结肠支架联合腹腔镜手术治疗梗阻性左半结肠癌手术效果及中长期预后的观察评价
2023-11-13傅文龙高鹰路春雷郭明晓
傅文龙,高鹰,路春雷,郭明晓
结肠支架联合腹腔镜手术治疗梗阻性左半结肠癌手术效果及中长期预后的观察评价
傅文龙1,高鹰2,路春雷2,郭明晓2
1.锦州医科大学临沂市人民医院研究生培养基地,山东临沂 276007;2.临沂市人民医院普外科,山东临沂 276007
探讨结肠支架联合腹腔镜手术对梗阻性左半结肠癌患者短期手术效果和中长期预后的影响。选取临沂市人民医院2016年1月至2019年6月收治的67例梗阻性左半结肠癌患者,并按照不同治疗方式将患者分为支架组30例,急症组37例,另随机选取30例未梗阻的左半结直肠癌患者作为对照组,比较三组患者的短期疗效和中长期预后。三组患者的性别、年龄、体质量指数(body mass index,BMI)、美国麻醉医师协会(American Society of Anesthesiologists,ASA)评分、TNM分期、肿瘤部位、合并症等临床资料差异均无统计学意义(>0.05)。支架组及对照组患者的术中出血量、肠造口率、预防性小肠造口率、结肠造口率低于急症组,差异均有统计学意义(<0.05)。支架组及对照组患者的一期吻合率高于急症组,差异有统计学意义(2=14.80,<0.05)。支架组及对照组患者术后住院时间明显短于急症组,差异有统计学意义(=5.448,<0.05)。三组患者的手术时间、淋巴结清扫数目、术后电解质紊乱、术后白细胞水平、术后排气时间、术后进食时间、围手术期死亡、术后化疗等指标差异均无统计学意义(>0.05)。急症组的并发症发生率与切口感染率高于支架组和对照组,差异有统计学意义(0.05)。三组患者的吻合口瘘、切口出血、肺栓塞、肺部感染、下肢静脉血栓等指标差异均无统计学意义(>0.05)。三组患者的3年无病生存率和总生存率差异无统计学意义(>0.05)。对于梗阻性左半结肠癌患者,支架联合腹腔镜手术的治疗方式能减少造口,提高手术一期吻合率,减少并发症的发生,但对中远期生存没有明显影响。
肠道支架;结肠肿瘤;肠梗阻;腹腔镜手术;预后
结直肠癌是全球第三大常见的恶性肿瘤,近年来,我国每年的发病人数不断增加,据估计8%~13%结肠癌患者出现肠梗阻症状[1-3]。虽然大多数结直肠癌患者选择择期手术治疗,但大多数恶性梗阻患者需紧急手术干预,通常患者术前伴有贫血、基础代谢紊乱、营养不良、酸碱平衡紊乱、败血症和肠道准备不足等情况,导致术后并发症的发生率较高,尤其是吻合口漏的发生,易形成无功能的吻合口。为降低风险,大多数外科医生在肿瘤切除后选择进行Hartmann术式或预防性造口,这会使患者遭受极大的痛苦[4]。1991年首次报道了急性梗阻性结肠癌患者的姑息性治疗中使用自膨胀式金属支架(self‑expandable metal stents,SEMS)[5]。随后SEMS的使用扩大到潜在的可治愈的梗阻性病变,内镜下放置自膨胀式金属支架是一种非侵入性的介入技术,通过扩张结肠肿瘤的狭窄部分的肠管,快速缓解梗阻症状,将急症手术变为择期手术,从而降低死亡率和造口率,改善患者术后生活质量。在临床工作中SEMS作为过渡到择期手术的桥梁(bridge to surgery,BTS),逐渐取代急诊手术用于治疗梗阻性结肠癌患者[6-8]。且随着微创手术的不断发展,腹腔镜手术得到广泛的应用,腹腔镜手术已逐渐成为治疗结直肠癌主要的手术方式[9]。本研究选取67例梗阻性左半结肠癌患者与30例未梗阻左半结肠癌患者进行回顾性研究,探讨结肠支架联合择期腹腔镜手术治疗梗阻性左半结肠癌的临床效果,现报道如下。
1 资料与方法
1.1 一般资料
选取2016年1月至2019年6月临沂市人民医院收治的梗阻性左半结肠癌患者的临床资料。纳入标准:①影像学检查(CT或MRI)提示结肠脾区及远端结直肠占位;②临床上出现梗阻症状(腹胀、腹痛、恶心或呕吐);③肠镜及病理证实为恶性肿瘤;④结肠脾区肿瘤及远端结直肠放置支架后无并发症(出血、穿孔)发生。排除标准:①严重心肺功能障碍或拒绝手术治疗;②肿瘤多发远处转移结节;③临床资料遗失或随访失联;④术前接受辅助化疗。根据纳入及排除标准纳入研究对象并分组:支架组30例(支架扩张联合限期腹腔镜手术)和急症组37例(急诊开腹手术),另随机选取30例未梗阻左半结直肠癌患者作为对照组(限期腹腔镜手术)。本研究经临沂市人民医院医学伦理委员会批准(伦理审批号:YX200530),患者术前均签署知情同意书。
1.2 围手术期处理
患者出现肠梗阻症状(腹痛、腹胀、呕吐、停止排气和排便),影像学提示左半结肠占位,进行肠镜检查并取活检进行病理检查证实为结肠癌,放置自膨胀式金属支架。支架置入成功的标准:X线或CT显示SEMS完全扩张,支架完全覆盖肿瘤,并且狭窄段肿瘤位于支架的中间。临床成功标准:患者在支架置入后数小时内开始排便、排气,腹痛、腹胀、呕吐等症状消失或减轻。放置支架后没有发生急性并发症(穿孔、出血等)或支架发生位移,复查腹部CT了解SEMS是否通畅。给予营养支持、功能锻炼和心理疏导等治疗,2~4周后择期进行手术。术前准备(禁饮食、口服泻药、清洁灌肠),根据肿瘤位置和术中探查情况决定治疗方案(一期肿瘤切除+肠管吻合或预防性造口)。对照组患者完善术前检查,择期行腹腔镜手术,急症组患者在入院后24h内进行急诊开腹手术,根据术中情况采用术式:①Hartmann术;②术中近段肠管减压灌洗,一期切除吻合或预防性小肠造口术。
1.3 观察指标
①患者的一般资料:性别、年龄、体质量指数(body mass index,BMI)、美国麻醉医师协会(American Society of Anesthesiologists,ASA)评分、肿瘤部位、合并症、TNM分期,合并症包括:糖尿病、高血压、冠状动脉粥样硬化性心脏病、脑梗死。②术中及术后观察指标:手术时间、术中出血量、淋巴结清扫数目、术后电解质紊乱、术后白细胞水平、术后排气时间、术后进食时间、肠造口率、预防性小肠造口率、结肠造口率、一期吻合率、围手术期死亡、术后住院时间、术后化疗。③术后并发症:切口感染、吻合口瘘、肺栓塞、切口出血、肺部感染、下肢静脉血栓。④长期随访采取病例查阅、电话随访和患者复诊的形式进行,包括无病生存率和总生存率,随访截至2022年6月。
1.4 统计学方法
2 结果
2.1 三组患者的一般资料比较
三组患者的性别、年龄、肿瘤部位、BMI、ASA评分、TNM分期、合并症差异无统计学意义(>0.05),见表1。
2.2 三组患者术中及术后观察指标的比较
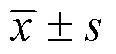
支架组及对照组患者的术中出血量、肠造口率、预防性小肠造口率、结肠造口率均明显低于急症组,差异有统计学意义(<0.05);支架组及对照组的一期吻合率显著优于急症组,差异有统计学意义(2=14.80,<0.05);三组患者的术后住院时间分别为(9.33±2.53)d、(8.93±1.46)d、(10.54±2.12)d,支架组与对照组患者术后住院时间没有明显差异,但较急症组患者明显缩短,差异有统计学意义(=5.448<0.05)。三组患者的手术时间、淋巴结清扫数目、术后电解质紊乱、术后白细胞水平、术后排气时间、术后进食时间、围手术期死亡、术后化疗等指标差异均无统计学意义(>0.05),见表2。
2.3 三组患者术后并发症的比较
三组患者术后并发症的发生率分别为45.9%、30.0%和16.7%,急症组并发症的发生率显著高于另外两组,差异有统计学意义(2=6.608,=0.037)。三组的切口感染率分别为18.9%、3.3%和3.3%,支架组及对照组的切口感染率显著低于急症组,差异有统计学意义(2=5.512,=0.037)。吻合口瘘、切口出血、肺部感染、肺栓塞、下肢静脉血栓等指标三组差异均无统计学意义(>0.05),见表3。
2.4 生存分析
随访结果显示:支架组的平均随访时间为(43.7±15.8)个月,对照组为(45.0±13.9)个月,急症组为(38.4±14.5)个月,三组间比较差异无统计学意义(=0.650)。三组患者的3年无病生存率分别为60.0%、70.0%和62.1%(2=0.730,0.690),总生存率为70.0%、76.6%和67.5%(2=0.690,0.700),差异均无统计学意义,见图1。

表1 三组患者的一般资料比较
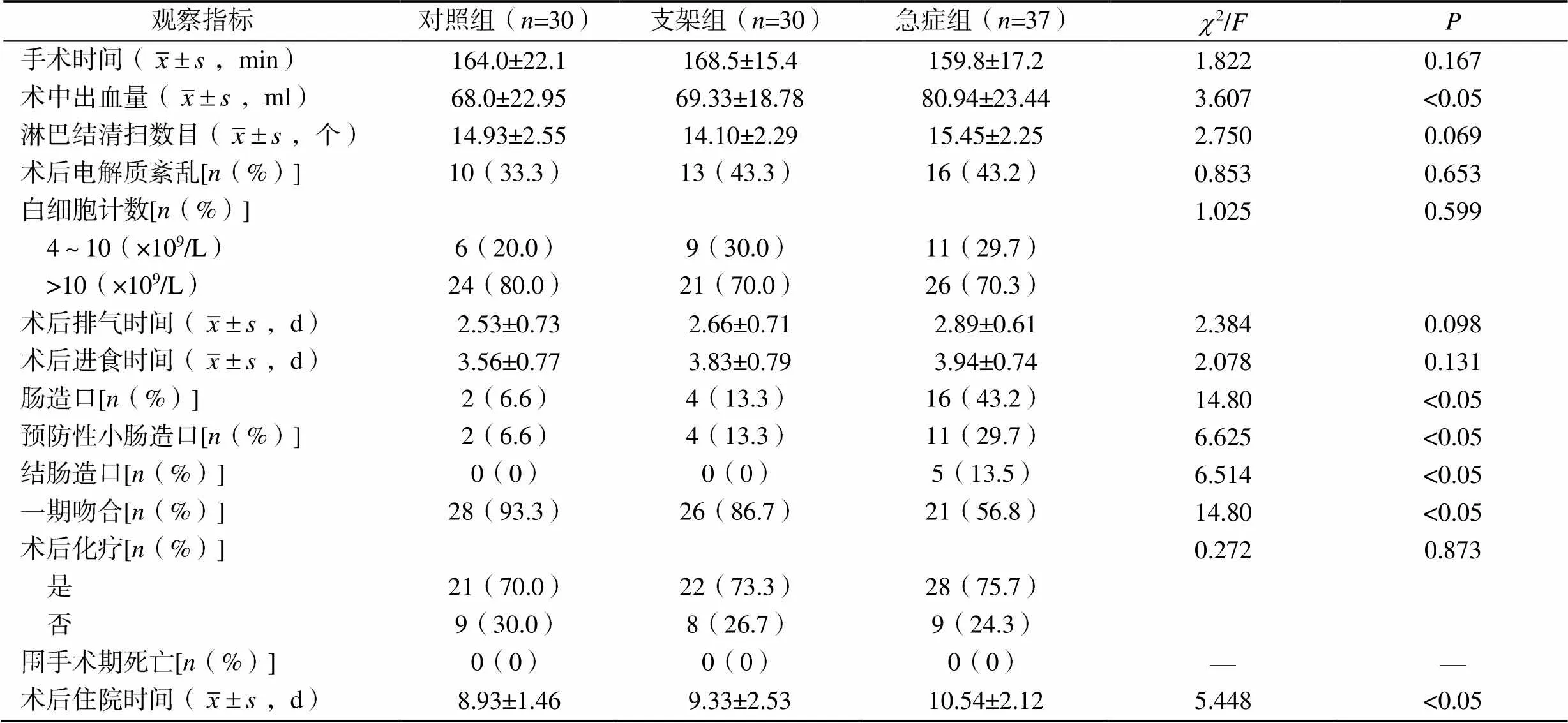
表2 三组患者术中及术后各项指标的比较
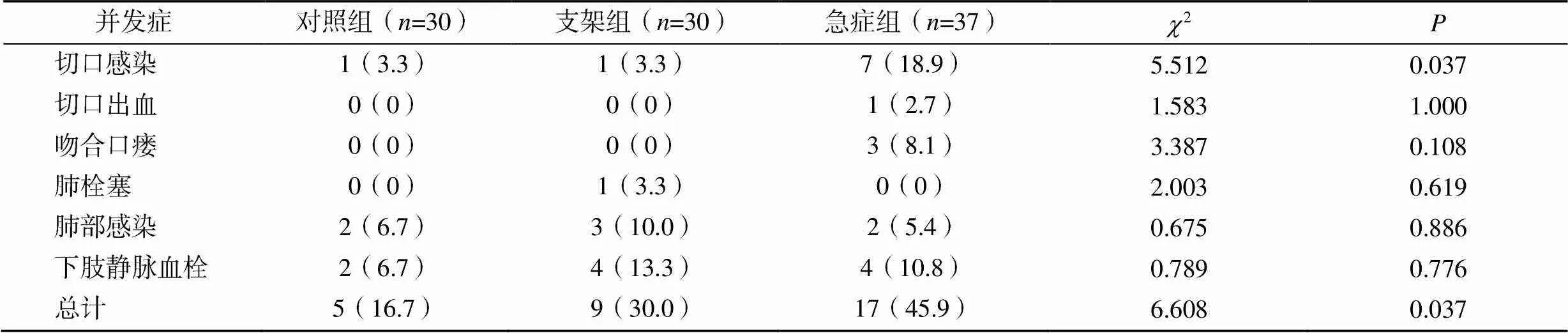
表3 三组患者术后并发症的比较[n(%)]
图1 三组患者的总生存率和无病生存率比较
A.总生存率比较;B.无病生存率比较
3 讨论
结直肠癌是消化系统中常见的恶性肿瘤之一,早期症状多不明显,肿瘤进展至中晚期阶段多引起相关症状,其中肠梗阻较为常见,约70%的梗阻发生于左半结肠。由于梗阻性结肠癌患者以老年人为主,营养状态差,身体功能下降,且多数患者伴有基础疾病,手术耐受力较差,病情发展较快而临床症状不典型,若治疗不及时易造成严重后果[10-12]。另外,由于左半结肠的特殊结构与回盲瓣形成抗反流的特殊作用,容易形成闭袢性肠梗阻,造成肠管内粪便淤积,肠道内细菌繁殖产生大量肠毒素,肠壁静脉回流不畅,大量肠道细菌移位,造成近端肠管扩张、肠壁水肿、弥漫性腹膜炎和感染性休克的发生,梗阻症状逐渐加重造成肠道内压力不断增加,最终肠道破裂或穿孔。结直肠癌合并急性梗阻一旦明确诊断,需及早进行手术探查与治疗[13]。早期传统分期手术是治疗左半结肠癌合并肠梗阻患者的主要手术治疗方案,主要分为一期造口术和二期还纳手术,然而分期手术有创伤大、恢复慢、增加造口等缺点,严重影响患者术后的生活质量。而SEMS联合限期腹腔镜手术的治疗模式,通过充分术前准备,避免分期手术[14]。
本研究中,SEMS作为梗阻性结肠癌治疗的过渡环节,很好地解决了梗阻问题,为后续腹腔镜微创手术提供机会,从而提高手术一期吻合率、降低造口率,短期内的效果更具优势,且风险更小,与Arezzo等[15]研究结论一致。降低术后并发症的发生率是手术有效性和安全性的重要判断标准之一,Jain等[16]分析发现,与急诊手术相比SEMS短期并发症的可能性降低,与本研究结果一致。可能是放置SEMS后肠梗阻得到有效缓解,排便功能得到保留,患者可恢复进食,经充分术前评估,治疗基础疾病,改善肠道功能,可一定程度上减少麻醉风险,提高手术耐受力,避免急诊手术的风险[17-18]。Li等[19]研究发现,SEMS联合择期腹腔镜手术与未梗阻性左半结肠癌患者围手术期的各项指标水平相当,短时间内的临床效果类似,与本研究结果一致。陈赜[20]分析SEMS联合择期手术治疗梗阻性结肠癌患者,发现梗阻的解除及术前状态的改善,能加快术后排气,减少术中出血,缩短住院时间,另有研究也取得类似的结果[21]。本研究支架组患者的手术出血量明显减少,术后住院时间明显缩短,可能是腹腔环境下进行手术,肠道扩张较少,伤口表面积减少,明确肿瘤与周围组织的关系,更能完整地切除肿瘤组织,减少正常组织损伤,从而减少出血。此外,患者通过围手术期内的多模式干预措施最大限度地减少术后应激反应,改善预后及减少术后并发症的发生,缩短住院时间,降低患者的医疗成本[22-23]。
本研究中,三组患者的3年无病生存率和总生存率比较差异无统计学意义。表明SEMS联合腹腔镜手术治疗方式对梗阻性结肠癌患者远期生存没有明显影响。与Kim等[24]研究结果相似;此外,一项前瞻性研究将接受SEMS治疗的急性梗阻性结肠癌患者与结直肠癌患者术后的生存时间进行比较,结果显示两组患者1年、5年和10年生存率差异无统计学意义,SEMS的应用没有对远期生存产生影响,但此结论需进一步证实[25]。本研究为回顾性研究,存在不足之处,如样本量较小,检验效能可能受到影响,且随访时间相对较短,故尚需更大样本量、更长的随访时间及更多的前瞻性比较研究来评估支架联合腹腔镜手术治疗梗阻性左半结肠癌患者的效果、安全性和长期疗效。
综上,对于梗阻性左半结肠癌的患者采用SEMS联合腹腔镜手术的治疗方式,不仅能提高手术一期吻合率、减少造口、缩短术后住院时间、减少并发症的发生、加速患者康复,而且对患者远期生存没有明显影响,值得在临床中推广应用。
[1] 谢丽, 戴卫星, 郭天安, 等. 中国结直肠癌1988—2009年发病率和死亡率趋势分析[J]. 中华胃肠外科杂志, 2018, 21(1): 33–40.
[2] DE CEGLIE A, FILIBERTI R, BARON T H, et al. A meta-analysis of endoscopic stenting as bridge to surgery versus emergency surgery for left-sided colorectal cancer obstruction[J]. Crit Rev Oncol Hematol, 2013, 88(2): 387–403.
[3] VELD J V, BEEK K J, CONSTEN E C J, et al. Definition of large bowel obstruction by primary colorectal cancer: A systematic review[J]. Colorectal Dis, 2021, 23(4): 787–804.
[4] NASIRIZIBA F, SAATI M, HAGHANI H, et al. Correlation between self-efficacy and self-esteem in patients with an intestinal stoma[J]. Br J Nurs, 2020, 29(16): S22–S29.
[5] DOHMOTO M. NEW method-endoscopic implantation of rec-tal stent in palliative treatment of malignant stenosis[J]. Endoscigest, 1991, 3(11): 1507–1512.
[6] KIM S H, JANG S H, JEON H J, et al. Colonic stenting as a bridge to surgery for obstructive colon cancer: Is it safe in the long term?[J]. Surg Endosc, 2022, 36(6): 4392–4400.
[7] KHOMVILAI S, PATTARAJIERAPAN S. Comparison of long-term outcomes of colonic stenting as a “bridge to surgery” and emergency surgery in patients with left-sided malignant colonic obstruction[J]. Ann Coloproctol, 2023, 39(1): 17–26.
[8] MATSUDA A, YAMADA T, MATSUMOTO S, et al. Short-term outcomes of a self-expandable metallic stent as a bridge to surgery vs a transanal decompress-sion tube for malignant large-bowel obstruction: A Meta-analysis[J]. Surg Today, 2019, 49(9): 728–737.
[9] LUEDERS A, ONG G, DAVIS P, et al. Colonic stenting for malignant obstructions-A review of current indications and outcomes[J]. Am J Surg, 2022, 224(1 Pt A): 217–227.
[10] ATUKORALE Y N, CHURCH J L, HOGGAN B L, et al. Self-expanding metallic stents for the management of emergency malignant large bowel obstruction: A systematic review[J].J Gastrointest Surg, 2016, 20(2): 455–462.
[11] FLOR-LORENTE B, BÁGUENA G, FRASSON M, et al. Self-expanding metallic stent as a bridge to surgery in the treatment of left colon cancer obstruction: Cost-benefit analysis and oncologic results[J]. Cir Esp, 2017, 95(3): 143–151.
[12] SAMPER WAMBA J D, FERNANDEZ MARTÍNEZ A, GNZALEZ PÁSTRANA M, et al. Efficacy and complications in the use of self-expanding colonic stents: An analysis of 15 years[J]. Radiologia, 2015, 57(5): 402–411.
[13] 佴永军, 马永, 曹红勇, 等. 老年完全梗阻性结肠癌的急诊手术治疗[J]. 实用老年医学, 2019, 33(12): 1199–1202.
[14] 李昀昊, 林国乐. 左半结肠癌合并肠梗阻外科治疗策略[J]. 中国实用外科杂志, 2019, 39(12): 1287–1290.
[15] AREZZO A, PASSERA R, LO SECCO G, et al. Stent as bridge to surgery for left-sided malignant colonic obstruction reduces adverse events and stoma rate compared with emergency surgery: Results of a systematic review and Meta-analysis of randomized controlled trials[J]. Gastrointest Endosc, 2017, 86(3): 416–426.
[16] JAIN S R, YAOW C Y L, NG C H, et al. Comparison of colonic stents, stomas and resection for obstructive left colon cancer: A Meta-analysis[J]. Tech Coloproctol, 2020, 24(11): 1121–1136.
[17] VAN HOOFT J E, VELD J V, ARNOLD D, et al. Self-expandable metal stents for obstructing colonic and extracolonic cancer: European society of gastrointestinal endoscopy (ESGE) guideline-update 2020[J]. Endoscopy, 2020, 52(5): 389–407.
[18] 曾维根, 庞国义, 赵琦, 等. 梗阻性左半结肠癌支架置入后手术方式的选择[J]. 中华肿瘤防治杂志, 2021, 28(16): 1253–1257.
[19] LI W, JIN X, LIANG G, et al. The efficacy of endoscopic stenting combined with laparoscopy in the treatment of left colon cancer with obstruction[J]. J Cancer Res Ther, 2019, 15(2): 375–379.
[20] 陈赜. 肠道支架置入术与急诊手术治疗急性梗阻性结直肠癌疗效观察[J]. 临床医药文献电子杂志, 2018, 5(67): 82–83.
[21] TAMAGAWA H, AOYAMA T, NUMATA M, et al. A comparison of open and laparoscopic-assisted colectomy for obstructive colon cancer[J]. In Vivo, 2020, 34(5): 2797–2801.
[22] TAN L, LIU Z L, RAN M N, et al. Comparison of the prognosis of four different treatment strategies for acute left malignant colonic obstruction: A systematic review and network meta-analysis[J]. World J Emerg Surg, 2021, 16(1): 11.
[23] GUSTAFASSON U O, SCOTT M J, HUBNER M, et al. Guidelines for perioperative care in elective colorectal surgery: Enhanced recovery after surgery (ERAS®) Society Recommendations: 2018[J]. World J Surg, 2019, 43(3): 659–695.
[24] KIM M H, KANG S I, LEE J, et al. Oncologic safety of laparoscopic surgery after metallic stent insertion for obstructive left-sided colorectal cancer: A multicenter comparative study[J]. Surg Endosc, 2022, 36(1): 385–395.
[25] VERSTOCKT B, VAN DRIESSCHE A, DE MAN M, et al. Ten-year survival after endoscopic stent placement as a bridge to surgery in obstructing colon cancer[J]. Gastrointest Endosc, 2018, 87(3): 705–713.
Evaluation of surgical results and medium and long term prognosis of colon stenting combined with laparoscopic surgery for obstructive left hemi-colon cancer
FU Wenlong, GAO Ying, LU Chunlei, GUO Mingxiao
1.Postgraduate Training Base of Linyi People’s Hospital of Jinzhou Medical University, Linyi 276007, Shandong, China; 2.Department of General Surgery, Linyi People’s Hospital, Linyi 276007, Shandong, China
To investigate the effects of colonic stenting combined with laparoscopic surgery on short term surgical outcomes and medium and long term prognosis in patients with obstructive left hemi-colon cancer.A total of 67 patients with obstructive left hemico-rectal cancer admitted to Linyi People’s Hospital from January 2016 to June 2019 were selected and divided into 30 cases in the stent group and 37 cases in the acute group according to different treatment modalities, and another 30 patients with unobstructed left hemico-rectal cancer were randomly selected as the control group to compare the short term efficacy and medium and long term prognosis of patients in the three groups.The differences in clinicopathological data such as gender, age, body mass index (BMI), American Society of Anesthesiologists (ASA) score, TNM stage, tumor site, and comorbidities among the three groups were not statistically significant (>0.05). The bleeding volume, enterostomy rate, prophylactic small colostomy rate and colostomy rate in the stent group and control group were lower than those in the acute group, and the differences were statistically significant (<0.05). The stent group and the control group had a higher rate of first-stage anastomosis than the acute group, and the difference was statistically significant (2=14.80,<0.05). The postoperative hospital stay was significantly shorter in the stent and control groups than in the acute group, and the difference was statistically significant (=5.448,<0.05). There were no statistically significant differences between the three groups in terms of operative time, number of lymph node dissection, postoperative electrolyte disorders, postoperative white blood cell levels, postoperative time of exhaustion, postoperative time of feeding, perioperative death, and postoperative chemotherapy (>0.05). The incidence of complications and incisional infections in the acute group were statistically higher than those in the stent and control groups (<0.05). The differences in anastomotic fistula, bleeding from the incision, pulmonary embolism, pulmonary infection, and lower extremity venous thrombosis were no statistically significant among the three groups (>0.05). There was no statistically significant difference in the 3-year disease-free survival rate and overall survival rate among the three groups (>0.05).In patients with obstructive left hemicolonic cancer, stenting combined with laparoscopic surgery reduces stoma, improves the rate of one-stage surgical anastomosis, and reduces complications, but does not have a significant impact on mid- and long-term survival.
Intestinal stenting; Colon tumor; Laparoscopic surgery; Intestinal obstruction; Prognosis
R656.9
A
10.3969/j.issn.1673-9701.2023.30.001
国家自然科学基金项目(81500688);山东省自然科学基金资助项目(ZR2021MH362)
郭明晓,电子信箱:gmx1211@163.com
(2022–12–19)
(2023–10–12)
