Clinical observation of acupuncture treatment for children with accommodative myopia
2023-06-19ZHANGXiaopeng张小芃HANRong韩榕QIUXiaodi邱晓頔KONGXiehe孔谐和CAOYaojiani曹姚佳妮WANGXuejun王雪君ZHAOYue赵越ZHAOFeng赵峰MAXiaopeng马晓芃
ZHANG Xiaopeng (张小芃), HAN Rong (韩榕), QIU Xiaodi (邱晓頔), KONG Xiehe (孔谐和), CAO Yaojiani (曹姚佳妮),WANG Xuejun (王雪君), ZHAO Yue (赵越), ZHAO Feng (赵峰), MA Xiaopeng (马晓芃),
1 Yueyang Hospital of Integrated Traditional Chinese and Western Medicine, Shanghai University of Traditional Chinese Medicine,Shanghai 200437, China
2 Shanghai Qigong Research Institute, Shanghai 200030, China
3 Eye and ENT Hospital Affiliated to Fudan University, Shanghai 200031, China
4 Shanghai Research Institute of Acupuncture and Meridian, Shanghai 200030, China
5 Shuguang Hospital, Shanghai University of Traditional Chinese Medicine, Shanghai 201203, China
Abstract
Keywords: Acupuncture Therapy; Vision, Ocular; Axial Length, Eye; Myopia; Refractive Errors; Randomized Controlled Trial
In recent years, myopia has become increasingly serious at home and abroad[1].The incidence of myopia in China shows a trend of lower age and rapid progression[2], making it a major public health problem.Accommodative myopia (AM) is functional myopia resulting from continuous contraction of the ciliary muscles and excessive accommodation.This transient myopia can be improved by timely intervention, but if not alleviated in time, it may develop into axial myopia.Therefore, visual acuity screening and follow-up treatment for children with AM are important for myopia prevention and control.Acupuncture is a common method used in traditional Chinese medicine to treat AM, as it can unblock the meridians and reconcile ocular Qi and blood.This study took AM as the research object to observe the therapeutic effect of acupuncture on children with AM and to provide clinical research data for acupuncture treatment of AM.
1 Clinical Materials
1.1 Study subjects and grouping
In this study, 76 subjects were enrolled in the Optometry Clinic of Shuguang Hospital, Shanghai University of Traditional Chinese Medicine, and the observation period was between June 2021 and March 2022.After the guardians of the subjects signed the informed consent, the subjects were divided into a test group or a control group according to the random numbers and random assignment table generated by SPSS version 26.0 software, with 38 cases in each group.
This study was approved by the Ethics Committee of Shuguang Hospital, Shanghai University of Traditional Chinese Medicine (Ethics Approval No.2020-893-102-01) and registered in the Chinese Clinical Trial Registry(Registration No.ChiCTR2100041735).
1.2 Diagnostic criteria
The diagnostic criteria for AM in theVisual Optics and Refraction[3]were adopted.
1.3 Inclusion criteria
Met the diagnostic criteria for AM; aged 7-14 years,male or female; voluntary to participate in the trial with good compliance; informed consent was signed by his/her guardian.
1.4 Exclusion criteria
Those with other ocular diseases or a history of eye surgery; with systemic diseases; used atropine or other treatments for myopia control; unable to adhere to the treatment; those whose guardian held unreasonable expectations.
1.5 Criteria for discontinuation and dropout
Those who had experienced serious adverse events,serious complications, or specific physiological changes that precluded study continuation; did not follow the study protocol; did not continue with the trial regimen for whatever reason.
1.6 Criteria for elimination
Those who did not meet the inclusion criteria or met the exclusion criteria but were mistakenly included;with no follow-up data and only pre-treatment data available.
1.7 Statistical analysis
The full analysis set based on the intention-to-treat principle was used for data analysis in this study, and the last observation carried forward method was used for imputation.The statistical analysis was performed using SPSS version 26.0 software.The measurement data were expressed as mean ± standard deviationor mean ± standard error, and the counting data were expressed as the number of cases(percentage).Analysis was performed using generalized estimating equations, including a within-group factor(time), a between-group factor (grouping), and the interaction between the two.The results of multiple comparisons in separate effects analysis were adjusted according to Bonferroni’s method.All statistical results were considered significant withP<0.05.
2 Treatment Methods
2.1 Control group
Education on eye health was given.
2.2 Test group
The test group was treated with acupuncture in addition to the intervention used in the control group.
Points: Bilateral Cuanzhu (BL2), Taiyang (EX-HN5),Sibai (ST2), Fengchi (GB20), Hegu (Ll4), Guangming(GB37), and Taichong (LR3).
Methods: The points were located according to theNomenclature and Location of Acupuncture Points(GB/T 12346-2006)[4].Subjects took a sitting or supine position.After the doctors disinfected the hands and the point areas of the subject, needles of 0.25 mm in diameter and 25 mm in length were taken for acupuncture manipulation.The oblique needle insertion with a depth of 7.5-12.5 mm was adopted for Cuanzhu (BL15).The perpendicular needle insertion with a depth of 7.5-12.5 mm was adopted for Taiyang(EX-HN5).The oblique needle insertion with a depth of 15.0-20.0 mm towards the nose tip was adopted for Fengchi (GB20).The oblique or perpendicular needle insertion with a depth of 7.5-12.5 mm was adopted for Sibai (ST2).The perpendicular needle insertion with a depth of 12.5-20.0 mm was adopted for Hegu (Ll4),Guangming (GB37), and Taichong (LR3).The needles were retained for 20 min after the arrival of the needling sensation (Deqi).Then, the needles were slowly withdrawn to the subcutaneous layer and quickly pulled out.The doctor then pressed the needle hole with a sterile cotton ball.Treatment was given twice per week, 4 weeks as a course, for 2 courses.
3 Observation of Therapeutic Efficacy
3.1 Observation items
Relevant indicators were assessed before treatment,and 1 month and 2 months after treatment.All assessments were carried out by the same person in strict accordance with the requirements.
3.1.1 Uncorrected visual acuity (UCVA)
The standard logarithmic visual acuity chart was used to perform the UCVA examination.The results were statistically calculated in the form of logMAR.The smaller the value, the better the visual acuity.
3.1.2 Refraction
Refraction was measured before cycloplegia using an ARK-1 autorefractor (Nidek Corporation, Japan).Five consecutive measurements were made, and the results were averaged and recorded.
3.1.3 Axial length (AL)
AL was measured by an optical coherence tomography-based IOL-Master (Carl Zeiss Meditec, Inc.,Germany).Three consecutive measurements were taken and averaged.
3.2 Results
3.2.1 Comparison of the general data
During the study, 2 subjects did not complete the 2-month examination.One patient in the test group withdrew due to intolerability of acupuncture treatment, and 1 case in the control group was found to have reduced visual acuity after reexamination and chose other therapies.Both of them completed the first follow-up visit, and the missing data were filled by the last observation carried forward method.Finally, 38 people were included in each of the two groups for statistical analysis.There was no significant difference in age or gender between the two groups (P>0.05), as shown in Table 1.
3.2.2 Comparison of the UCVA
After 2 months of treatment, the UCVA in the control group was lower than that before treatment, with a statistically significant difference (P<0.05); the UCVA in the test group was higher than that before treatment,with statistical significance (P<0.05).After 1-month treatment, there was no significant difference in UCVA between the two groups (P>0.05).After 2-month treatment, the UCVA in the test group was better than that in the control group, and the difference was statistically significant (P<0.05).It is suggested that acupuncture treatment for 2 months can improve UCVA in children with AM.See Table 2.
3.2.3 Comparison of the refraction
After 1 and 2 months of treatment, the refractions of the two groups were significantly different from those before treatment (P<0.05).There was no significant difference in the refraction after 1 month and 2 months of treatment between the two groups (P>0.05).The results showed that myopic refraction improved after 2 months of treatment in both groups of subjects, but there was no statistically significant difference in the effect of the two intervention modalities on the refraction in children with AM.See Table 3.
3.2.4 Comparison of the AL
After 1 month and 2 months of treatment, the AL of the eye in the control group was significantly different from that before treatment (P<0.05); the AL in the test group was not significantly different from that before treatment (P>0.05).After 1 and 2 months of treatment,there was no significant difference in AL between the two groups (P>0.05).These results suggest that there is no statistical difference between the two interventions on AL of the eyes in children with AM.See Table 4.

Table 1 Comparison of the general data between the two groups
Table 2 Comparison of the UCVA between the two groups before and after treatment Unit: logMAR
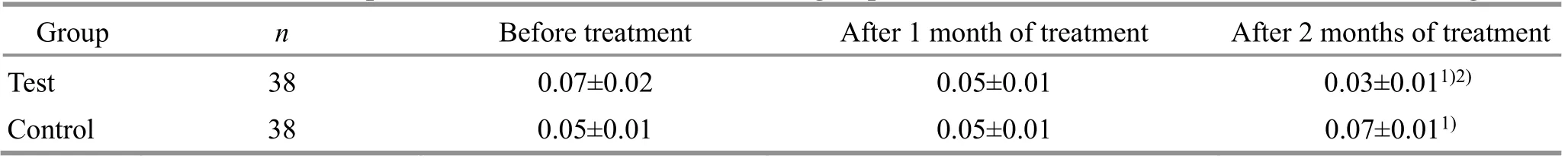
Table 2 Comparison of the UCVA between the two groups before and after treatment Unit: logMAR
Note: UCVA=Uncorrected visual acuity; compared with the same group before treatment, 1) P<0.05; compared with the control group, 2)P<0.05.
Group n Before treatment After 1 month of treatment After 2 months of treatment Test 38 0.07±0.02 0.05±0.01 0.03±0.011)2)Control 38 0.05±0.01 0.05±0.01 0.07±0.011)
Table 3 Comparison of the refraction between the two groups before and after treatment Unit: D
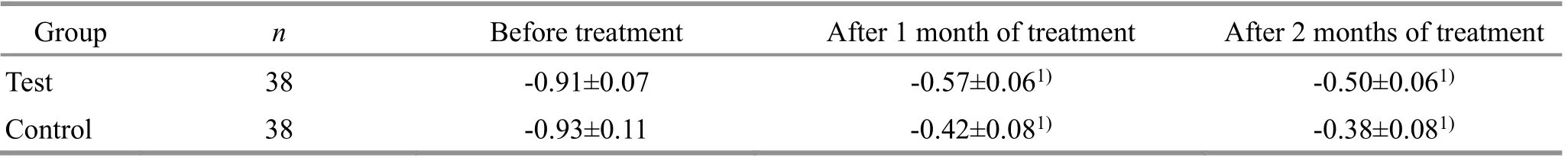
Table 3 Comparison of the refraction between the two groups before and after treatment Unit: D
Note: Compared with the same group before treatment, 1) P<0.05.
Group n Before treatment After 1 month of treatment After 2 months of treatment Test 38 -0.91±0.07 -0.57±0.061)-0.50±0.061)Control 38 -0.93±0.11 -0.42±0.081)-0.38±0.081)
Table 4 Comparison of the AL between the two groups before and after treatment Unit: mm

Table 4 Comparison of the AL between the two groups before and after treatment Unit: mm
Note: AL=Axial length; compared with the same group before treatment, 1) P<0.05.
Group n Before treatment After 1 month of treatment After 2 months of treatment Test 38 23.60±0.11 23.63±0.11 23.64±0.11 Control 38 23.34±0.12 23.36±0.121)23.38±0.121)
4 Discussion
AM is also known as spastic AM[5].External interventions to relieve spasticity and maintain good dynamic accommodation are still needed in most patients, except for those with a mild degree.Currently,the main clinical methods used to improve AM include drug therapy and behavioral intervention, but there are certain side effects[6]and adverse reactions[7], so it is still necessary to find a durable, reliable, and safe prevention and treatment method.
In traditional Chinese medicine (TCM), AM is similar to myopia in clinical manifestation and is called “being able to see close but fear of distance”or “Jin Qu (short sight)”[8].Acupuncture is one commonly used method for AM in TCM.It can improve patients’visual experience, delay the progression of axial myopia, and reduce the incidence of myopia, with the idea of“preventing a disease before it arises”in TCM[9].At present, there are few rigorous clinical studies on acupuncture for AM.The effect of acupuncture on AM is worth further verification and exploration.
The results of this study showed that 2-month acupuncture treatment improved the UCVA in children with AM, which was generally consistent with the results of previous studies[10].The subjects in this study were school-age children who had not developed axial myopia but only AM, and their eye vision and other aspects of imaging function were normal.After relieving excessive ciliary muscle tension and restoring normal accommodative function, the UCVA can reach a better level.In this study, there was no significant difference in the refraction between the two groups, which may be related to the observation time and the accuracy of the optometry device.In this study, an autorefractor with an accuracy of 0.25 D was used for refraction assessment, which may not detect relatively subtle diopter changes.Long-term clinical observation will be carried out in the future, and an autorefractor with higher accuracy will be used to confirm the current findings.In addition to the refraction, the AL of eyes in the two groups also showed no significant betweengroup difference after 2-month treatment, but intragroup comparison showed that the AL of eyes in the control group increased compared with that before treatment, while AL of the test group showed no increase compared with that before treatment.Previous studies showed that it was difficult to observe significant changes in the AL of eyes in the short term[11],and the AL of eyes in children of this age group is mainly related to the natural growth and the degree of myopia.Subsequentacupuncture intervention for more than 6 months will be carried out to further observe the AL of eyes.
The pathogenesis of myopia is still being explored.With the development of research, more and more researchers focus on the posterior segment of the eye.In the process of myopia development, the AL of the eye gradually increases, forcing the sclera, choroid,retina, and other tissues to stretch and extend[12], which may eventually cause permanent damage[13].The onset and development of myopia may be related to the changes in blood flow in the retina and choroid[14].In myopic children, the shallow retina in the macular area often has microcirculation disorder, which is manifested as reduced blood flow density and perfusion[15].Myopia can also damage the choroid blood circulation and reduce the thickness, which cannot meet the nutritional requirements of the retina and further lead to the morphological changes of fundus tissue[16].Some scholars have proposed that fundus microcirculation disorders in myopia patients may appear earlier than organic changes[17-18].AM is temporary myopia induced by long-term nearsightedness.Although there may not be physical lesions, the fundus microcirculation may also produce a series of reactions.
Our previous studies have shown that acupuncture can improve the retinal blood supply and delay the decreasing trend of choroidal blood flow in myopia children[19-20].In addition, previous researchers have found that acupuncture may protect retinal microcirculation in children with AM[21].The ciliary muscle is a key part involved in eye accommodation and is innervated by sympathetic and parasympathetic nerves[22], which is closely related to the occurrence and development of AM.Studies have shown that acupuncture combined with accommodation training is better than accommodation training alone in improving the UCVA of children with AM[23].Acupuncture can stimulate the autonomic nervous system, enhance tissue metabolism, activate microcirculation, affect the ciliary muscle function[24], improve the state of fundus ischemia and hypoxia, regulate the contraction and relaxation of fundus blood vessels, and regulate blood supply[25].This may be the mechanism of acupuncture in treating AM and improving UCVA.In the future, by observing the influence of acupuncture on the retina,choroid, and accommodative function, we will explore the relationship between fundus microcirculation and accommodative function and further explore the mechanism of acupuncture for AM.
This study still has some limitations, such as the short research period.The clinical design needs to be further improved to carry out in-depth research so as to provide high-quality clinical evidence for acupuncture in treating children’s AM.
Conflict of Interest
Author MA Xiaopeng is a member of the Editorial Board ofJournal of Acupuncture and Tuina Science.The paper was handled by other editors and has undergone a rigorous peer review process.Author MA Xiaopeng was not involved in the journal’s review or decisions related to this manuscript.
Acknowledgments
This work was supported by Shanghai Municipal Health Commission Research Projects of Traditional Chinese Medicine [上海市卫生健康委员会中医药科研项目,No.2020LP017, No.ZY(2021-2023)-0105-17].
Statement of Informed Consent
Informed consent was obtained from the guardians of the recruited children in this study.
Received: 31 May 2022/Accepted: 19 September 2022
猜你喜欢
杂志排行
Journal of Acupuncture and Tuina Science的其它文章
- Journal of Acupuncture and Tuina ScienceInstructions for Authors
- Editorial Members of Journal of Acupuncture and Tuina Science
- Acupuncture intervening depressive disorder:research progress in its neurobiological mechanism
- Efficacy and safety of acupuncture-moxibustion for cerebral palsy-induced speech impairment:a systematic review and meta-analysis
- Clinical observation of Tuina combined with Bu Zhong Yi Qi Tang in the treatment of rectocele
- Clinical study of treating somatoform pain disorder with the combination of electroacupuncture and duloxetine