Clinical significance of episcleral venous fluid wave in gonioscopy-assisted transluminal trabeculotomy
2023-12-14LiuZhiZengYuHeXiaoQinWangYiPingXianHanYingFanLinJingJingShuQinLiNingLiWang
Liu-Zhi Zeng, Yu He, Xiao-Qin Wang, Yi-Ping Xian, Han-Ying Fan, Lin Jing, Jing Shu,Qin Li, Ning-Li Wang
1Department of Ophthalmology, Chengdu First People’s Hospital/Chengdu Integrated TCM and Western Medicine Hospital, Chengdu 610041, Sichuan Province, China
2Beijing Tongren Eye Center, Beijing Institute of Ophthalmology, Beijing Tongren Hospital, Capital Medical University, Beijing 100730, China
Abstract
● KEYWORDS: episcleral venous fluid wave; intraocular pressure; transluminal trabeculotomy, gonioscopy-assisted;anti-glaucoma medication; postoperative complications
INTRODUCTION
In recent years, minimally invasive glaucoma surgery(MIGS) has attracted the attention to glaucoma doctors and glaucoma patients due to its safer surgical profile and fewer complications[1].MIGS with Schlemm’s canal is characterized by bypassing or removing the diseased trabecular meshwork,allowing aqueous humor to flow directly through Schlemm’s canal into the collector tube and into the scleral circulation system.This procedure provides a physiological pathway for a smoother outflow[2-3].
Gonioscopy-assisted transluminal trabeculotomy (GATT) is one of MIGS surgeries[4].The theory of GATT is to cut the trabecular tissue and the inner wall of Schlemm’s canal in a 360-degree circular way with suture or catheter assisted by gonioscope, so that the aqueous humor can directly connect with the Schlemm’s canal, so as to reduce the resistance of aqueous humor outflow and achieve the purpose of lowering intraocular pressure (IOP)[5-6].It has been reported that the success rate after only GATT is 70%-80%[7-8].What is the mark of success in surgery? Fellmanet al[9]described a new perioperative marker for successful trabecular ablation, which they named as episcleral venous fluid wave (EVFW), and found that postoperative IOP was significantly negatively correlated with the degree of EVFW.Aktaset al[10]observed EVFW during GATT operation in 34 eyes of 28 patients with advanced primary open angle glaucoma (POAG).They found that the degree of EVFW was negatively correlated with postoperative IOP, suggesting that EVFW may be a valuable prognostic indicator to judge the success of GATT surgery.In this study, 30 patients (45 eyes) with open angle glaucoma(OAG) were examined for the location and extent of EVFW during GATT, and the effect of EVFW on IOP and success rate after operation was analyzed and discussed.
SUBJECTS AND MATHODS
Ethical ApprovalThe study was conducted in accordance with the Declaration of Helsinki and approved by the Medical Ethics Committee of Chengdu First People’s Hospital(No.2022YNYJ22).Oral informed consent was obtained from all patients.
Study SubjectsTotally 45 eyes of 30 patients with OAG who underwent GATT surgery were included in this retrospective study in the Department of Ophthalmology, Chengdu First People’s Hospital from August 2019 to August 2020.All of the patients were OAG comprising POAG (n=20), juvenile congenital glaucoma (n=6), posner-schlossman syndrome(n=2), and angle recession glaucoma (n=2).Among the 30 patients (45 eyes), there were 20 males (30 eyes) and 10 females (15 eyes) who aged 13-80 years old, with an average age of 66.80±14.20y.All patients were performed by the same surgeon.There were 10 patients (15 eyes) with middle stage glaucoma and 20 patients (30 eyes) with advanced stage glaucoma.Glaucoma was staged according to the mean defect(MD) of visual field.Early stage: MD≤-6 dB, middle stage:-12 dB≤MD<-6 dB, and advanced stage: MD<-12 dB[11].The inclusion criteria were as follows: the patient was diagnosed with OAG and no other anti-glaucoma surgery was performed.Patients with a history of trabeculectomy, drainage valve implantation, operation of pterygium, conjunctival hemorrhage and edema that affected the observation of EVFW were excluded, and patients without a 360-degree trabeculectomy during surgery were excluded.
Surgical ProceduresEach patient underwent GATT surgery and the procedure was as follows.Two auxiliary incisions were made in the subtemporal and superior nasal transparent limbus with a 15-degree blade after three times of topical anesthesia.A 2.2 mm temporal clear cornea incision was made after topical anesthesia.In addition, a 2.0-mm limbal incision was created at the clear superior temporal cornea.Lidocaine injection (1%,0.1 mL) was injected into anterior chamber for intraocular anesthesia through temporal site incision.Diluted carbachol 1:1 was injected into anterior chamber to contract pupil and viscoelastic material was injected into anterior chamber to increase the IOP about 30 mm Hg.Adjust the microscope angle and the position of the patient’s head.
An iTrack™ 250-μm microcatheter was pre-positioned into the anterior chamber from the assisted incision, and the Zeng’s trabeculotomy knife was used at o’clock 7:30 (left eye) or 4:30 (right eye) with the aid of a gonioscope.The trabecular tissue and the inner wall of Schlemn’s canal were incised about 2 mm, viscoelastic material was injected into the incision to prevent bleeding, the tip of the microcatheter was clamped with the inner eye, and the Schlemm’s canal was inserted from the broken end of the trabecular incision and advanced counterclockwise or clockwise.Viscoelastic material was injected one time for every one clock position forward of the optical fiber.After traveling through 360 degrees, the head end of the microcatheter was seen passing through the other end of the incision opening of Schlemm’s canal.At the same time, pulled the other end of the microcatheter to make a 360-degree incision of the trabecular tissue and the inner wall of Schlemm’s canal (Figure 1A, 1B).If there was blood return from the anterior chamber angle, the position and range of blood return should be recorded in detail, and then the blood and viscoelastic agent should be washed with balanced salt solation (BSS), and the four quadrants of the chamber angle should be pressurized with BSS respectively.The changes of scleral veins on the surface of the corneal limbal should be examined during the pressor irrigation process.If the color of the limbal conjunctiva changed from red to pale (Figure 1C,1D) or BSS flow was observed in the scleral veins (Figure 1E,1F), the EVFW was defined to be positive, and the rientation and extent of EVFW were recorded in detail.If no EVFW was found during pressure irrigation, repeated irrigation was performed in the quadrant for 3 to 4 times until EVFW was seen.The limbal incision was closed to form the anterior chamber, and the operation was completed.
After surgery, prednisolone acetate eye drops and levofloxacin eye drops were given 4 times a day for 2wk.Diclofenac sodium eye drops was given 4 times a day for 2wk and 3 times a day for 3mo.One week after surgery, 2% picotropicine eye drops were given 3 times for 3mo.
Follow-up and Observation IndexesIOP, the number of anti-glaucoma medication and complications were observed at 1d, 1wk, 1, 3, 6 and 12mo postoperation.The phenomenon of BSS flow in superficial scleral veins or the keroscleral margin vessels turning from red to white during the operation is called EVFW positive, and no BSS flow or color change is considered as negative.EVFW is divided into 5 grades:negative in four quadrants as grade 0, positive in one quadrant as grade 1, positive in two quadrants as grade 2, positive in three quadrants as grade 3, and positive in four quadrants as grade 4.A complete success for surgery is defined as a postoperative IOP<18 mm Hg without any anti-glaucoma medication.IOP<18 mm Hg with less than two anti-glaucoma medications is defined as qualified success, while the control of IOP requiring three anti-glaucoma medications is considered as unsuccess.

Figure 1 GATT surgery procedures The microcatheter was introduced into Schlemm’s canal (A), and the trabecular tissue and the inner wall of Schlemm’s canal were dissected 360 degrees with the microcatheter (B).The color of conjunctival corneal limbus changed from red (C) to pale (D) when the anterior chamber angle was pressurized with BBS injection.BSS fluid flow in the scleral vein during injection with anterior chamber angle pressure, and the color of blood vessels changed from red (E) to pale (F).GATT: Gonioscopyassisted transluminal trabeculotomy; BSS: Balanced salt solation.
Statistical AnalysisSPSS 20.0 software was used to analyze the data.Pairedttest was used to compare IOP before and the last follow-up after surgery.Wilcoxon rank sum test was used to compare the number of anti-glaucoma medications used before and after the operation.P<0.05 was considered statistically significant.
RESULTS
Intraocular PressurePreoperative IOP was 26-48 mm Hg with the average of 35.38±7.16 mm Hg.The average IOP at 3,6, and 12mo after surgery were significantly decreased (P<0.01;Figure 2).There was no difference in IOP between middle stage and advanced stage glaucoma.
Episcleral Venous Fluid WaveThe grade of EVFW in all patients were 2-4, of which grade 2 accounted for 33.33%,grade 3 accounted for 40%, and grade 4 accounted for 26.67%(Table 1).The location of EVFW were inferior (36%), nasal(28%), superior (20%), and temporal (16%).The distribution of EVFW was consistent with that of blood return from the anterior chamber angle.There was no significant difference in EVFW grade between patients in the middle and late stages(P>0.05).
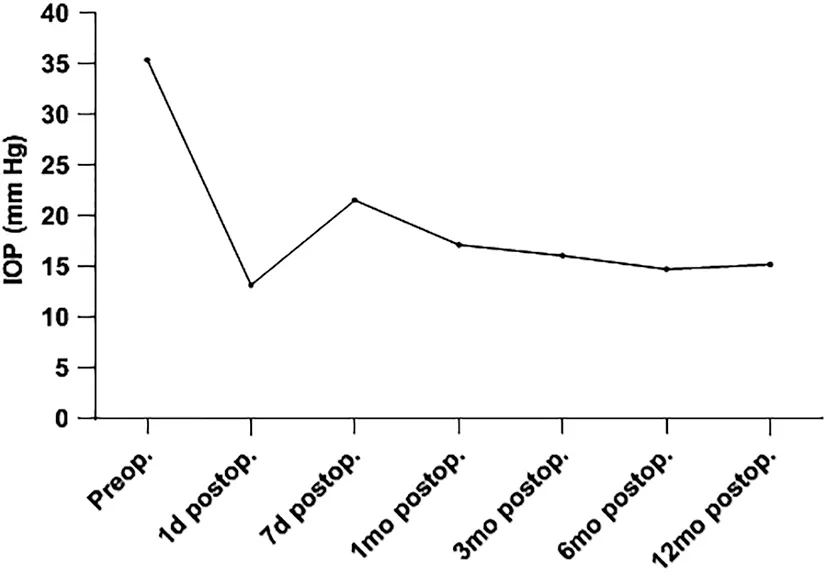
Figure 2 Changes in IOP before and after surgery Preop.: Preoperation;Postop.: Postoperation; IOP: Intraocular pressure.
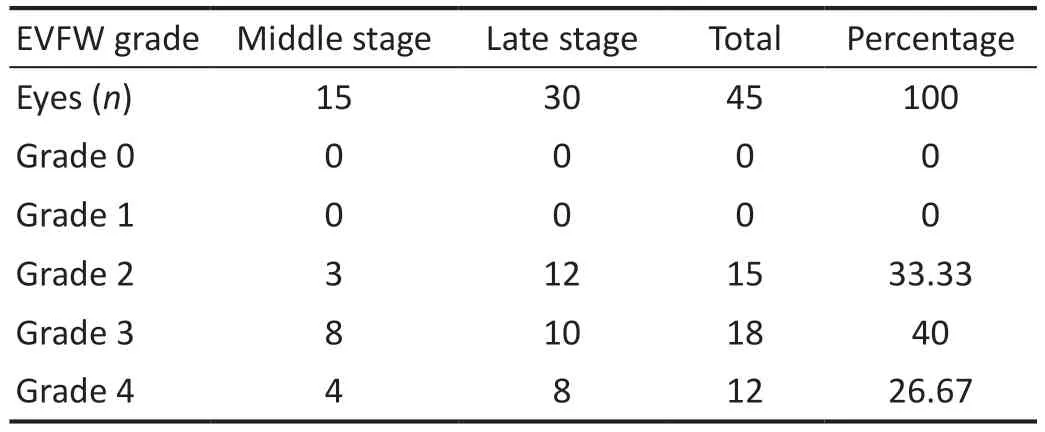
Table 1 The grade of EVFW in all patients

Table 2 EVFW grade with difference success rates after GATT
Success RateThe total success rate was 93.33%.Complete success rate was 66.67%, qualified success rate was 26.67%and 6.66% of unsuccessful cases required reoperation.The EVFW grade of complete success patients was 3.4±0.6 (3-4),and that of qualified success patients was 2.6±1.0 (2-4) and there was a statistical difference between them (P<0.05; Table 2).Number of Anti-glaucoma MedicationThe number of medication was 2.8±1.2 (2-4) before surgery and 0.6±1.3(0-3) 12mo after surgery.There was a significant statistical difference in the number of medication before and after surgery(P<0.01; Table 3).
ComplicationsIntraoperative fluid misdirection syndrome and descemet membrane detachment were 2 eyes (4.44%),respectively.Postoperative hyphema was 16 eyes (35.56%) and IOP-spike occurred in 18 eyes (40%), and there were no serious complications such as choroidal detachment and endophthalmitis.

Table 3 Number of anti-glaucoma medications
DISCUSSION
GATT is an MIGS surgery, firstly proposed by Groveret al[12]in 2014.This surgery is performed by 5-0 prolene suture or the iTrack™ 250-μm microcatheter to make a 360° incision of the trabecular tissue and the inner wall of Schlemm’s canal for primary and secondary OAG[13-14].It has been reported that the success rate of GATT alone can reach 60%-70%, while it can reach more than 90% combined with medication or cataract surgery[15].How to predict the success of GATT? Some people think that it is a sign of success when there is a uniform blood return from anterior chamber angle.Other researchers found that the intraoperative examination of EVFW in GATT could be used to predict the success of the operation[9,16].They divided the EVFW into 0-6h and the EVFW range is calculated by clock time.It was found that the range of EVFW was significantly correlated with the number of anti-glaucoma medications need and the degree of IOP reduction.The larger the range of EVFW, the greater the range of IOP reduction and the smaller the number of anti-glaucoma medications required.In present study, we performed GATT on 45 eyes of 30 patients with OAG.During the operation, EVFW was examined by pressurizing the anterior chamber angle with BSS.The purpose was to estimate whether the aqueous humor drainage channel was clear or not by using BSS to enter the superficial scleral vein of the limbal from the incised trabecular tissue and the fluid collecting tube.At the same time, it was hoped that the blocked or closed aqueous humor channel can be opened up again by pressure flushing.Our method of recording the range of EVFW was different from that of the previous study in terms of hours[10].We classified the range of EVFW into 5 grades which was simpler and more accurate to record EVFW by quadrant than by hour.At present study, EVFW was positive in all cases, ranging from 2 to 4, including 15 eyes of 10 cases(33.33%) in grade 2, 18 eyes of 12 cases (40.00%) in grade 3,and 12 eyes of 8 cases (26.67%) in grade 4.However, grade 0 and 1 were not observed in this study, indicating that the aqueous humor pathway was unblocked at least 2 quadrants in all cases.Our study showed that the distribution of EVFW may have certain rules, with the proportion of EVFW in inferior(36%), nasal (28%), superior (20%), and temporal (16%),respectively.The proportion of EVFW in the inferior and nasal quadrant was larger than that in the superior and the temporal quadrant, which indicated that the inferior and nasal quadrant may be the dominant pathways for aqueous humor outflow.
In current study, 30 patients (45 eyes) with OAG were followed up 12mo after operation, and the total success rate was 93.33%.Among them, 30 eyes of 20 patients (66.67%)were complete success without anti-glaucoma medication, and 13 eyes of 8 patients (26.67%) were qualified success with less than two kinds of medication.The operation failed in 2 eyes(6.66%) requiring 3 kinds of medication for lowering IOP.Compared with the success rate reported in previous studies,the success rate of this study was higher[17-18].This study found that the EVFW grade of complete success patients was 3.4±0.6,and that of qualified success patients was 2.6±1.0.The higher the EVFW grade, the lower the postoperative IOP, indicating that the grade of EVFW was negatively correlated with IOP.
Among all the patients in our study, 10 patients (15 eyes) in the middle stage accounted for 33.33%, and 20 patients (30 eyes) in the advanced stage accounted for 66.67%.The higher the EVFW grade, the greater the IOP reduction and the better the effect, indicating that both groups of patients obtained higher grade EVFW through pressure irrigation of aqueous humor pathway with BSS during surgery.In fact, we made 3 to 4 clear limbus incisions during surgery.The external wall of the open Schlemm’s canal and the connected aqueous humor pathway can be irrigated in all aspects.During the operation,we investigated that at the beginning of the observation of EVFW, some EVFW could not be observed.But after several times of pressurized irrigation of the anterior chamber angle,the positive EVFW could be observed and the range gradually increased, even reaching grade 4.It indicated that the anterior chamber angle was irrigated by pressure during GATT.It can make the narrow and occluded aqueous humor channel open again, reduce the resistance of aqueous humor, and achieve a better effect of lowering IOP.There was no correlation between the EVFW grade and the severity of glaucoma in our study.The extent of EVFW have achieved at least grade 2 in all patients with advanced glaucoma.Theoretically, the EVFW of grade 2, equivalent to 180 degrees of aqueous humor access unobstructed, can meet the requirements of aqueous humor circulation, so that IOP can be controlled after surgery.
In this study, IOP higher than 25 mm Hg in the early postoperative period of GATT was referred as IOP-spike,while previous authors referred IOP higher than 30 mm Hg as IOP-spike[18-19].In all cases, IOP decreased on the first day after GATT surgery, and IOP was around 15 mm Hg in most patients.So we believe that the IOP of 25 mm Hg is a more appropriate value.IOP-spike occurred in 18 eyes of the 45 eyes at 5-10d after operation in this study.The mechanism of postoperative IOP-spike has not yet been clarified[20-21].It may be related to postoperative aqueous humor pathway remodeling, and further studies are needed to clarify the mechanism of IOP-spike.
Intraoperative fluid misdirection syndrome was 2 eyes during the pressure irrigation of the anterior chamber angle, which may be related to the aqueous humor misdirection.This situation was not special treated during the operation, and mannitol was given after the operation[22].The anterior chamber recovered on the second day after the operation, and the IOP was normal.At present, the mechanism of aqueous humor misdirection is not clear, and there is no literature report on the occurrence of aqueous humor misdirection during GATT.This study is the first report on the intraoperative aqueous humor misdirection syndrome in GATT.However, fluid misdirection syndrome has been reported in other ocular surgeries[23-24].The cause and mechanism of fluid misdirection syndrome may be related to intraoperative high IOP and loose fiber structure of the suspensory ligament of the lens[25].Excessive perfusion pressure of the anterior chamber may cause relaxation or even tear of the suspensory ligament, or abnormal development of the suspensory ligament of the lens.This causes reflux of perfusate into the vitreous resulting in shallow anterior chamber and elevated IOP.Intravenous mannitol infusion,vitreous extraction, anterior vitrectomy and other measures can be taken to relieve acute aqueous humor misdirection[26].It is suggested that during the operation, the anterior chamber angle should be washed by pressure slowly, with moderate force, not too hard, and try to avoid the flow of aqueous humor into the vitreous cavity.
Descemet membrane detachment was occurred in 2 eyes of 2 cases during the operation, and the disinfection air bubble was injected into the anterior chamber after the operation, and all of them recovered in 1-3d.This may be related to the excessive expansion of the inner wall of Schlemm’s canal by the injection of viscoelastic agent during the operation, or the excessive force and fast speed during the pulling of the microcatheter[27].It is suggested that the dose of viscoelastic material injected into the Schlemm’s canal should be appropriate during GATT.Generally, it is advisable to rotate the syringe 1-2 times when we pull the microcatheter one clock.At the same time, after the microcatheter is fully penetrated 360 degrees, the action of pulling the microcatheter should be gentle, not too fast, and avoid excessive force, so as to reduce the risk of shedding the descemet membrane of cornea.
In 45 eyes of 30 patients, there were 11 cases (16 eyes)with varying degrees of hyphema, accounting for 36.67%.Among them, 2 cases of hyphema were difficult to absorb by themselves, which was relieved after anterior chamber irrigation.It has been reported that the incidence of hyphema after GATT is 9.3%-68%, generally appearing on the first day after surgery, absorbing about 1wk, and rarely requiring anterior chamber irrigation[28-29].The incidence of hyphema is correlated with the type of glaucoma surgery, surgical skills and the presence of viscoelastic agent in anterior chamber[30].
In conclusion, during GATT surgery, pressurized irrigation of anterior chamber to check EVFW can reduce the outflow resistance of aqueous humor and increase the effect of postoperative IOP.The range of EVFW is negatively correlated with postoperative IOP.The larger the range of EVFW, the lower the postoperative IOP.Therefore, EVFW may be a valuable prognostic indicator for the success of GATT surgery.However, due to the small number of cases in this study,further studies are required to clarify the clinical value of EVFW examination and the exact mechanism and influencing factors of successful and failed GATT surgery.
ACKNOWLEDGEMENTS
Authors’ contributions:Zeng LZ and Wang NL conceived and designed the study.He Y, Xian YP, Fan HY, Jing L, Shu J and Li Q collected patient data and analyzed the data.Zeng LZ, Wang XQ and Shu J drafted and revised the manuscript.Wang NL took responsibility for the integrity of the work.All authors read and approved the manuscript.
Foundation:Supported by Sichuan Science and Technology Program (No.2021YFS0214).
Conflicts of Interest: Zeng LZ,None;He Y,None;Wang XQ,None;Xian YP,None;Fan HY,None;Jing L,None;Shu J,None;Li Q,None;Wang NL,None.
杂志排行
International Journal of Ophthalmology的其它文章
- Dynamic tear meniscus parameters in complete blinking:insights into dry eye assessment
- Effects of diquafosol sodium in povidone iodine-induced dry eye model
- Morroniside ameliorates lipopolysaccharide-induced inflammatory damage in iris pigment epithelial cells through inhibition of TLR4/JAK2/STAT3 pathway
- Role of reactive oxygen species in epithelial-mesenchymal transition and apoptosis of human lens epithelial cells
- Electroacupuncture alleviates ciliary muscle cell apoptosis in lens-induced myopic guinea pigs through inhibiting the mitochondrial signaling pathway
- De novel heterozygous copy number deletion on 7q31.31-7q31.32 involving TSPAN12 gene with familial exudative vitreoretinopathy in a Chinese family
