Hemorrhagic pancreatitis from fenofibrate and metformin toxicity: a case report
2023-11-27MarcusAikBengLeeMingweiNgPaulYugendraYijuYaoPonampalamBoonKiatKennethTan
Marcus Aik Beng Lee, Mingwei Ng, Paul Yugendra, Yiju Yao, R Ponampalam, Boon Kiat Kenneth Tan
1 Department of Emergency Medicine, Singapore General Hospital, Singapore 169608, Singapore
2 Analytical Toxicology Laboratory, Health Sciences Authority, Singapore 169078, Singapore
Fibrates have been used for over forty-odd years to manage dyslipidemia and are generally considered safe and well-tolerated.[1]However, little is known about the toxicity of fibrates in overdose,[2]and most of the knowledge about fibrate toxicity comes from extrapolated observations of adverse effects encountered at therapeutic doses instead.Cholelithiasis, pancreatitis, hepatic enzyme derangement,acute kidney injury, myopathies leading to rhabdomyolysis,thromboembolism, skin photosensitivity and atrial fibrillation have been reported as rare but clinically-relevant adverse events from the therapeutic use of fibrates.[3]
Metformin, a biguanide oral hypoglycemic agent, is commonly used as first-line therapy for type II diabetes mellitus.However, metformin is highly toxic in overdoses and has been associated with metformin-associated lactic acidosis (MALA) through inhibition of mitochondrial function leading to cellular hypoxia.[4]Metformin toxicity and MALA have been reported even at therapeutic dosing, with risk factors including advanced age over 60 years old.[4]Other lethal complications include haemolytic anaemia, pancreatitis and altered mental status – in some cases leading to multiorgan failure and death.[5]
In this case report, we demonstrate how physicians should keep acute poisoning as a possible differential in any critically ill patient on metformin and fenofibrate presenting with haemorrhagic pancreatitis and severe lactic acidosis.
CASE
An intellectually disabled 60-odd-years-old woman was brought to the emergency department after family members found her weak and lethargic.She presented with vomiting for two days, associated with poor oral intake.She complained of giddiness but denied any headache, chest pain, focal neurological deficit or abdominal pain.She had no recent falls or head injuries.
The patient had extensive chronic conditions including hypertension, dyslipidemia and diabetes,while her prescribed medications included bisoprolol,amlodipine, linagliptin, metformin, fenofibrate,atorvastatin and iron tablets.Her family members helped with medication administration and were confident that drug overdose was unlikely.
On arrival at the emergency department, the patient was hypotensive with a blood pressure of 96/63 mmHg(1 mmHg=0.133 kPa) and a pulse rate of 87 beats/min.She was managed in the resuscitation area and fluid resuscitation with 2 L of intravenous crystalloids was started immediately.On examination, she was drowsy and her mucous membranes were dry.The rest of the physical examination was largely unremarkable.
The patient’s blood pressure remained low despite fluid resuscitation and deteriorated to a nadir of 69/37 mmHg.Intravenous noradrenaline was initiated for hemodynamic support once central venous access was secured.The initial impression was septic shock from a gastrointestinal source and she was given intravenous ceftriaxone and metronidazole.She eventually required intubation for airway protection to prevent aspiration in view of worsening drowsiness.Initial blood results showed severe metabolic acidosis from hyperlactatemia and a computed tomography mesenteric angiogram was therefore performed.Although this did not demonstrate bowel ischemia, it revealed peripancreatic fluid with a small focus of haemorrhage, suggestive of acute haemorrhagic pancreatitis.In particular, computed tomography did not show any biliary disease or choledocholithiasis that could have caused pancreatitis.Blood tests revealed increased lipase (>600 U/L) which was consistent with pancreatitis (Supplementary Table 1).The patient was subsequently admitted to the Medical Intensive Care Unit (MICU) for further management(Supplementary Figure 1).
In the MICU, her empirical antibiotic therapy was escalated to first piperacillin/tazobactam and then meropenem in view of refractory hypotension as septic shock remained a strong differential for her undifferentiated presentation.Blood toxicology was dispatched and the Toxicology team was consulted in view of inappropriate bradycardia in the setting of profound hypotension, raising suspicion for possible overdose on beta-blockers, calciumchannel antagonists, metformin or iron.After discussion with Toxicology team, 50 g of activated charcoal, 20 mL of 10% calcium gluconate, 5 mg glucagon, 50 mg methylene blue and hyperinsulinemic euglycemic therapy(1 U/kg bolus, followed by 0.5 U/[kg·h] infusion) were started.Continuous renal replacement therapy (CRRT)was also initiated for enhanced elimination.Despite initial treatment, the patient remained hypotensive and required the addition of both intravenous vasopressin and adrenaline for hemodynamic support.Extracorporeal membrane oxygenation was explored but was deemed to be of no benefit because her cardiac contractility was relatively preserved on bedside echocardiogram, suggesting vasodilatory shock rather than cardiogenic shock.Lipid emulsion therapy was then commenced as salvage therapy in three 100 mL boluses, followed by maintenance infusion therapy at 75 mL/h over 3 h (Figure 1).
The patient’s drug screen results returned on the second day and revealed supratherapeutic levels of fenofibrate, metformin and amlodipine (Table 1).In particular, fenofibrate levels were nearly five times above the upper limit of the therapeutic range, while metformin levels were also within the toxic range.Only traces of linagliptin were detected.Her serum iron level was 29 mmol/L, within the therapeutic range.Hyperinsulinemic euglycemic therapy that had been started empirically was stopped since there was no beta-blocker or calciumchannel antagonist toxicity.
The patient also required multiple blood product transfusions (30 U of cryoprecipitate, one pack of platelets and two packed red blood cells) because she developed disseminated intravascular coagulopathy but without any overt bleeding.CRRT was continued for 3 d until the patient was producing urine and her blood results had normalized.
Her condition continued to improve with supportive management and she was extubated and transferred out of the MICU on Day 4.Her acute pancreatitis resolved gradually with conservative management.Her serum lipase levels down-trended from >600 U/L on presentation, to 316 U/L on Day 4 and 291 U/L by Day 6.Her acute peripancreatic collection was still persistent on follow-up imaging at two weeks.She was eventually transferred to a nursing home due to care issues after a lengthy hospitalization of 44 d.
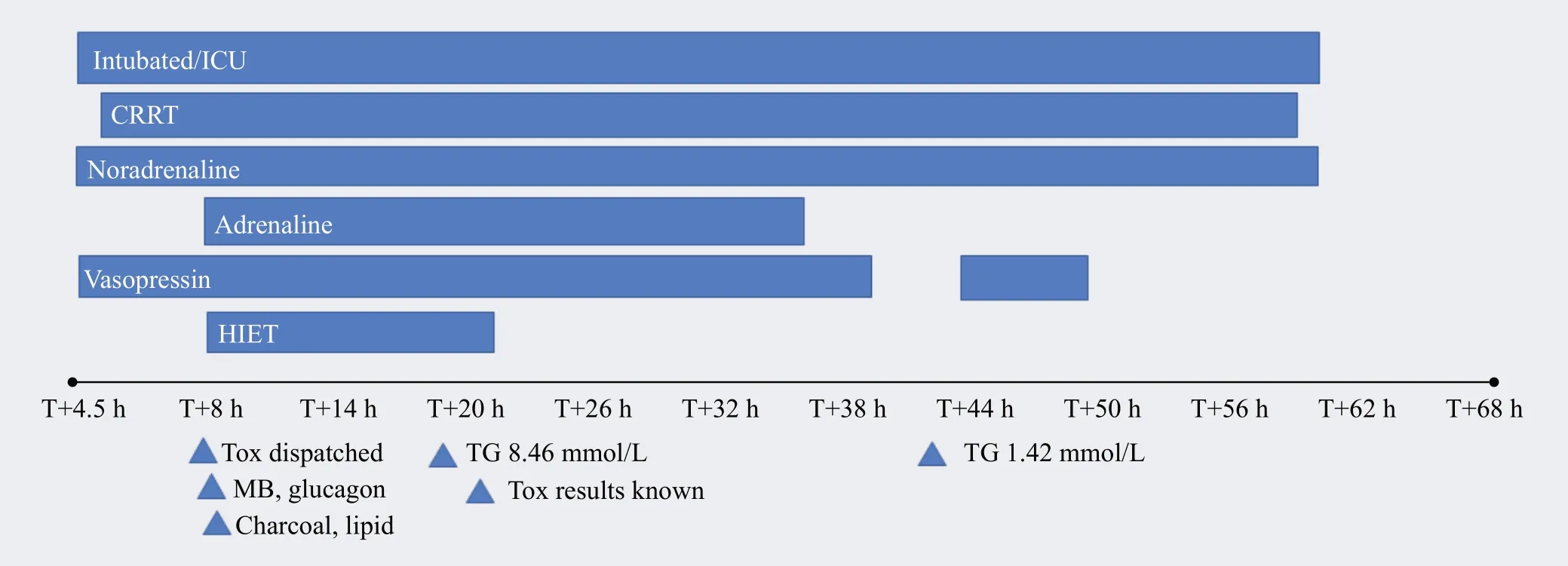
Figure 1.Progress in medical intensive care unit.Tox: toxicology; MB: methylene blue; CRRT: continuous renal replacement therapy; HIET:hyperinsulinemic euglycemic therapy; TG: triglycerides.

Table 1.Results of blood toxicology levels
DISCUSSION
Medications are a well-established cause of acute pancreatitis.However, the commonly-cited offending medications are usually thiazide and furosemide diuretics,sulphonamides, azathioprine and antimicrobials such as anti-retroviral agents.Several large randomized controlled trials and case reports in the literature have cited both metformin and fibrates as possible but less common causative agents of pancreatitis as well.In particular, a metaanalysis by Preiss et al analysed seven fibrate trials and found a relative risk of 1.39 for developing pancreatitis with fibrate therapy.[6]Interestingly, linagliptin – an anti-diabetic dipeptidyl peptidase-4 (DPP-4) inhibitor that this patient was also on – has also been associated with pancreatitis,although this patient’s blood toxicology levels only yielded traces of linagliptin.[7]
The pathophysiology of metformin-induced pancreatitis remains poorly understood.It has been postulated that this could be due to direct toxicity to the pancreatic acinar cells leading to intercellular leakage of digestive enzymes from the pancreatic ductules.[8]However, metformin-induced pancreatitis has also occurred at therapeutic dosing in the absence of impaired kidney function causing accumulation,[9]which leaves this theory wanting.While most authors hypothesize that fibrate-induced pancreatitis is likely due to the lithogenic potential of fibrates which increases biliary cholesterol saturation leading to gallstone precipitation, Kassim et al[10]highlighted a case of recurrent fenofibrate-induced pancreatitis with no evidence of biliary stones or sludge on endoscopic ultrasound which again suggests that unexplained mechanisms may be involved.
Yet other authors have suggested that acute pancreatitis could also have been caused by hypertriglyceridemia– a confounder frequently observed in patients with metabolic syndrome as fibrates are first-line treatment for severe hypertriglyceridemia based on current guideline recommendations[11](given that statins are also associated with increased risks of pancreatitis).However,hypertriglyceridemia-induced acute pancreatitis was less likely in our patient because her baseline lipid panel five months prior was normal (Supplementary Table 2).
There are no known antidotes or specific treatments available for managing either metformin or fenofibrate toxicity.As most cases of drug-induced pancreatitis usually follow a relatively benign course, general supportive care should suffice.Patients who present early may benefit from activated charcoal or gastric lavage to achieve decontamination.Haemodialysis for drug elimination is recommended for metformin toxicity in the setting of severe MALA unresponsive to fluid resuscitation and sodium bicarbonate,[4]but is less useful for fenofibrate which demonstrates high plasma protein-binding.
Several case reports have described successful reversal of refractory vasoplegic shock from MALA with methylene blue.[12]Metformin is theorized to activate guanylyl cyclase pathways, leading to the release of nitric oxide that induces vascular endothelial smooth muscle relaxation and causes distributive shock.While the evidence is weak and limited mostly to case series, methylene blue is thought to overcome this vasoplegia by inhibiting guanylyl cyclase activity.[12]Methylene blue should therefore be considered as adjunct supportive treatment in severe hemodynamically unstable cases of MALA.
The use of lipid rescue has not been documented specifically in the context of fibrate toxicity but could be considered a feasible adjunct therapy based on the pharmacokinetics and lipophilic nature of fibrates.[13]Metformin, conversely, is unusually hydrophilic and should not respond well to lipid rescue.Doubts have been raised over the safety of lipid emulsion therapy for poisoning in the setting of acute pancreatitis but the evidence remains largely inconclusive.Most of the concerns stem from studies in the 1980s that found that total parenteral nutrition patients are at increased risk of pancreatitis from intolerance of high-concentration lipid emulsion.[14]However, long-term intravenous lipid emulsion has been safely used to improve nutrition in acute necrotic pancreatitis in more recent studies,[15]while the ESPEN guidelines on parenteral nutrition suggest that lipid emulsion remains safe and feasible even in pancreatitis with the caveat that triglycerides are monitored regularly to avoid hypertriglyceridemia.[16]Rosenblatt et al[17]also reported a case of local anaesthetic toxicity that was successfully resuscitated with lipid emulsion therapy and noted no evidence of pancreatitis on follow-up at two weeks.Indeed, different formulations of intravenous lipids (enriching lipids with medium-chain triglycerides or ω-3 fatty acids) were found to impact outcomes differently.[18]Moreover, lipid rescue is usually administered in a large quantity over a short period of time,with the intent of creating a lipid sink that can sequester lipophilic toxins.This significantly differs from how total parenteral nutrition is administered, which is as a continuous infusion over a prolonged period instead.As such, the same risks of total parenteral nutrition may not translate to lipid rescue for poisoning.
Plasmapheresis is another therapeutic modality that could prove beneficial for fibrate toxicity given that fibrates demonstrate high protein-binding.Yang et al[19]reported the first use of plasmapheresis to remove excessive bezafibrate in an end-stage renal failure patient with fibrate-induced rhabdomyolysis.Plasma exchange led to a dramatic reduction in bezafibrate levels while contributing to the elimination of creatine kinase and other toxic metabolites.Plasmapheresis is of limited benefit in metformin overdose because metformin is not bound to plasma proteins.[20]While plasmapheresis was considered for our patient, this extracorporeal therapy(alongside ECMO) was ultimately not pursued because discussions with the family (in view of the patient’s intellectual disability and care needs) established a ceiling on the extent of care.
CONCLUSION
Haemorrhagic pancreatitis is a rare complication of metformin and fibrate toxicity.Lipid rescue can be used with caution in such patients, as it can potentially lead to iatrogenic worsening of acute pancreatitis.This case illustrates the importance of maintaining an index of suspicion for drug-induced acute pancreatitis in patients on commonly-used diabetic medications (such as metformin and linagliptin) or dyslipidemia medications such as fenofibrate, especially since toxicity may be possible even with therapeutic dosing.This case also highlights how expedient blood toxicology results can guide the clinician to achieve timely confirmatory diagnosis and facilitate optimal management of critically ill patients.
Funding:None.
Ethical approval:As the patient has a background of intellectual disability, informed consent for publication was obtained from the next-of-kin instead.All efforts have been made to anonymize case details to protect patient confidentiality whilst preserving the scientific merit for discussion of the case.
Conflicts of interest:The authors report no potential conflicts of interest and have no financial disclosures to declare.All coauthors have agreed to publish the manuscript.
Author contribution:AMBL and MN were involved in drafting the initial manuscript.Both contributed equally to the writing of this manuscript.PY was involved in subsequent review of the draft manuscript.YJY provided critical interpretation of the blood toxicology results involved and case analysis.RP and BKKT provided critical review of the manuscript and were instrumental in providing guidance as subject matter content experts.
All the supplementary files in this paper are available at http://wjem.com.cn.
杂志排行
World journal of emergency medicine的其它文章
- Tension urinothorax as a reversible cause of cardiac arrest: a case report
- Omadacycline for the treatment of Legionella pneumophila pneumonia caused by drowning: a case report
- A case of pulmonary mucormycosis presented with cardiac arrest
- Pyopneumothorax caused by Parvimonas micra and Prevotella oralis: a case report
- The effect of prophylactic antibiotics in acute upper gastrointestinal bleeding patients in the emergency department
- The effects of hyperbaric oxygen therapy on paroxysmal sympathetic hyperactivity after cardiopulmonary resuscitation: a case series
