTA can be used as a supportive test in cases when structural and functional tests are not conclusive.
ACKNOWLEDGEMENTS
The authors would like to thank Prof.Dr.Ahmet Akman for his advices and encouragements.
Authors’ contributions:Medical practices: Öztürk C,Güngӧr SG, Ekşioğlu Ü; Design: Öztürk C, Güngӧr SG; Data collection or processing: Öztürk C, Sezenӧz AS; Analysis or interpretation: Öztürk C, Güngӧr SG, Çolak M; Literature search: Öztürk C; Writing: Öztürk C.
Conflicts of Interest: Öztürk C,None;Güngör SG,None;Ekşioğlu Ü,None;Sezenöz AS,None;Çolak M,None.
杂志排行
International Journal of Ophthalmology的其它文章
- Dynamic tear meniscus parameters in complete blinking:insights into dry eye assessment
- Effects of diquafosol sodium in povidone iodine-induced dry eye model
- Morroniside ameliorates lipopolysaccharide-induced inflammatory damage in iris pigment epithelial cells through inhibition of TLR4/JAK2/STAT3 pathway
- Role of reactive oxygen species in epithelial-mesenchymal transition and apoptosis of human lens epithelial cells
- Electroacupuncture alleviates ciliary muscle cell apoptosis in lens-induced myopic guinea pigs through inhibiting the mitochondrial signaling pathway
- De novel heterozygous copy number deletion on 7q31.31-7q31.32 involving TSPAN12 gene with familial exudative vitreoretinopathy in a Chinese family
