不同BavenoⅦ标准筛查进展期慢性肝病出现高风险食管胃静脉曲张的价值分析
2023-04-29郭春梅刘红王亚丹孟明明王沧海宿慧吴静
郭春梅 刘红 王亚丹 孟明明 王沧海 宿慧 吴静
摘要:目的 評价Baveno Ⅶ标准用于筛查国内进展期慢性肝病患者出现高风险食管胃静脉曲张(HRV)的价值,并比较与Expanded Baveno Ⅶ标准的优劣。方法 纳入2016年1月—2018年12月期间首都医科大学附属北京世纪坛医院收治的进展期慢性肝病患者146例,根据胃镜检查是否存在HRV分为HRV组(n=68)和对照组(n=78)。分析患者的临床资料、肝脏硬度值(LSM)和胃镜结果,评价不同的BavenoⅦ标准对于诊断HRV的敏感度和特异度。计量资料组间比较采用Mann-Whitney U检验和McNemar检验;计数资料组间比较采用χ2检验。对预测HRV的各变量进行单因素Logistic回归分析,对单因素分析P<0.1的变量进行多因素分析。比较两种Baveno Ⅶ标准诊断HRV的敏感度和特异度。结果 入组患者中位年龄54(29~84)岁,男性占比65.8%,主要病因为HBV(n=115, 78.8%)。Logistic单因素回归分析显示,LSM、PLT计数与HRV有关(P值均<0.05);多因素分析显示,根据Baveno Ⅶ标准,LSM>20 kPa或PLT<150×109/L与HRV有关(P值均<0.05);根据Expanded Baveno Ⅶ标准,LSM>25 kPa或PLT<110×109/L与HRV有关(P值均<0.05)。LSM和PLT诊断HRV的受试者工作特征曲线下面积分别为0.797(95%CI:0.723~0.859)和0.789(95%CI:0.714~0.852)。符合与不符合Baveno Ⅶ标准患者的食管胃静脉曲张和HRV患病率比较差异有统计学意义(χ2值分别为23.14、23.14,P值均<0.001)。符合与不符合Expanded Baveno Ⅶ标准患者的食管胃静脉曲张和HRV患病率比较差异均有统计学意义(χ2值分别为43.51、25.71,P值均<0.001)。虽然Expanded Baveno Ⅶ标准可以豁免更多的胃镜检查(32.9% vs 13.7%),但BavenoⅦ标准敏感度更高(0.98 vs 0.88),NPV更高(0.95 vs 0.83),且可更好地避免漏诊HRV(1.0% vs 9.3%)。结论 Baveno Ⅶ标准更适用于筛查国内进展期肝病患者出现HRV。
关键词:Baveno Ⅶ标准; 食管和胃静脉曲张; 肝硬化
基金项目:国家自然科学基金青年科学基金项目(81900505); 中国国家铁路集团有限公司科研专项(J2021Z609)
Value of different Baveno Ⅶ-based criteria in screening for high-risk esophageal and gastric varices in advanced chronic liver disease
GUO Chunmei1, LIU Hong1, WANG Yadan1, MENG Mingming1, WANG Canghai1, SU Hui1, WU Jing1,2. (1. Department of Gastroenterology, Beijing Shijitan Hospital, Capital Medical University, Beijing 100038, China; 2. Department of Gastroenterology, Beijing Friendship Hospital, Capital Medical University, Beijing 100050, China)
Corresponding author:
WU Jing, wujing36youyi@ccmu.edu.cn (ORCID:0000-0002-8255-1953)
Abstract:
Objective To investigate the value of Baveno Ⅶ criteria versus Expanded Baveno Ⅶ criteria in screening for high-risk varices (HRV) in patients with compensated advanced chronic liver disease (cACLD). Methods A total of 146 patients with cACLD who were admitted to Beijing Shijitan Hospital, Capital Medical University, from January 2016 to December 2018 were enrolled, and according to the absence or presence of HRV based on gastroscopy, they were divided into HRV group with 68 patients and control group with 78 patients. Clinical data, liver stiffness measurement (LSM), and gastroscopy findings were analyzed, and different Baveno Ⅶ criteria were analyzed in terms of their sensitivity and specificity in the diagnosis of HRV. The Mann-Whitney U test and the McNemar test were used for comparison of continuous data between groups, and the chi-square test was used for comparison of categorical data between groups. A univariate logistic regression analysis was performed for the variables used to predict HRV, and a multivariate analysis was performed for the variables with P<0.1. The two sets of Baveno Ⅶ criteria were compared in terms of their sensitivity and specificity in the diagnosis of HRV. Results A total of 146 patients were enrolled in the study, among whom 68 (46.6%) were found to have HRV. The median age was 54 years (range 29-84 years), male patients accounted for 65.8%, and hepatitis B virus was the main etiology observed in 115 patients (78.8%). The univariate logistic regression analysis showed that LSM and platelet count (PLT) were associated with HRV (both P<0.05). The multivariate analysis showed that based on Baveno Ⅶ criteria, LSM >20 kPa or PLT <150×109/L was associated with HRV (both P<0.05), and based on Expanded Baveno Ⅶ criteria, LSM >25 kPa or PLT <110×109/L was associated with HRV (both P<0.05). LSM and PLT had an area under the ROC curve of 0.797 (95% confidence interval [CI]: 0.723-0.859) and 0.789 (95% CI: 0.714-0.852), respectively, in the diagnosis of HRV. There were significant differences in the prevalence rates of esophageal and gastric varices and HRV between the patients who met Baveno Ⅶ criteria and those who did not meet such criteria (χ2=23.14 and 23.14, both P<0.001), as well as between the patients who met Expanded Baveno Ⅶ criteria and those who did not meet such criteria (χ2=43.51 and 25.71, both P<0.001). Although a higher proportion of patients were exempted from gastroscopy based on Expanded Baveno Ⅶ criteria (32.9% vs 13.7%), Baveno Ⅶ criteria had higher sensitivity (0.98 vs 0.88) and negative predictive value (0.95 vs 0.83) and could better avoid the missed diagnosis of HRV (1.0% vs 9.3%). Conclusion Baveno Ⅶ criteria are more suitable for the screening for HRV in cACLD patients in China.
Key words:
BavenoⅦ Criteria; Esophageal and Gastric Varices; Liver Cirrhosis
Research funding:
National Natural Science Foundation of China Youth Fund (81900505); The Science and Technology Development Project of China State Railway Group (J2021Z609)
门静脉压力升高[肝静脉压力梯度(HVPG)≥10 mmHg]导致临床显著门静脉高压(clinically significant portal hypertension,CSPH)是肝硬化病程中的重要节点[1]。CSPH患者发生食管胃静脉曲张破裂出血、腹腔积液、肝性脑病等的风险明显升高,标志着患者由代偿期进入失代偿期[2]。食管胃静脉曲张是肝硬化门静脉高压的常见并发症,研究[3]表明高风险食管胃静脉曲张(high-risk varices,HRV)6周的急诊病死率高达10%~20%,主要死亡原因为食管胃静脉曲张破裂出血及其并发症,因此早期识别HRV对改善患者预后非常重要。目前,HVPG仍是诊断门静脉高压症的金标准[4]。然而,HVPG为侵入性检查,限制了其临床应用。且研究[5-6]表明,HVPG低估了非酒精性脂肪肝相关肝硬化患者的门静脉压力。胃镜是诊断食管胃静脉曲张的金标准,然而胃镜也为侵入性检查,存在一定的风险[7]。
近年来,临床医生致力于寻找门静脉高压的无创诊断工具。2015年Baveno协作组指出符合BavenoⅥ标准[肝脏硬度值(LSM)<20 kPa且PLT>150×109/L]的患者发生HRV的可能性较低,从而可避免胃镜检查。研究[8]表明其大约可避免30%的胃镜检查,而漏诊HRV的可能性为2%。随后Augustin等[9]提出Expanded BavenoⅥ标准(LSM<25 kPa且PLT>110×109/L)。Meta分析[8]显示,BavenoⅥ标准与Expanded BavenoⅥ标准在避免胃镜和减少HRV漏诊方面各有优势。2021年,Baveno协作组发布门静脉高压的新共识(BavenoⅦ共识),指出LSM>20 kPa或PLT<150×109/L的进展期慢性肝病(compensated advanced chronic liver disease,cACLD)患者,应筛查胃镜[10]。但BavenoⅦ标准是基于欧洲肝硬化疾病谱制定的诊断标准,其肝硬化病因主要是丙型肝炎和酒精性肝病,而我国肝硬化的主要病因为乙型肝炎,Baveno Ⅶ标准是否适用于我国尚需进一步验证。考虑到Meta分析[9]提示Expanded BavenoⅥ标准(即LSM<25 kPa且PLT>110×109/L)虽然可避免更多的胃镜检查,但增加漏诊HRV的风险,同时既往研究[11]表明LSM≥25 kPa在各种病因肝硬化(酒精性肝病、慢性乙型肝炎、慢性丙型肝炎、非酒精性脂肪性肝病)中是诊断CSPH的最佳临界值。因此,当把截断值设定为LSM>25 kPa或PLT<110×109/L时,诊断HRV的特异度更高,本研究将其命名为“Expanded Baveno Ⅶ标准”,并比较两种Baveno Ⅶ标准用于筛查cACLD患者出现HRV的优劣。
1 资料与方法
1.1 研究对象 纳入2016年1月—2018年12月期间首都医科大学附属北京世纪坛医院收治的cACLD患者。分析患者同一时期(间隔<3个月)的临床资料、弹性测定值(LSM)和胃镜结果。根据胃镜检查是否出现HRV,将患者分为HRV组和对照组。
纳入标准:根据Baveno Ⅶ标准,纳入LSM≥10 kPa的慢性肝病患者。排除标准:(1)出现失代偿事件(腹水和/或肝性脑病);(2)出现食管胃静脉曲张出血和/或接受食管胃静脉曲张套扎术、硬化剂或组织胶治疗;(3)孤立性胃静脉曲张;(4)服用非选择性β受体阻滞剂或抗病毒药物;(5)门静脉血栓形成;(6)经颈静脉肝内门体分流术后;(7)非肝硬化门静脉高压;(8)肝细胞癌。
1.2 方法
1.2.1 LSM测量 由1~2名经过培训的医师进行测量。患者取仰卧位,右臂置于头部并充分暴露肋間隙,检测区域为右侧腋前线至腋中线间的第7~9肋间隙,使用FibroScan(法国巴黎Echosens)“M”探头进行检测。检测过程中探头需垂直于皮肤表面,所有患者均检测10次,取中位数为最终检查结果并要求四分位数间距小于30%,成功率≥60%,以保证结果可靠。
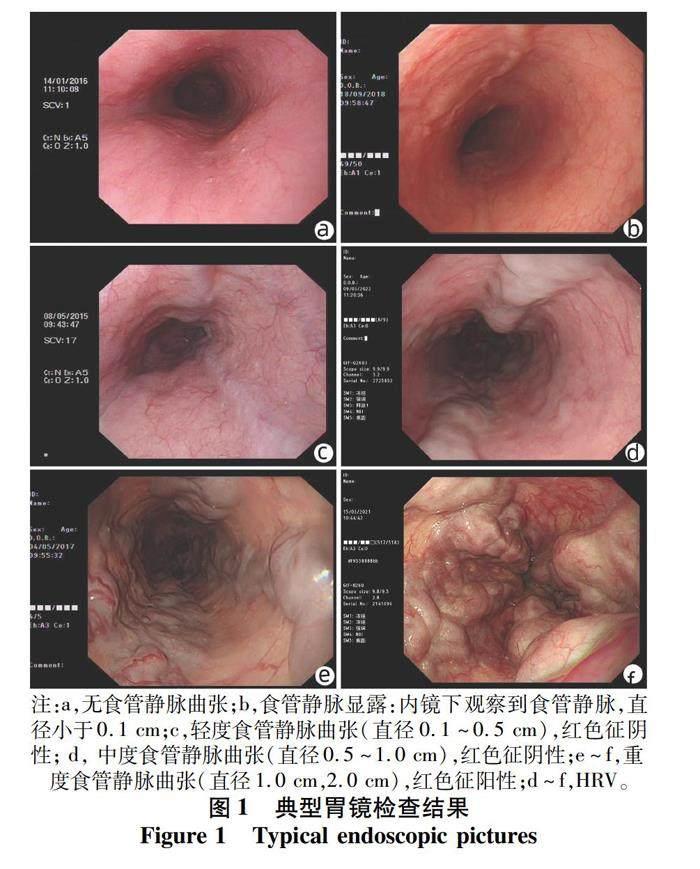
1.2.2 胃镜检查 由2名具备5年以上操作经验的内镜医生完成胃镜检查。胃镜检查记录包括:食管胃静脉曲张出现的部位、直径和红色征。检查结果由同一名具备15年以上操作经验的胃镜医师完成胃镜统一阅片,判读有无食管胃静脉曲张,并根据LDRf 分型标准[12]评估食管胃静脉曲张的风险程度,结合国内外指南[6,12],将D0.5以上或Rf1,2的静脉曲张定义为HRV(图1)。
1.3 统计学方法 采用SPSS 20.0和MedCalc软件进行统计学分析。计量资料采用M(P25~P75)表示,组间比较采用Mann-Whitney U检验和McNemar检验;计数资料组间比较采用χ2检验。对预测HRV的各变量进行单因素Logistic回归分析,对单因素分析P<0.1的变量进行多因素分析。对多因素分析有意义的变量,绘制其预测HRV的受试者工作特征曲线(ROC曲线)。比较两种Baveno Ⅶ标准诊断HRV的敏感度和特异度。P<0.05为差异有统计学意义。
2 结果
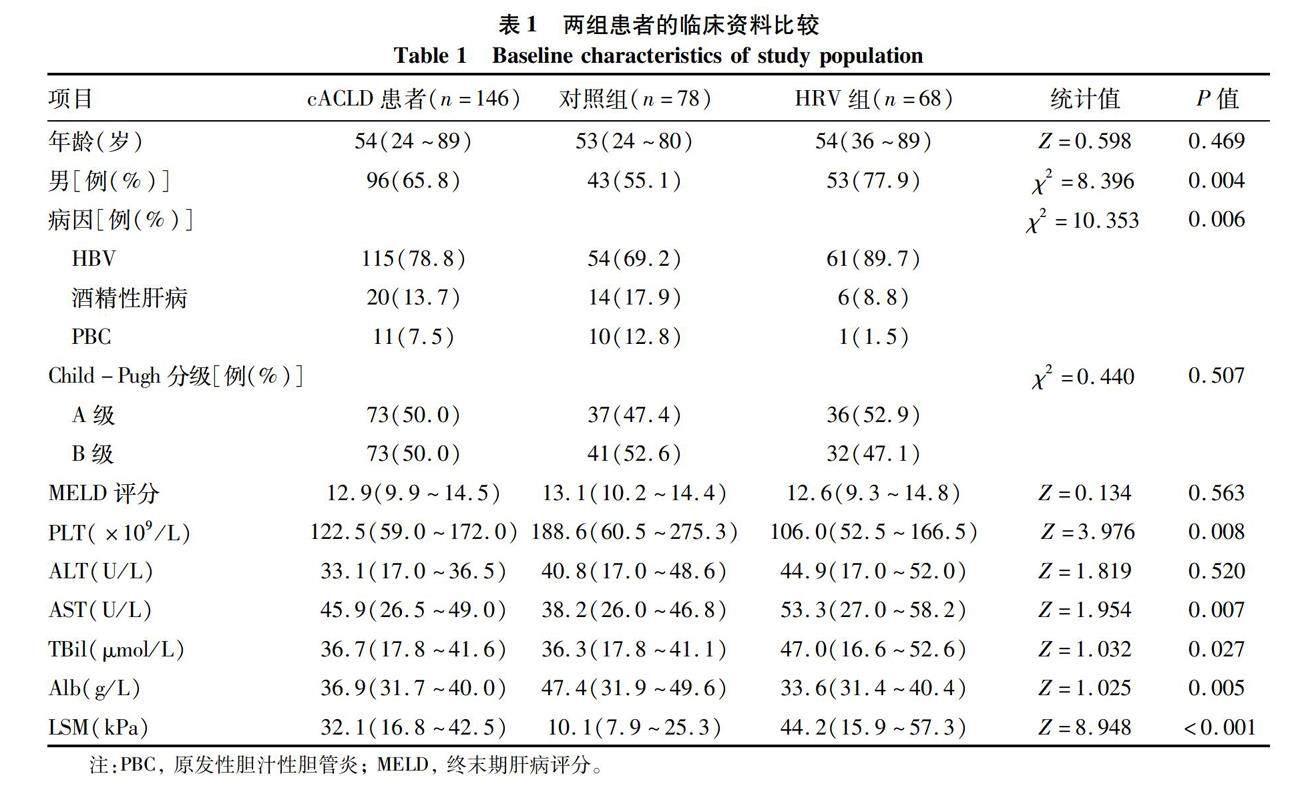
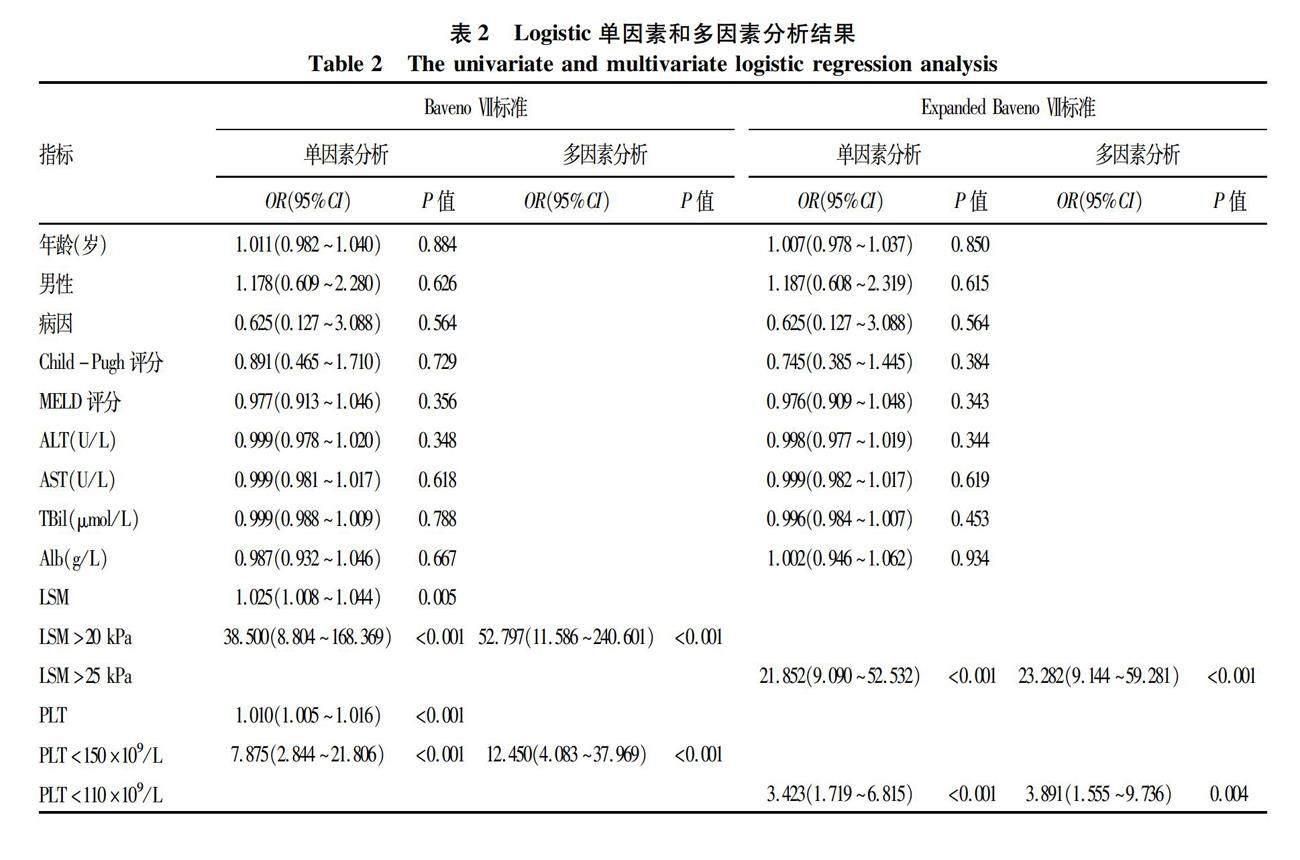
2.1 一般资料 共245例cACLD患者符合纳入标准,最终146例患者被纳入本研究(图2),HRV组68例,对照组78例。与对照组相比,HRV组患者男性、HBV的比例更高,AST和TBil水平更高,PLT和Alb水平更低,LSM更高(P值均<0.05)(表1)。2.2 HRV相关危险因素分析 Logistic单因素回归分析显示,LSM、PLT计数与HRV有关(表2)。多因素分析显示,根据Baveno Ⅶ标准,LSM>20kPa或
2.3 两种BavenoⅦ标准对于cACLD患者出现食管胃静脉曲张或HRV的诊断价值 符合与不符合Baveno Ⅶ标准患者的食管胃静脉曲张和HRV患病率比较差异有统计学意义(χ2值分别为23.14、23.14,P值均<0.001)。符合与不符合Expanded Baveno Ⅶ标准患者的食管胃静脉曲张和HRV患病率比较差异均有统计学意义(χ2值分别为43.51、25.71,P值均<0.001)(表3)。虽然Expanded Baveno Ⅶ标准可以豁免更多的胃镜检查(32.9% vs 13.7%),但BavenoⅦ标准敏感度更高(0.98 vs 0.88), NPV更高(0.95 vs 0.83),且可更好地避免漏诊HRV(1.0% vs 9.3%)(表4)。
2.4 两种BavenoⅦ标准对于各病因cACLD患者的诊断价值 在cACLD患者中,符合BavenoⅦ标准的HBV感染者或酒精性肝病患者中不存在HRV漏诊,PBC患者有1例HRV漏诊。按照Expanded BavenoⅦ标准,三类患者均存在HRV漏诊。对于HBV感染者、酒精性肝病和PBC患者,BavenoⅦ标准的NPV均高于Expanded Baveno Ⅶ标准(表5)。
3 讨论
门静脉高压是慢性肝病发生发展过程中广泛存在的一组临床综合征,其较高的发病率和较差的临床结局(食管胃静脉曲张破裂出血、腹水、肝性脑病等)在全球范围内造成了严重的公共卫生问题[1-2,13-15]。食管胃静脉曲张(尤其是HRV)破裂出血是门静脉高压症的严重并发症,病死率为12%~22%[16]。最新的指南[7,17-19]建议将LSM>20~25 kPa(禁食状态至少检测2次)作为无创评估门静脉高压和食管胃静脉曲张的重要手段[20]。此外,加拿大、瑞士和美国的研究人员也提出了一些诊断CSPH的非侵入性模型[21-22]。然而,这些模型尚未在中国人群中进行验证。既往有研究[23]表明,基于瑞士肝癌人群的CT相关HVPG评分并不适用于中国患者。这主要是由于中国肝硬化患者中HBV和PBC占相当大的比例,而欧美的肝硬化病因主要是HCV和酒精性肝病。
近几年临床采用Baveno Ⅵ标准和Expanded Baveno Ⅵ标准[22-26]以豁免胃镜检查。但是,每种标准都有其自身的优缺点[22-23,26]。Meta分析[27](共纳入30项研究,8 469例患者)显示,Baveno Ⅵ标准用于排除cACLD患者发生HRV具有较高的诊断准确性(敏感度0.97,特异度0.32,AUC 0.90)。然而,其他研究[22]认为,与Baveno Ⅵ标准相比,Expanded Baveno Ⅵ标准可能进一步豁免胃镜检查。Giannini等[28]研究表明,Expanded Baveno Ⅵ标准在诊断HCV感染者食管胃静脉曲张的实用性(准确性和豁免胃镜检查)和安全性(需要治疗的静脉曲张)之间提供了最佳平衡。在上述前提下,Baveno研讨会于2021年10月提出了一种无创工具(Baveno Ⅶ标准),用于未使用非选择性β受体阻滞剂治疗的cACLD患者的内镜筛查[19]。
Baveno Ⅶ標准提出用LSM和PLT计数预测食管胃静脉曲张风险[19]。LSM>20 kPa或PLT<150×109/L的患者存在需要治疗的HRV,因此需要进行胃镜筛查[19]。然而,根据Baveno Ⅶ标准,很多无高风险静脉曲张的患者仍然接受了内镜检查。因此,提出了一种基于Baveno Ⅶ的标准,命名为“Expanded Baveno Ⅶ标准”以确定与Baveno Ⅶ标准相比,其是否可以豁免更多的内镜检查,同时降低漏诊HRV的风险。
本研究在国内患者中评价了Baveno Ⅶ标准和Expanded BavenoⅦ标准,发现与非HRV患者相比,HRV患者中男性和HBV感染者的比例更高,且HRV患者的PLT计数和血清Alb更低,LSM、AST和胆红素更高,与既往研究[17,29]类似。同时,比较了两种BavenoⅦ标准对食管胃静脉曲张或HRV的诊断价值,发现与Baveno Ⅶ标准相比,Expanded Baveno Ⅶ标准可以豁免更多的胃镜检查(32.9%),但漏诊HRV的风险较高(9.3%)。Baveno Ⅶ标准显示出更高的敏感度(0.98 vs 0.88)和更高的NPV(0.95 vs 0.83)。考虑到实用性(豁免胃镜)和安全性(漏诊HRV)之间的平衡,Baveno Ⅶ标准可以满足临床筛查HRV的需求。
根据不同的Baveno Ⅶ标准,漏诊HRV的病因并不相同。根据Baveno Ⅶ标准,1例PBC患者漏诊HRV,而根据Expanded Baveno Ⅶ标准,8例患者(包括HBV感染者、酒精性肝病和PBC患者)漏诊了HRV。与Baveno Ⅶ标准相比,按照Expanded Baveno Ⅶ标准,HBV感染者中出现了HRV漏诊。总之,本研究显示,在HBV感染者中,Baveno Ⅶ标准用来诊断HRV更实用。
本研究存在以下不足:第一,胃镜检查和LSM测定由不同的医生进行,可能导致观察者间的差异。但本研究由经验丰富的内镜医生进行统一阅片和质控,有效减少了选择偏倚。第二,在研究队列中,一些患者存在重度胃静脉曲张,但其食管静脉曲张较轻,这可能会影响内镜医师的诊断。然而该类患者人数极少,且研究中采用统一阅片的方式进行修正,因此对结果没有产生严重影响。第三,内镜检查、PLT计数和LSM未在同一天检查。但食管胃静脉曲张、PLT计数和LSM不会在短期内发生明显变化,因此不会造成结果的重大偏差。第四, 在患者随访过程中发生破裂出血的HRV更需关注,而本研究为横断面研究,未纳入患者随访数据。因此本研究的结果还需要进一步多中心、大样本的前瞻性研究进行验证并纳入患者随访资料。
综合评估后,Baveno Ⅶ标准更适用于筛查我国cACLD患者是否存在HRV。
倫理学声明:本研究方案于2019年5月16日经由首都医科大学附属北京世纪坛医院伦理委员会审批,批号:2019年科研伦理第(41)号。
利益冲突声明:本研究不存在研究者、伦理委员会成员、受试者监护人以及与公开研究成果有关的利益冲突。
作者贡献声明:郭春梅、吴静负责课题设计,资料分析,撰写论文;王亚丹、孟明明、王沧海、宿慧参与收集数据,修改论文;刘红、吴静负责拟定写作思路,指导撰写文章并最后定稿。
参考文献:
[1]
DAMICO G, GARCIA-TSAO G, PAGLIARO L. Natural history and prognostic indicators of survival in cirrhosis: a systematic review of 118 studies[J]. J Hepatol, 2006, 44(1): 217-231. DOI: 10.1016/j.jhep.2005.10.013.
[2]FORTUNE BE, GARCIA-TSAO G, CIARLEGLIO M, et al. Child-turcotte-pugh class is best at stratifying risk in variceal hemorrhage: analysis of a us multicenter prospective study[J]. J Clin Gastroenterol, 2017, 51(5): 446-453. DOI: 10.1097/MCG.0000000000000733.
[3]SUN X, ZHANG A, ZHOU T, et al. Partial splenic embolization combined with endoscopic therapies and NSBB decreases the variceal rebleeding rate in cirrhosis patients with hypersplenism: a multicenter randomized controlled trial[J]. Hepatol Int, 2021, 15(3): 741-752. DOI: 10.1007/s12072-021-10155-0.
[4]KIM DJ, CHOI MS. Life-sustaining treatment and palliative care in patients with liver cirrhosis - legal, ethical, and practical issues[J]. Clin Mol Hepatol, 2017, 23(2): 115-122. DOI: 10.3350/cmh.2017.0018.
[5]LAU J, YU Y, TANG R, et al. Timing of endoscopy for acute upper gastrointestinal bleeding[J]. N Engl J Med, 2020, 382(14): 1299-1308. DOI: 10.1056/NEJMoa1912484.
[6]GARCIA-TSAO G, ABRALDES JG, BERZIGOTTI A, et al. Portal hypertensive bleeding in cirrhosis: Risk stratification, diagnosis, and management: 2016 practice guidance by the American Association for the study of liver diseases[J]. Hepatology, 2017, 65(1): 310-335. DOI: 10.1002/hep.28906.
[7]SUK KT. Hepatic venous pressure gradient: clinical use in chronic liver disease[J]. Clin Mol Hepatol, 2014, 20(1): 6-14. DOI: 10.3350/cmh.2014.20.1.6.
[8]STAFYLIDOU M, PASCHOS P, KATSOULA A, et al. Performance of Baveno VI and Expanded Baveno VI criteria for excluding high-risk varices in patients with chronic liver diseases: a systematic review and meta-analysis[J]. Clin Gastroenterol Hepatol, 2019, 17(9): 1744-1755. e11. DOI: 10.1016/j.cgh.2019.04.062.
[9]AUGUSTIN S, PONS M, MAURICE JB, et al. Expanding the Baveno VI criteria for the screening of varices in patients with compensated advanced chronic liver disease[J]. Hepatology, 2017, 66(6): 1980-1988. DOI: 10.1002/hep.29363.
[10]IRANMANESH P, VAZQUEZ O, TERRAZ S, et al. Accurate computed tomography-based portal pressure assessment in patients with hepatocellular carcinoma[J]. J Hepatol, 2014, 60(5): 969-974. DOI: 10.1016/j.jhep.2013.12.015.
[11]PONS M, AUGUSTIN S, SCHEINER B, et al. Noninvasive diagnosis of portal hypertension in patients with compensated advanced chronic liver disease[J]. Am J Gastroenterol, 2021, 116(4): 723-732. DOI: 10.14309/ajg.0000000000000994.
[12]Chinese Society of Hepatology, Chinese Medical Association; Chinese Society of Gastroenterology, Chinese Medical Association; Chinese Society of Endoscopy, Chinese Medical Association. Guidelines for the diagnosis and treatment of esophageal and gastric variceal bleeding in cirrhotic portal hypertension[J]. J Clin Hepatol, 2016, 32(2): 203-219. DOI: 10. 3969/j.issn.1001-5256.2016.02.002.
中華医学会肝病学分会, 中华医学会消化病学分会, 中华医学会内镜学分会. 肝硬化门静脉高压食管胃静脉曲张出血的防治指南[J]. 临床肝胆病杂志, 2016, 32(2): 203-219. DOI: 10.3969/j.issn.1001-5256.2016.02.002.
[13]ABRALDES JG, BUREAU C, STEFANESCU H, et al. Noninvasive tools and risk of clinically significant portal hypertension and varices in compensated cirrhosis: The “Anticipate” study[J]. Hepatology, 2016, 64(6): 2173-2184. DOI: 10.1002/hep.28824.
[14]QI XL. New techniques for diagnosis and monitoring of portal hypertension in liver cancer (Part )[J/CD]. Chin J Exp Clin Infect Dis(Electronic Edition), 2021, 15(1): 72. DOI: 10.3877/cma.j.issn.1674-1358.2021.01.101.
祁小龙. 肝癌门静脉高压症诊断与监测新技术(上)[J/CD]. 中华实验和临床感染病杂志(电子版), 2021, 15(1): 72. DOI: 10.3877/cma.j.issn.1674-1358.2021.01.101.
[15]QI XL. New techniques for diagnosis and monitoring of portal hypertension in liver cancer (Part Ⅱ)[J/CD]. Chin J Exp Clin Infect Dis(Electronic Edition), 2021, 15(2): 144. DOI: 10.3877/cma.j.issn.1674-1358.2021.02.101
祁小龙. 肝癌门静脉高压症诊断与监测的新技术(下)[J/CD]. 中华实验和临床感染病杂志(电子版), 2021, 15(2): 144. DOI: 10.3877/cma.j.issn.1674-1358.2021.02.101
[16]
REVERTER E, TANDON P, AUGUSTIN S, et al. A MELD-based model to determine risk of mortality among patients with acute variceal bleeding[J]. Gastroenterology, 2014, 146(2): 412-419. e3. DOI: 10.1053/j.gastro.2013.10.018.
[17]European Association for Study of Liver, Asociacion Latinoamericana para el Estudio del Higado. EASL-ALEH Clinical Practice Guidelines: Non-invasive tests for evaluation of liver disease severity and prognosis[J]. J Hepatol, 2015, 63(1): 237-264. DOI: 10.1016/j.jhep.2015.04.006.
[18]PALANIYAPPAN N, COX E, BRADLEY C, et al. Non-invasive assessment of portal hypertension using quantitative magnetic resonance imaging[J]. J Hepatol, 2016, 65(6): 1131-1139. DOI: 10.1016/j.jhep.2016.07.021.
[19]de FRANCHIS R, BOSCH J, GARCIA-TSAO G, et al. Baveno VII - Renewing consensus in portal hypertension[J]. J Hepatol, 2022, 76(4): 959-974. DOI: 10.1016/j.jhep.2021.12.022.
[20]BUCK M, GARCIA-TSAO G, GROSZMANN RJ, et al. Novel inflammatory biomarkers of portal pressure in compensated cirrhosis patients[J]. Hepatology, 2014, 59(3): 1052-1059. DOI: 10.1002/hep.26755.
[21]WANG S, HUANG Y, HU W, et al. Detachable string magnetically controlled capsule endoscopy for detecting high-risk varices in compensated advanced chronic liver disease (CHESS1801): A prospective multicenter study[J]. Lancet Reg Health West Pac, 2021, 6: 100072. DOI: 10.1016/j.lanwpc.2020.100072.
[22]CHANG PE, TAN CK, CHEAH CC, et al. Validation of the Expanded Baveno-VI criteria for screening gastroscopy in asian patients with compensated advanced chronic liver disease[J]. Dig Dis Sci, 2021, 66(4): 1343-1348. DOI: 10.1007/s10620-020-06334-y.
[23]HU Y, WEN Z. Validation and comparison of non-invasive prediction models based on liver stiffness measurement to identify patients who could avoid gastroscopy[J]. Sci Rep, 2021, 11(1): 150. DOI: 10.1038/s41598-020-80136-0.
[24]DAJTI E, RAVAIOLI F, COLECCHIA A, et al. Are the Expanded Baveno VI Criteria really safe to screen compensated cirrhotic patients for high-risk varices?[J]. Dig Liver Dis, 2019, 51(3): 456-457. DOI: 10.1016/j.dld.2018.12.013.
[25]KANG Y, PARK S, KIM S, et al. Validating the BAVENO VI criteria to identify low risk biliary atresia patients without endoscopy for esophageal varix[J]. Clin Res Hepatol Gastroenterol, 2021, 45(1): 101437. DOI: 10.1016/j.clinre.2020.04.007.
[26]ZHENG KI, LIU C, LI J, et al. Validation of Baveno VI and expanded Baveno VI criteria to identify high-risk varices in patients with MAFLD-related compensated cirrhosis[J]. J Hepatol, 2020, 73(6): 1571-1573. DOI: 10.1016/j.jhep.2020.06.042.
[27]THABUT D, BUREAU C, LAYESE R, et al. Validation of Baveno VI criteria for screening and surveillance of esophageal varices in patients with compensated cirrhosis and a sustained response to antiviral therapy[J]. Gastroenterology, 2019, 156(4): 997-1009.e5. DOI: 10.1053/j.gastro.2018.11.053.
[28]GIANNINI EG, de MARIA C, CRESPI M, et al. Course of oesophageal varices and performance of noninvasive predictors following hepatitis C virus clearance in compensated advanced chronic liver disease[J]. Eur J Clin Invest, 2020, 50(5): e13231. DOI: 10.1111/eci.13231.
[29]LEE HA, KIM SU, SEO YS, et al. Prediction of the varices needing treatment with non-invasive tests in patients with compensated advanced chronic liver disease[J]. Liver Int, 2019, 39(6): 1071-1079. DOI: 10.1111/liv.14036.
收稿日期:
2022-09-13;錄用日期:2022-11-09
本文编辑:林姣
