Uterine artery pseudoaneurysm after subtotal hysterectomy: a case report
2023-11-27TingXuXiaoboWangRuoanJiangWenLiShengtingYinHaiyangTangHaizhenDaiXiaoxiaBai
Ting Xu, Xiaobo Wang, Ruo’an Jiang, Wen Li, Shengting Yin, Haiyang Tang, Haizhen Dai, Xiaoxia Bai,2,3,4
1Department of Obstetrics and Gynecology, Women’s Hospital Zhejiang University School of Medicine, Hangzhou 310006, China
2Traditional Chinese Medicine for Reproductive Health Key Laboratory of Zhejiang Province, Hangzhou 310006, China
3Zhejiang Provincial Clinical Research Center for Obstetrics and Gynecology, Hangzhou 310006, China
4Key Laboratory of Women’s Reproductive Health, Hangzhou 310006, China
Vaginal bleeding is a common symptom in the emergency department of obstetrics and gynecology hospitals; however, post-hysterectomy vaginal bleeding is a rare phenomenon.Uterine artery pseudoaneurysm (UAP)is a rare condition that can lead to fatal bleeding and most commonly occurs as a long-term complication after invasive surgery or even in non-invasive procedures, such as cesarean section, myomectomy, dilatation and curettage, cervical conization and vaginal delivery.[1-3]Pseudoaneurysm is a pulsatile hematoma formed after arterial injury and rupture.The aneurysmall wall of a pseudoaneurysm is made of loose connective tissue, as opposed to a true aneurysm, which has three intact walls.The wall of a pseudoaneurysm is more likely to rupture under turbulent blood flow, resulting in intermittent and sometimes fatal bleeding.We report herein a rare case of UAP following a subtotal hysterectomy and provide details on the treatment strategies.
CASE
A 33-year-old woman, gravida 2, para 2, was admitted to our hospital due to significant vaginal bleeding 36 d after cesarean section and subtotal hysterectomy.The patient underwent an urgent cesarean section due to preterm labor and a scarred uterus in a local hospital.The procedure went smoothly.After cesarean section, severe postpartum hemorrhage occurred due to uterine atony.The blood loss was approximately 3,000 mL.Conservative treatment was ineffective;therefore, the patient underwent emergent subtotal hysterectomy and accepted transfusion perioperatively.She was discharged on the 11thpostoperative day.After surgery, the patient’s leucorrhea had a peculiar smell together with a small amount of blood.On the 36thpostoperative day, the patient suddenly experienced brisk vaginal bleeding without obvious inducement and was immediately sent to the local hospital by ambulance.At the local hospital, speculum examination revealed no active bleeding; the cervix was normal and closed.Local ultrasound suggested a cystic hypoechoic mass in the cervix, which was considered to be an arteriovenous fistula.Due to the limited medical resources of the local hospital, the patient was transferred to our hospital promptly for further investigation.There was no obvious vaginal bleeding during the transfer and admission.The patient had stable vital signs and no abdominal tenderness on admission, with a hemoglobin level of 95 g/L.Transabdominal pelvic ultrasound revealed a welldefined hypoechoic mass measuring 2.5 cm × 2.8 cm× 2.4 cm on the upper right side of the cervical stump,which showed an internal blood flow signal (Figure 1).Computed tomography angiography (CTA) of the abdomen revealed a 2.9 cm × 2.3 cm × 2.5 cm sac supplied by the right uterine artery, which was presumed to be a UAP.
Approximately three hours after admission, the patient suddenly presented with brisk and durative vaginal bleeding on the ward.Hence, she was immediately transferred to the theatre.Using the Seldinger technique, the catheter was inserted into the right femoral artery, and uterine arteriography revealed a tumor-like vascular mass arising from the distal residual right uterine artery; the leakage of contrast agent was evident (Figure 2A).During the operation, the patient continued bleeding, and the volume of vaginal bleeding accumulated to 1,700 mL.The patient presented with hemorrhagic shock and immediately received vigorous rehydration and blood transfusions.The rescue team arrived promptly and sped up the uterine artery embolization (UAE).A 4 mm × 4 cm microcoil was deposited into the neck of the pseudoaneurysm, and the right uterine artery was embolized with gelfoam.Repeated arteriograms demonstrated complete occlusion of the pseudoaneurysm (Figure 2B).The vaginal bleeding was reduced significantly, and the vital signs of the patient gradually stabilized after embolization.Six days after surgery, the patient underwent a uterine artery CTA scan, which showed that the microcoil was in the stump of the right uterine artery as expected, without extravasation of contrast agent (Supplementary Figure 1).The patient finally recovered and was discharged home one week post-embolization.The patient was followed up at 16 months post-embolization and no abnormal symptoms were observed.
DISCUSSION
Emergency postpartum hysterectomy is considered a final treatment for severe postpartum hemorrhage (PPH)that is unresponsive to conservative management.Due to its short surgical time, minimal bleeding and trauma,subtotal hysterectomy is the preferred option over total hysterectomy for PPH.Although it is extremely rare,the occurrence of UAP after hysterectomy has been documented.A search conducted on PubMed revealed only six reported cases between 1997 and 2023.[4-8]These existing cases either occurred after total hysterectomy or did not specify the surgical method.To the best of our knowledge, our patient represents the first case of UAP after subtotal hysterectomy.Furthermore, all the current cases underwent hysterectomy due to gynecological diseases, while our case underwent cesarean hysterectomy for PPH.With regard to the surgical approach, the previous cases of UAP after abdominal,[5,8]laparoscopic,[7]vaginal[6]and laparoscopic-assisted vaginal[4]hysterectomy.Thus, UAP after hysterectomy may not relate specifically to a surgical approach.According to the literature, pseudoaneurysm after hysterectomy presents as lower abdominal pain, postoperation fever, and vaginal bleeding.[4-8]In half of the patients, the first symptom was vaginal bleeding, while the other half experienced fever and abdominal pain.Only one patient had no symptoms of vaginal bleeding.The interval between symptom onset and surgery ranged from 6 d to 17 d.However, in this case, the patient developed symptoms 36 d after surgery.Generally,pseudoaneurysm has no specific manifestation and may occur even more than 1 month after hysterectomy;therefore, an insufficient understanding of UAP can easily lead to missed diagnosis or misdiagnosis.
In previous cases, UAP was diagnosed by color Doppler ultrasonography, computed tomography (CT),and angiography.Ultrasound, especially transvaginal ultrasonography, is the most important method for diagnosing UAP after subtotal hysterectomy.The ultrasound diagnosis is based on the to-and-fro blood flow in the neck of the aneurysm.In contrast to arteriovenous fistulas, the systolic phase of the UAP features high-velocity blood flow while the diastolic phase features reverse moderate flow.Although it has been reported that the diagnostic specificity of ultrasonography is approximately 95%,[1]the blood supply of UAPs cannot be clearly identified by ultrasonography.Angiography is the gold standard for the diagnosis of UAP and helps to identify the supplying arteries and provides guidance for subsequent uterine artery embolization.
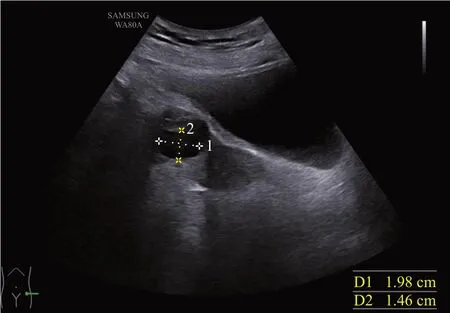
Figure 1.The result of transabdominal pelvic ultrasound.Hypoechoic mass on the upper right side of the cervical stump.
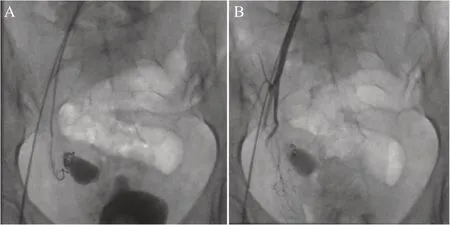
Figure 2.Results of the uterine artery angiography.A: arteriography revealed a pseudoaneurysm arising from the distal residual right uterine artery; B: post-embolization arteriogram showing complete occlusion of the pseudoaneurysm.
Since the UAP may rupture at any time and be life-threatening, active treatment should be performed once UAP is diagnosed.Treatment options include conservative therapy, surgery, and selective arterial embolization.In one case, conservative treatment(vaginal gauze packing) was used to stop the bleeding but failed.[5]Two patients underwent transvaginal vault suturing and packing for hemostasis, one of whom failed and the other recurred 12 h later.[4]This procedure is extremely challenging because of the difficulty in locating the bleeding and the fragile edema of the vaginal stump.Therefore, vaginal vault suturing and vaginal packing (with gauze or a balloon) are suitable for rapid hemostasis in primary healthcare setting with limited medical resources.Kumar et al[5]performed exploratory laparotomy to ligate the bilateral internal iliac arteries; however, this was not effective.This was thought to be due to the abundant collateral circulation,resulting in a low success rate of internal iliac artery ligation.Currently, UAE is the preferred treatment for UAP, which usually involves gelfoam, microcoils, or polyvinyl alcohol as embolic agents.Regardless of the embolic material, the uterine artery collateral circulation can be reconstructed in approximately 3 d, which may cause recurrent bleeding in the UAP.Therefore, the recommendation is to embolize the contralateral uterine artery at the same time.It is worth mentioning that the blood vessels are mostly recanalized in approximately three weeks after UAE with gelfoam, which may lead to hemorrhage.[7]Hence, most UAP patients are embolized with coils or various composite materials.[6,8]
CONCLUSION
Patients undergoing hysterectomy through any surgical approach, especially those with postoperative infection, are still at risk of UPA even 1 month after surgery.In particular, UPA should first be considered in cases involving massive vaginal bleeding after hysterectomy.Emergency physicians need to perform targeted ultrasonography and angiography to confirm the diagnosis and timely perform UAE to avoid progression and save lives.
Funding:Zhejiang Province Health Innovative Talent Project(A0466), Key Projects of the Science and Technology Coconstruction by National Administration of Traditional Chinese Medicine and Zhejiang Provincial Administration of Traditional Chinese Medicine (GZY-ZJ-KJ-23082).
Ethical approval:Not needed.
Conflicts of interest:The authors declare that they have no competing interests.
Author contribution:TX and XBW contributed equally to this research.The article was conceived by TX and XBW.RAJ and WL collected the clinical data and provided radiological photographs.STY and HZD reviewed and analyzed the literature.TX drafted the article and was critically revised by XXB and HYT.All the authors have read and approved the final manuscript.
All the supplementary files in this paper are available at http://wjem.com.cn.
杂志排行
World journal of emergency medicine的其它文章
- Hemorrhagic pancreatitis from fenofibrate and metformin toxicity: a case report
- Omadacycline for the treatment of Legionella pneumophila pneumonia caused by drowning: a case report
- A case of pulmonary mucormycosis presented with cardiac arrest
- Pyopneumothorax caused by Parvimonas micra and Prevotella oralis: a case report
- The effect of prophylactic antibiotics in acute upper gastrointestinal bleeding patients in the emergency department
- The effects of hyperbaric oxygen therapy on paroxysmal sympathetic hyperactivity after cardiopulmonary resuscitation: a case series
