Exploration and optimization of surgical techniques for laparoscopic transhiatal lower mediastinal lymph node dissection for adenocarcinoma of esophagogastric junction: A prospective IDEAL 2a study with qualitative design
2023-05-14YinkuiWangFanlingHongShuangxiLiFeiShanYongningJiaRulinMiaoZheminLiZiyuLiJiafuJi
Yinkui Wang ,Fanling Hong ,Shuangxi Li ,Fei Shan ,Yongning Jia ,Rulin Miao ,Zhemin Li,Ziyu Li,Jiafu Ji
1Key Laboratory of Carcinogenesis and Translational Research (Ministry of Education/Beijing),Gastrointestinal Cancer Center,Peking University Cancer Hospital &Institute,Beijing 100142,China;2Endoscopy Center,Zhongshan Hospital,Fudan University (Xiamen Branch),Xiamen 361015,China
Abstract Objective:To explore the change and feasibility of surgical techniques of laparoscopic transhiatal (TH)-lower mediastinal lymph node dissection (LMLND) for adenocarcinoma of the esophagogastric junction (AEG)according to Idea,Development,Exploration,Assessment,and Long-term follow-up (IDEAL) 2a standards.Methods:Patients diagnosed with AEG who underwent laparoscopic TH-LMLND were prospectively included from April 14,2020,to March 26,2021.Clinical and pathological information as well as surgical outcomes were quantitatively analyzed.Semistructured interviews with the surgeon after each operation were qualitatively analyzed.Results:Thirty-five patients were included.There were no cases of transition to open surgery,but three cases involved combination with transthoracic surgery.In qualitative analysis,108 items under three main themes were detected: explosion,dissection,and reconstruction.Revised instruction was subsequently designed according to the change in surgical technique and the cognitive process behind it.Three patients had anastomotic leaks postoperatively,with one classified as Clavien-Dindo IIIa.Conclusions:The surgical technique of laparoscopic TH-LMLND is stable and feasible;further IDEAL 2b research is warranted.
Keywords: Adenocarcinoma of esophagogastric junction;laparoscopic surgery;transhiatal approach;lower mediastinal lymph node dissection;IDEAL 2a research
Introduction
Previous studies have shown that the metastatic rate of lower mediastinal lymph nodes in adenocarcinoma of the esophagogastric junction (AEG) is high (1-6),with dissection required according to Japanese Gastric Cancer Treatment Guidelines (5th edition) (7).
Radical dissection and surgical safety should both be considered when designing the surgical route for AEG.According to JCOG9502 (8,9),transhiatal (TH) dissection is noninferior to left thoracoabdominal dissection with respect to overall survival for tumors with esophageal invasion less than 3 cm.Therefore,the TH approach is recommended for AEG with esophageal invasion less than 3 cm according to Japanese Gastric Cancer Treatment Guidelines (5th edition) (7).
Laparoscopic surgery for gastric cancer has been widely studied in recent years.High-quality evidence has proven the safety and noninferiority of laparoscopy to open surgery in the distal gastrectomy for both early and locally advanced gastric cancer (10-13).However,high-quality evidence is still lacking for laparoscopic total or proximal gastrectomy,which is required for AEG treatment.Although the JCOG1401,KLASS03,and CLASS02 trials have demonstrated its safety in early gastric cancer (14-16),AEG was excluded or included in only a small number of these studies.Therefore,the safety and feasibility of laparoscopic surgery for AEG treatment still need further exploration.
Laparoscopic TH lower mediastinal lymph node dissection (LMLND) is challenging in laparoscopic surgery for AEG.Indeed,due to the limited number of landmark structures,it is difficult to standardize the surgical procedures for LMLND (17).Most previous studies involved retrospective cohorts with small sample sizes,and the results showed significant heterogeneity (17-27).Similarly,the surgical techniques employed were only briefly described in the Methods section and were inconsistent among the studies,with the definition of the left and right borders being one of the most controversial steps.Costiet al.first described the procedure in 2004 and defined the left and right borders as the left and right mediastinal pleura (18).Prophylactic chest drainage has been used in cases of potential pleural injury.The incidence of pleural injury I previous studies was between 14.3% and 30.0% (19,22).Nevertheless,other studies have indicated that dissection of the left and right mediastinal pleura may allow for complete dissection of the lower mediastinal lymph nodes and adequate exposure of the surgical field,especially for proximal reconstruction(20,21,24,25,28).
The methodology for surgical innovation — the Idea,Development,Exploration,Assessment,and Long-term follow up (IDEAL) framework and recommendations —may be applied for exploration of surgical techniques for laparoscopic LMLND.The IDEAL framework and recommendation describe the development of a surgical innovation in five stages: pre-IDEAL,stage 1,the idea stage;stage 2a,the development stage;stage 2b,the exploration stage;stage 3,the assessment stage;and stage 4,evaluation in the long-term study stage (29-31).Accordingly,surgical techniques for LMLND should be at stage 2a,the development stage,and research should involve a prospective single-center study with a small sample size,aiming to present the safety and efficacy of the technique.Moreover,reporting results should focus on technique changes to determine stability and repeatability for further studies (31).
Materials and methods
Patients
From April 14,2020,to March 26,2021,patients diagnosed with AEG who underwent laparoscopic gastrectomy and LMLND with the TH approach in the First Ward,Gastrointestinal Cancer Center,Peking University Cancer Hospital,were included.The same surgeon (male) with 14 years of experience in gastrointestinal surgery,with a yearly average of 300 cases,performed all of the surgeries.
Inclusion criteria included the following: 1) diagnosis of adenocarcinoma preoperatively by endoscopy and biopsy;2) tumors located at the esophagogastric junction (EGJ)according to the Siewert criteria with invasion of the EGJ,as confirmed by preoperative endoscopy or upper gastrointestinal radiography (32,33);3) tumors at clinical stages of T2-T4a diagnosed by contrast-enhanced computed tomography (CT) scan;4) no evidence of distant metastasis according to preoperative examinations,except for positive cytological results in peritoneal lavage;and 5)informed consent.
Exclusion criteria were as follows: 1) pregnancy or breastfeeding;2) severe or uncontrolled diseases of other systems,including heart failure,renal failure,seizures,psychosis,and infectious diseases;3) history of ischemic heart disease or cerebral vascular disease within 6 months;4) organ transplants and needing immunosuppressive therapies;or 5) needing emergency surgery because of perforation,obstruction,or hemorrhage.
Elimination criteria included the following: 1) complete surgery not performed;2) withdrawal from the study;or 3)inappropriateness of continuing the study because of severe adverse events.
The study was approved by the Institutional Review Board of Peking University Cancer Hospital,and written informed consent was obtained from every patient.
Surgical procedures
A 12 mm trocar was inserted subumbilically,and a 5 mm trocar was inserted at the anterior axillary line below the right costal margin.Laparoscopic exploration was regularly performed to rule out peritoneal metastasis;peritoneal lavage was also performed routinely.A 5 mm trocar and a 12 mm trocar were inserted at the left and right midclavicular lines,respectively,slightly above the umbilical level.A 12 mm trocar was inserted at the anterior axillary line below the left costal margin.Total or proximal gastrectomy was performed according to Japanese Gastric Cancer Treatment Guidelines (5th edition) (7).LMLND was carried out;details are presented inFigure 1and video(http://www.cjcrcn.org/video/33.html).If laparoscopicassisted surgery was chosen,an upper abdominal incision was made for digestive tract reconstruction.If total laparoscopic surgery was chosen,reconstruction was performed intracorporeally,and the specimen was removed using a specimen pocket through elongation of the subumbilical trocar incision.
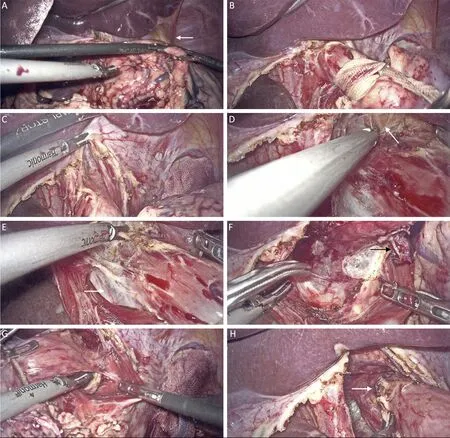
Figure 1 Surgical process of LMLND.(A) Nathanson liver retractor was adjusted.LTL (white arrow) was not divided in this case;(B)Esophagus was denudated and retracted with tape;(C) Hiatus was split;(D) Dissection of the anterior esophagus and exposure of the pericardium (white arrow);(E) Dissection of the right side of the esophagus,with exposure of the infra-cardiac bursa (white arrow);(F)Dissection of the posterior esophagus.A lymph node is exposed (white arrow);(G) Dissection of the left side of the esophagus;(H)Dissection is complete,and a lymph node is exposed (white arrow).LMLND,lower mediastinal lymph node dissection.
Data collection
Baseline information,intraoperative and postoperative information,and pathological information were collected from the electronic medical records system.One researcher performed a face-to-face semistructured interview with the surgeon after each surgery,with audio recording,in the surgeon’s office.The researcher (male) is at the same department as the surgeon,has an MD degree,and had finished residential and fellowship training in general surgery and gastrointestinal tumor surgery.The surgeon was aware of the purpose and goal of this study.The interviews included the following: 1) an overall evaluation of the difficulty level;2) changes in each procedure and the reason;3) potential risks and mistakes in each procedure;and 4) potential improvements for ensuing surgeries and the reasons.The duration of the interviews was not predetermined.Data saturation was considered when no technique changes were undertaken for at least 5 consecutive cases.After transcribing the audio records,two researchers reviewed all the records for accuracy.Then,the surgeon reviewed the records to confirm the transcription.Videos were taken during the surgeries using the recording function of the laparoscope.All the videos were reviewed to extract the following information: 1) the dissection time of the LMLND (starting with opening the diaphragm and ending with freeing the esophagus) and 2) injury to the mediastinal pleura and subsequent management.
Data analysis and qualitative methodology
Regular quantitative analysis of the data was performed using SPSS software (Version 26;IBM Corp.,NewYork,USA).
Qualitative methodology was applied for analysis of the postoperative interviews.Qualitative methodology aims to categorize information,including texts,pictures,and videos,which are difficult to analyze with calculation in quantitative methodology (34).The results are reported in line with the Consolidated Criteria for Reporting Qualitative Research (COREQ) criteria (35).
The framework approach was utilized in the current research (36) with the following steps,all of which were performed by two researchers: 1) read all of the transcriptions;2) extracted the key themes and constructed the framework;3) coded each transcription according to the framework using NVivo software (Version 12;QSR International,Burlington,USA);4) reviewed and revised all contents under each theme and subtheme;5) summarized all contents and prepared a chart of technical changes;and 6) revised technical changes (done by the surgeon) and generated optimized technical instruction.
The framework was constructed with task analysis methodology (37,38),which analyzes each task in the following two dimensions: 1) hierarchical task analysis,listing the main surgical steps;and 2) cognitive task analysis,describing the cognitive process using the naturalistic model.The latter includes the following: task(T),the specific manipulation taken;situation awareness(SA),understanding of specific surgical situations;decision making (DM),the change in plan according to different conditions;potential errors (E),avoidable or already existing risks and errors.We also analyzed the root cause(R) of E according to T,SA and DM.
Results
Clinical and pathological characteristics of included patients
Thirty-five patients were prospectively included in the current study (Figure 2,Table 1).According to preoperative examinations,most cases (74.3%) were Siewert type II and cT3 (60.0%).Twenty-seven patients (77.1%) received total gastrectomy and eight (22.9%) proximal gastrectomy.Three patients underwent combined trans-thoracic surgery.Two of these cases were because of the positive intraoperative proximal margin;the other patient had a history of esophageal injury,and the esophageal resection was extended to avoid risks of anastomotic complications.One case was transferred to open surgery because of difficulty in proximal reconstruction.The dissection time for LMLND was (18.2±6.3) min.Thirteen (38.2%)patients sustained pleural injury under the TH approach.
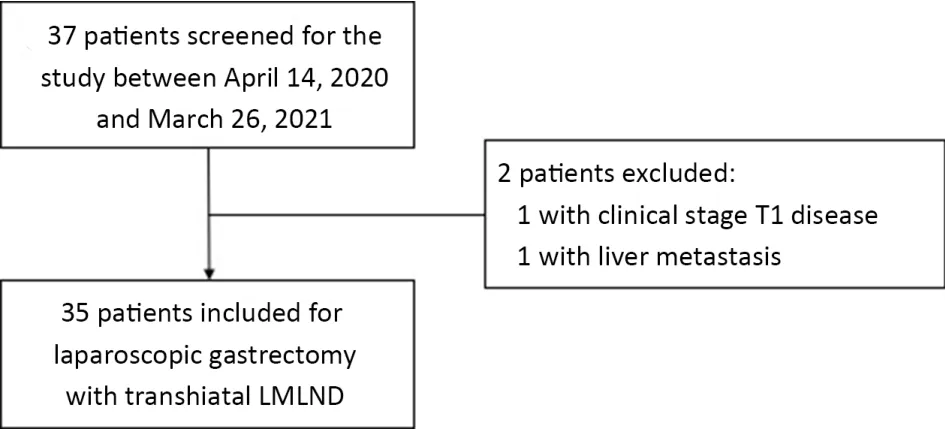
Figure 2 Flowchart of patient inclusion.LMLND,lower mediastinal lymph node dissection.
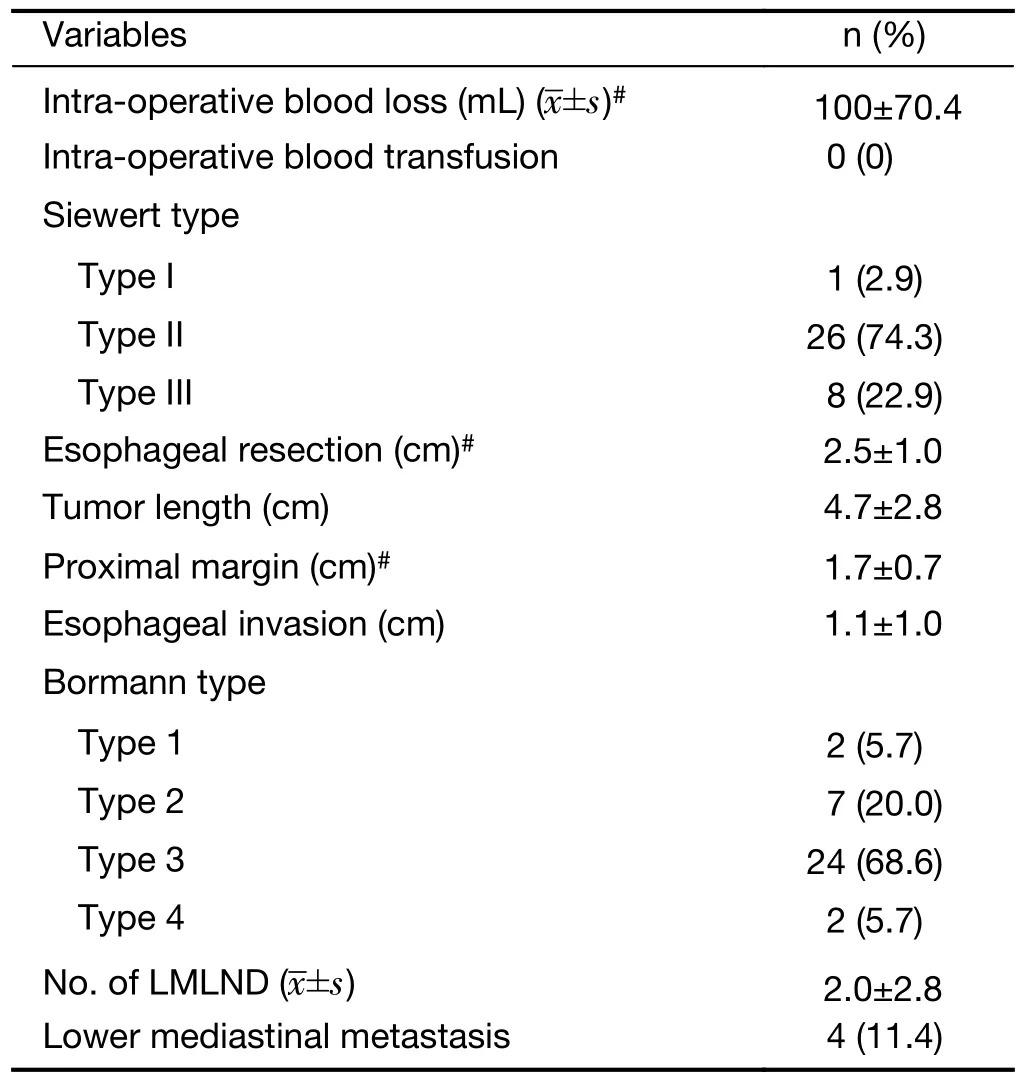
Table 1 (continued)
Framework of changes in surgical technique and optimized technical instruction
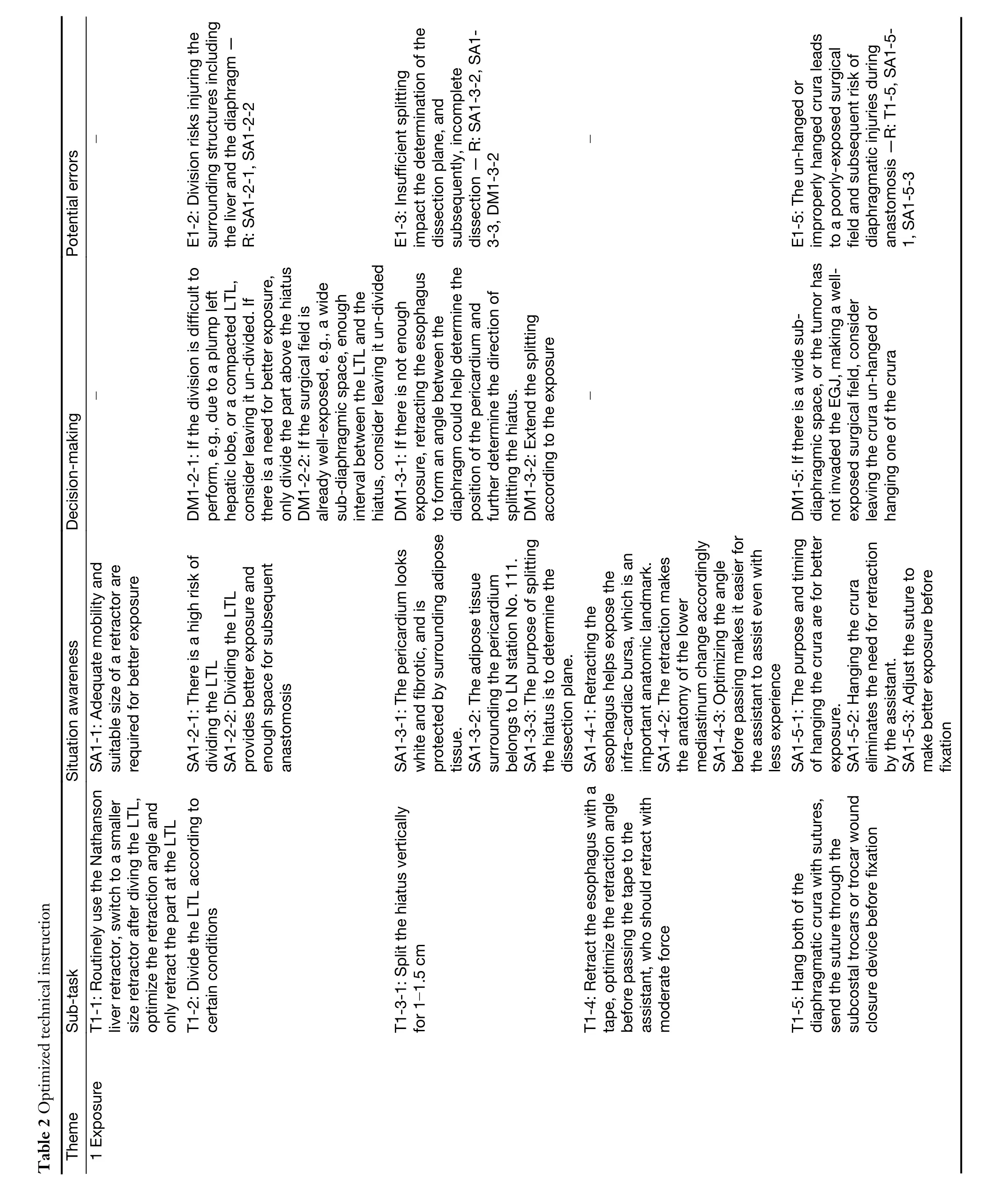
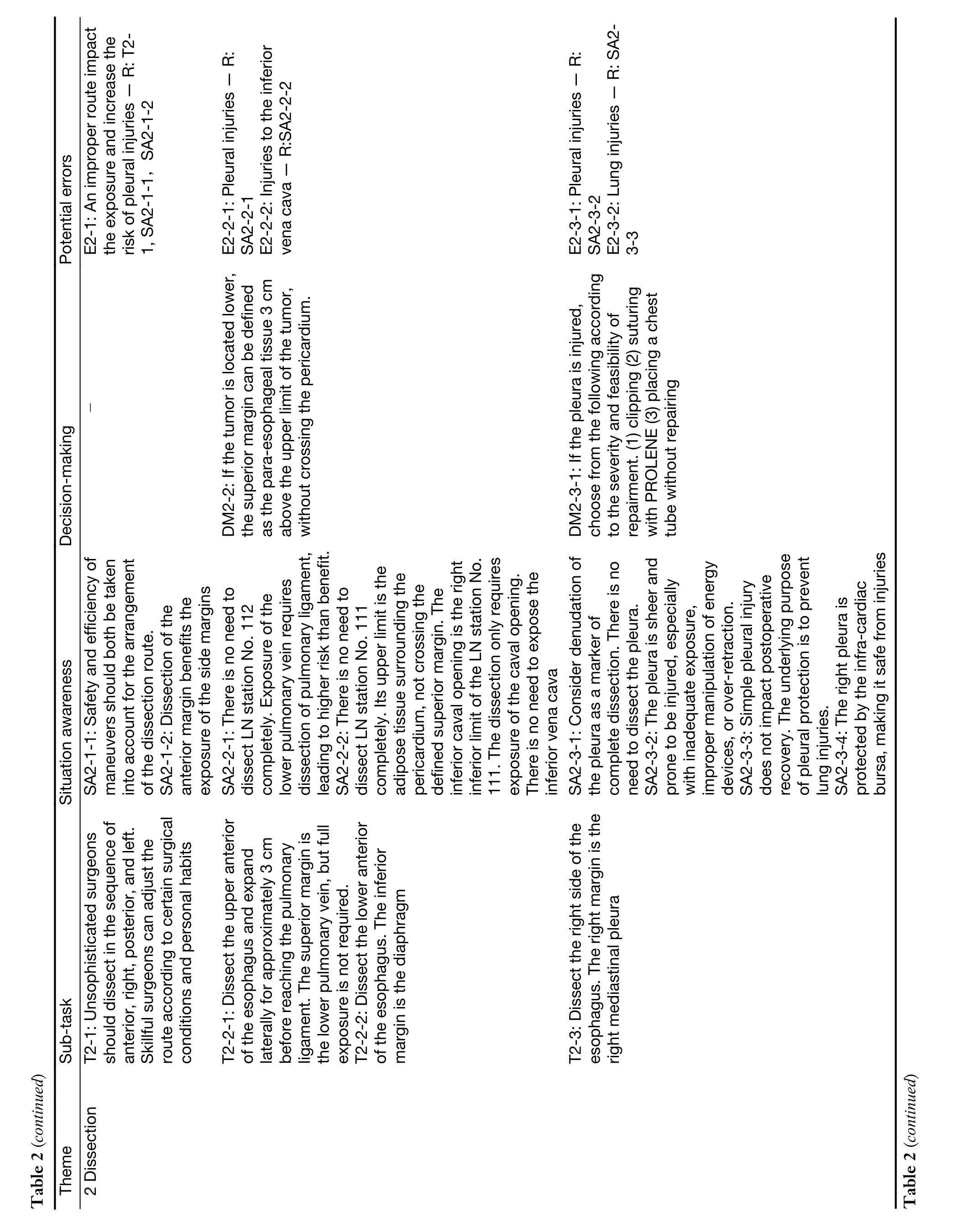
Twenty interviews were conducted after the surgery for 24 of the patients.The characteristics of each patient as well as the overall evaluation of the difficulty level are shown inSupplementary Table S1.There were three main themes in the framework according to hierarchical task analysis:exposure,dissection,and reconstruction.Five,three,and two subthemes were categorized under these three main themes.The contents under each subtheme were summarized into several points and categorized according to the naturalistic model,and points similar to those in the prior interview were deleted.Overall,there were 108 points,44 of which were under the theme “exposure”,50 under “dissection”,and 14 under “reconstruction”(Supplementary Table S2,S3).Similarly,when categorized according to cognitive task analysis,of the 108 points,38 were under “subtask”,36 under “situation-awareness”,19 under “decision-making” and 15 under “potential error”.
We derived optimized technical instruction based on the changes in technical details according to the above framework as well as descriptions in previous studies (18-26) (Table 2).For each item under “potential error”,root causes were mapped to failures in “subtask”,“situationawareness” and “decision-making”.Of the 11 potential errors raised,all of which were rooted in lacking “situation awareness”,two were rooted in the failure to complete“subtask” or correct “decision-making”.
Postoperative outcomes
Postoperative recovery and postoperative complications are shown inSupplementary Table S4,Table 3,respectively.The postoperative hospital stay was 19.0±12.0 d.The incidence of postoperative complications was 60.0%.The incidence of anastomotic leakage was 8.6%,and one case (2.9%) was classified as Clavien-Dindo (CD) IIIa.There was one case of anastomotic stenosis (2.9%),which was classified as CD I.There was no perioperative death or reoperation.Postoperative complications are reported in detail for each case inSupplementary Table S5.
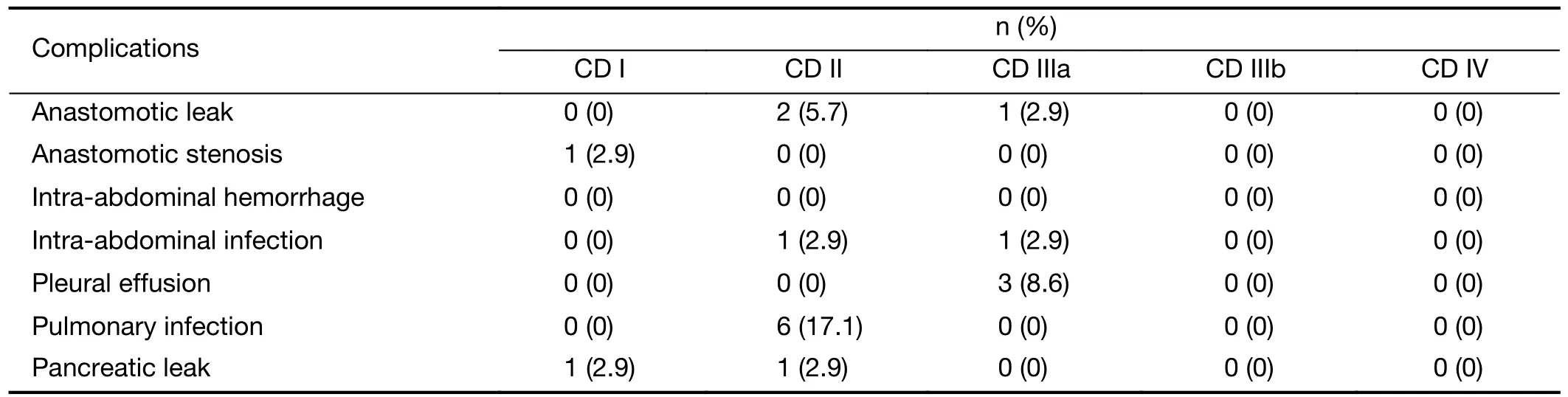
Table 3 Postoperative complications and CD classification
Discussion
There is a consensus regarding the necessity of LMLND for AEG (39,40),though a technical standard of surgical procedures is lacking.According to the IDEAL framework and recommendations,research regarding laparoscopic LMLND under the TH approach is at stage 2a,the development stage.However,previous studies on LMLND have only reported surgical outcomes of small cohorts and briefly described the techniques applied in the Methods section,without presenting technique changes (17,19-21,24,25).The current study reports technique changes of LMLND following the standard of IDEAL 2a (41) and is the first IDEAL 2a study on laparoscopic LMLND under the TH approach.
Qualitative methodology was applied for analysis of postoperative interviews.The framework constructed by the task analysis approach presents changes in technical details.Moreover,the cognitive process is shown in the framework,including the interpretation and decisionmaking of certain surgical conditions and potential errors and risks.Because there is yet no technical standard for laparoscopic LMLND,the optimized technical instruction derived from the framework may help inexperienced surgeons to better understand the what and why of the surgical process.Training and evaluation programs based on this instruction may also be the foundation of a further multicenter IDEAL 2b study.The current study,to our knowledge,is the first IDEAL 2a study using/qualitative methodology to report technique changes in a particular surgical process (42).
The significant changes are described and discussed below.
Sufficient exposure to the surgical field is prerequisite for a successful surgery.There were five subtasks regarding exposure in the framework,including 1) adjusting the Nathanson liver retractor;2) dividing the left triangular ligament (LTL);3) splitting the hiatus;4) retracting the esophagus;and 5) hanging the diaphragmatic crura.The surgeon adjusted these subtasks according to different anatomy and tissue conditions.Additionally,techniques to decrease the difficulty for an in-experienced assistant to help with the exposure were noted.Nevertheless,they all have the same purpose: to ensure better exposure and a sufficient operative space.
In general,dissection of the lower mediastinal lymph nodes is the most important and most disputed aspect of this surgery.The number of points under the theme“Dissection” was greater than that the other two and focused on the subtheme “The margin of the dissection”.According to Japanese Classification of Esophageal Cancer(43),the lower mediastinal lymph nodes include station 110,111,and 112,and station 112 includes 112aoA and 112pul.However,complete dissection of all lymph node stations under the TH approach may lead to potential injuries to the pleura,lung,lower pulmonary vein,and inferior vena cava.Because most AEG patients in China receive treatment from gastrointestinal surgeons,with the TH approach being widely adopted,it is reasonable to consider limited dissection to lower surgical risk.According to previous high-quality evidence,station 110 is the only lymph node station among the lower mediastinal lymph nodes that warrant dissection for AEG with esophageal invasion less than 4 cm (3,6),and its dissection does not require opening the pleura.Thus,the final instruction defined the following margin of dissection: 1) the superior margin is the lower pulmonary vein,but full exposure is not needed;2) the inferior margin is the diaphragm with exposure of the caval opening;3) the posterior margin is the aorta;and 4) the lateral margins are the left and right mediastinal pleura with a recommendation to keep close to the esophagus while dissecting the left margin.
The most vulnerable structure during LMLND was the mediastinal pleura.There were also changes in the cognitive process regarding the significance and management of its injury.Because the pleura is relatively sheer and exposure and recognition of the pleura during surgery are difficult,the surgeon quickly noted the potential risk of injury during the first few cohort cases.Additionally,due to the protection of the infra-cardiac bursa,the right pleura is less risky,as supported by the current study’s quantitative analysis (Table 1).Nevertheless,its impact on postoperative recovery and management was not determined until the last cases.The first pleural injury occurred in case No.4;with a history of esophageal injury,this patient eventually underwent trans-thoracic surgery,and the pleural injury was left without management.The second injury was in case No.8,involving clipping during surgery.Neither of these cases involved postoperative pulmonary complications.After discussion with thoracic surgeons and reviewing the literature,we believe that simple pleural injuries are not a significant factor for poor postoperative recovery.More cases of pleural injuries emerged as the surgeon became more efficient with the maneuver and less careful.Thus,the surgeon further noticed that the pleural mediastinum may serve as a marker for entering the pleural cavity,preventing further injury to the lung.Moreover,the integrity of the pleura may be a barrier to the spread of possible anastomotic leaks.Therefore,the optimized instruction recommends various choices according to the severity of injuries,including clipping,suturing,and chest tube placement without repairment if repair is not feasible.
The route of dissection is rarely mentioned in previous studies.However,it still needs consideration in actual practice.Safety and efficiency should both be taken into account when designing a procedure.In the early stages,when the maneuvers were not highly sophisticated and the significance of pleural injuries was not fully understood,safety should be placed first.Because dissection of the anterior and posterior margins favors exposure of the lateral margins and the left pleura is more prone to injury than the right,we recommended dissecting in the order of anterior,posterior,right and left.With the number of successful cases increasing,the surgeon may adjust the order according to specific surgical conditions.The only requirement is to leave the left margin in the last place.
As there were no technique changes after case 30,we considered that the procedure had reached stability and is feasible for further research according to IDEAL stages.Because the current study was in an early IDEAL stage,there would inevitably be limitations.Although implemented in as standardized a manner as possible,the qualitative method is inevitably objective,especially when the review was conducted with a single surgeon,due to the innovativeness of the technique.On the other hand,with a small number of cases,there was limited potential for quantitative research.We calculated the overall complication rate to be 60%,but it was difficult to perform comparisons due to the one-arm design.According to our previous data of laparoscopic total gastrectomy without LMLND,the complication rate is 34.7% in patients undergoing TLTG with either π-shaped or the modified overlap method using knotless barbed sutures (44).However,48.2% of the patients had tumors located in the middle-third of the stomach,clearly lower than the patients included in the current study,who had tumors in the EGJ.According to another study,patients undergoing laparoscopic gastrectomy with OrVilTMhad a complication rate of 46.7%,and 78.8% of them had AEG (45).Thus,in the current study focusing on AEG patients with an even higher tumor location on average,the higher complication rate is acceptable.Overall,the current result showed the safety of this procedure.A further IDEAL 2b study to verify this procedure in a larger number of cases with randomized clinical trials is in progress (No.NCT0444 3478) (46).
Conclusions
In the current study,there were no technique changes after case 30,showing the feasibility and stability of the procedure.An optimized technical instruction was eventually produced.Moreover,quantitative analysis showed an acceptable postoperative outcome and thus the safety of this procedure.In conclusion,the IDEAL 2a study for laparoscopic LMLND under the TH approach has reached its prospective outcome.A further IDEAL 2b study for this surgery may be performed in the future.
Acknowledgements
This study was supported by Beijing Municipal Administration of Hospitals (No.DFL20181103) and Beijing Hospitals Authority Innovation Studio of Young Staff Funding Support (No.202123).
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
杂志排行
Chinese Journal of Cancer Research的其它文章
- Adjuvant therapy for hormone receptor-positive breast cancer:Perspective from a survey on breast cancer physicians’acceptance of practice-changing data
- Aqueous-soluble components of sporoderm-removed Ganoderma lucidum spore powder promote ferroptosis in oral squamous cell carcinoma
- Variant rs8400 enhances ALKBH5 expression through disrupting miR-186 binding and promotes neuroblastoma progression
- Integrated strategies for chemotherapy cycles in nasopharyngeal carcinoma patients: Real-world data from two epidemic centers guiding decision-making
- Transforming cancer cells for long-term living with cancer:An inspiring new approach
- When immunotherapy meets liver transplantation for hepatocellular carcinoma: A bumpy but promising road
