Vascularization of intravitreal injection of Conbercept in the treatment of retinopathy of prematurity
2023-03-13*
*
Abstract
•AIM:To evaluate retinal vascularization caused by the intravitreal injection of Conbercept in the treatment of a series of retinopathy of prematurity (ROP) cases in Type Ⅰ (threshold and pre-threshold period) and aggressive ROP (A-ROP).
•METHODS:The data of 34 ROP cases (67 eyes) treated by intravitreal injection of Conbercept (IVC) in the ophthalmology department of the Xiamen Children’s Hospital from July 2017 to March 2020 were retrospectively analyzed. Reactivation,which refers to recurrence of acute phase features,occurred at any stage of the disease in the presence or absence of other diseases.
•RESULT:The average gestational age of the 34 children was 28.82±2.32wk. The average birth weight was 1155.18±398.22g. The lesion zone of 19 cases (37 eyes) was Zone Ⅰ. In 10 cases (20 eyes),the lesion was in Zone Ⅱ,and in 5 cases(10 eyes),the lesion was in the posterior Zone Ⅱ. The total effective rate of disease control in ROP children treated with once IVC was 73.1% (49/67),and the vascularization of Zone Ⅱ was completed. The patients showed variable changes in the vascularization in Zone Ⅲ. For the patients who received one treatment and did not reactivate,the average rate of Type Ⅰ vascularization of ROP was 9.11±2.49wk,and the A-ROP was 13.40±4.04wk. The rate of A-ROP vascularization in Zone Ⅱ was significantly longer compared to Type Ⅰ.
•CONCLUSION:IVC effectively completes vascularization in Zone Ⅱ.
•KEYWORDS:Conbercept;retinopathy of prematurity;vascularization
INTRODUCTION
The expert consensus from the American Journal of Pediatrics,published for the first time in 2013,proposed the use of anti-vascular endothelial growth factor (VEGF) treatments in Stage 2 and 3 retinopathy of prematurity (ROP) with additional lesions in Zones Ⅰ and Ⅱ[1].Recent studies showed that the intravitreal injection of anti-VEGF effectively treats ROP[2-5].However,compared to traditional laser treatments,the use of anti-VEGF drugs remains controversial,as they may inhibit the development of normal blood vessels during retinal vascularization.In 2017,Wuetal[6]found that the level of serum VEGF decreased for 2mo after intraocular injection of bevacizumab to prolong the process of retinal vascularization.Furthermore,Sukgen and Koçluk[7]reported that the average vascular reconstruction time in Zone Ⅱ was 45wk (41-56wk) after the operation in children with aggressive ROP (A-ROP) treated with ranibizumab.Conbercept is a new anti-VEGF drug that exhibits high efficacy and a prolonged action time.It has recently been used in the treatment of ROP.The purpose of this study is to evaluate retinal vascularization resulting from the intravitreal injection of Conbercept in the treatment of a series of ROP cases in Zones Ⅰ and Ⅱ.
METHODS
EthicalApprovalAll patients were recruited underwritten informed consent by their parents.All experiments were approved by the institutional review committee and carried out under the ethical standards of the Declaration of Helsinki (No.2020-24).
Data from 34 cases (67 eyes) of ROP treated by intravitreal injection of Conbercept (IVC) in the Department of Ophthalmology of Xiamen Children’s Hospital from July 2017 to March 2020 were retrospectively analyzed.The parents of the children were informed of the effects and possible complications of the operation before treatment.The diagnoses were performed based on the ICROP3[8]criteria,and treatment indications were based on the consensus[9]criteria.Before the examinations,the pupils were dilated with Topicamide (Mydrin-p;Santen pharm,Japan) and the retina was examined using a RetCam Ⅲ wide-angle digital retinal imaging system (Clarity Medical Devices,USA).Images were acquired,and the diagnoses were confirmed with a binocular indirect ophthalmoscope (Keeler,UK).
The operation was performed in the operating room under sterile conditions,and patients were monitored during the entire procedure.After anesthesia (combined intravenous and inhalation anesthesia,CIIA),povidone iodine (Shanghai disinfection Likang High Tech Co.,Ltd.,Ioerkang) was used to wipe the periphery of the eyes.The surface of the eye was cleaned with povidone iodine and 0.09% normal saline.The operation area was 1.5 mm from the superior temporal limbus.A local massage was performed with a sponge before the intravitreal injection of 0.25 mg/0.025 mL Conbercept (Chengdu Kanghong Biotechnology Co.,Ltd.,Langmu,China).All injections were performed by the same surgeon.After the injection,Tobramycin eye ointment was applied four times a day for 1wk to prevent postoperative infections.The anterior chamber was examined on the first day after the operation,and the fundus was examined one week after the operation.The follow-up interval was 1-2wk according to the development of the lesion until the vascularization of Zone Ⅱ was complete.The patients were reassessed every month.
RetCam was performed at each follow-up to assess the regression and reactivation of disease and the degree of peripheral vascularization.Effective treatment was defined as the reduction of retinal arteriovenous curvature,regression of disease,and vascularization of the surrounding retina.Reactivation is defined as the reactivation of any stage of the disease with or without additional disease[8].Statistical analysis was performed using SPSS 20.0 software.The qualitative indices were expressed as frequencies and percentages,and the differences between the groups were compared using a Chi-square or Fisher exact probability test.The normal distribution of the quantitative indices was expressed by the mean ± standard deviation.Differences between groups were quantified using a two independent samplet-test and a one-way variance (ANOVA).The comparison between the two groups was further analyzed using an LSDt-test.α=0.05 was set as the threshold for statistical significance.
RESULTS
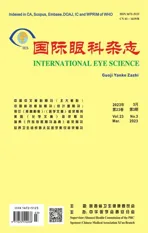
The pretreatment findings and demographic data of the 34 children (19 females and 15 males) recruited to the study are listed in Table 1.The average gestational age (GA) was 28.82±2.32wk (range 26-33wk),and the average birth weight (BW) was 1155.18±398.22g (range 780-2500)g.The lesion zone in 19 cases (37 eyes) was Zone Ⅰ,10 cases (20 eyes) in Zone Ⅱ,and 5 cases (10 eyes) in the posterior Zone Ⅱ.The average GA was 36.48±1.99wk (range 34-41).The follow-up time was 3 to 10mo after the operation.All children showed evident ridge dilution and regression within 48h-72h after treatment.No serious complications were observed after the injection.
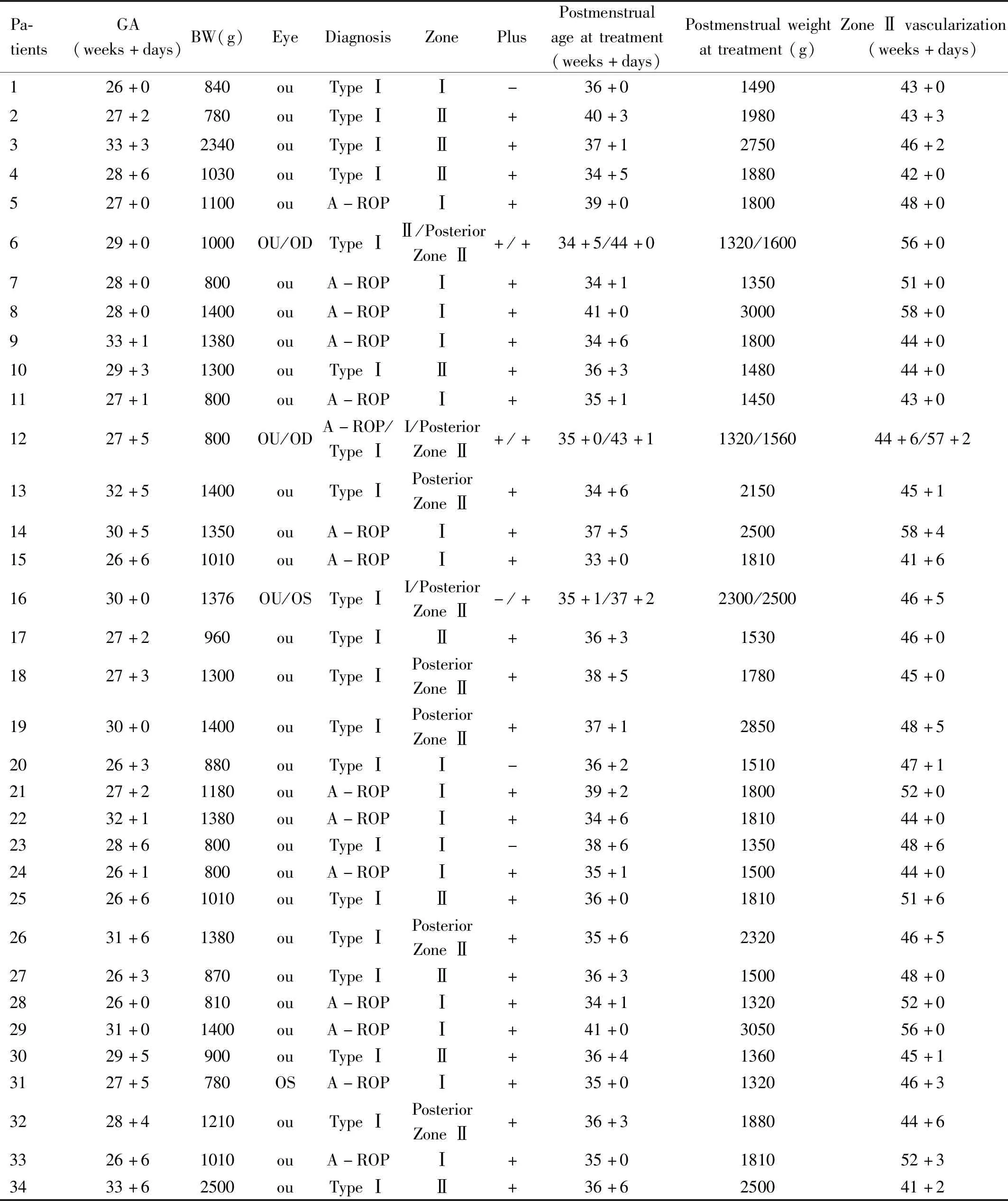
Table 1 Summary of patient demographic data and pretreatment findings
The mean corrected GA of complete vascularization of the Zone Ⅱ after treatment was 47.09±4.47 wk (range 41-58;Table 2).Fifteen cases (29 eyes) were reactivated after the first treatment,which occurred at a median of 42wk after the operation (range 40.5-44;Table 3).A total of 43.3% (29/67) cases reactivated,among which 9 cases (17 eyes) occurred in Zone Ⅰ,4 cases (8 eyes) occurred in Zone Ⅱ,and 2 cases (4 eyes) occurred in posterior Zone Ⅱ.Four cases (8 eyes) received repeated IVC treatment,and 5 cases (10 eyes) received laser treatment.Spontaneous regression of the disease was observed in 6 cases (11 eyes),and these patients were not retreated.

Table 2 Vascularization rate in Zone Ⅱ of patients who received only one treatment

Table 3 General information on reactivated cases
The average rate of vascularization in Zone Ⅱ was compared between cases that received one treatment and were not reactivated (from the GA of the first treatment to the GA of complete vascularization in Zone Ⅱ):Type Ⅰ was 9.11±2.49wk,A-ROP was 13.40±4.04wk.These two groups yielded significantly different results (P=0.001;Table 2).An LSDt-test showed that the rate of A-ROP vascularization in Zone Ⅱ was significantly longer compared to Type Ⅰ (P=0.001,0.045).
During the follow-up period,25 cases(49 eyes) degenerated and were completely vascularized (Figure 1).A total of 15 cases (29 eyes) achieved complete vascularization in Zone Ⅲ.A total of 4 cases (8 eyes) left showed white lesions in the peripheral retina (Figure 3).Only 5 cases (10 eyes) were not completely vascularized (Figure 2),among which 2 cases (4 eyes) still contained cristae.The original popcorn features disappeared,and the cristae regressed in 3 cases (6 eyes).With the exception of the 6 cases (11 eyes) that were reactivated and did not receive retreatment,the incomplete vascularization rate of Zone Ⅰ lesion group was significantly higher than that of Zone Ⅱ and the posterior Zone Ⅱ lesion group (χ2=3.419a,P<0.10;Table 4).
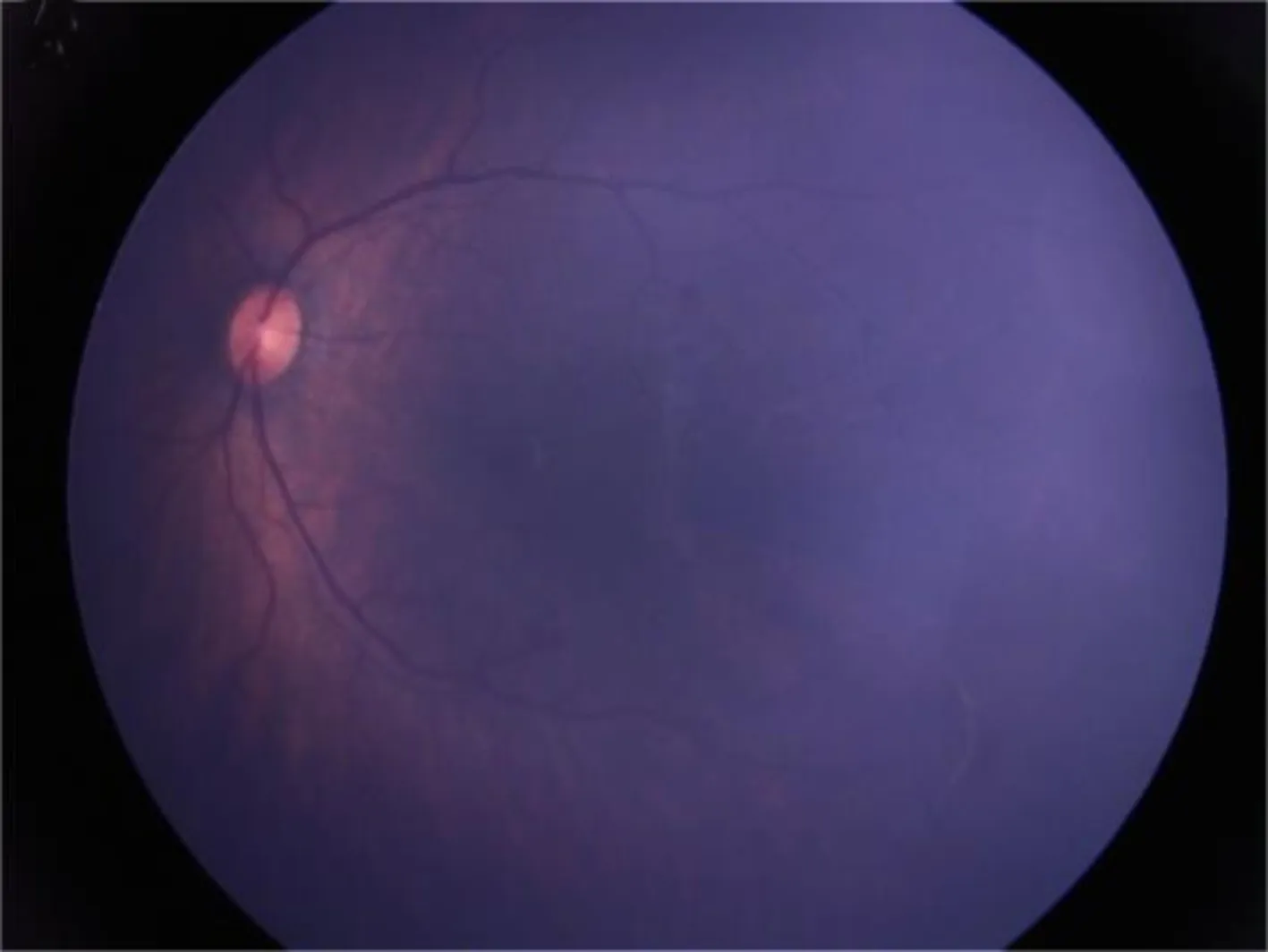
Figure 3 Retcam image of case 15. White lesions are observed in the temporal peripheral retina 6mo after IVC treatment.

Table 4 Completion of vascularization after treatment with reactivation and no retreatment
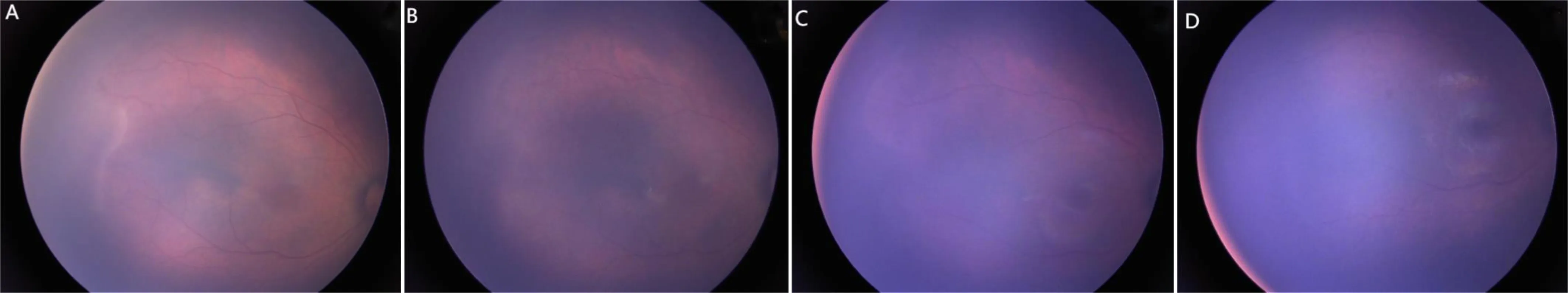
Figure 1 RetCamⅡ images of Type 1 patient (Case 13) treated with intravitreal Conbercept. A:Presence of vascularization and ridge before treatment;B:The ridge subsided 1wk after treatment;C:1mo after the operation,an increased number of terminal vascular branches and crests were observed.D:3mo after the operation,the ridge subsided,and the temporal peripheral retina was vascularized.

Figure 2 RetCam Ⅱ images of case 10 after IVC treatment. A:A partial arteriovenous short-circuit was observed in the temporal peripheral retina at 5mo after IVC treatment;B:7mo after IVC treatment,the temporal peripheral retina was not vascularized.
DISCUSSION
ROP is a proliferative retinal disease that most commonly occurs in preterm infants with low BW and small GA.More than 50,000 premature infants are diagnosed with ROP every year.Mild ROP can spontaneously resolve,however,severe cases of ROP can progress to retinal detachment,visual impairment,and ultimately lead to blindness[8].The main pathological development in ROP is vascular occlusion caused by high levels of hypoxia,which results in the release of VEGF to drive abnormal angiogenesis in the retina.The use of anti-VEGF drugs can reduce the level of neovascularization in the ridge of the retina,which is therefore an effective treatment for ROP.Conbercept is a novel anti-VEGF drug that has a high affinity for the VEGF receptor,a long half-life and a bioavailability of 44%,which partially reduces systemic adverse reactions[10].Conbercept has recently been used in the treatment of ROP,and in June 2021,the State Drug Administration issued the notice of approval for clinical trials of Conbercept with ophthalmic injection.Furthermore,Conbercept has been officially approved for clinical trials for ROP in Zones Ⅰ and Ⅱ or A-ROP in China (No.2021LP00814).
In this study,we found that the single total effective rate of the Conbercept injection in children with ROP was 73.1% (49/67) for Zone Ⅰ,Ⅱ and posterior Zone Ⅱ lesions.After injection,additional lesions subsided,and the diameter of the vessels was reduced.Previous reports reported the single treatment effectiveness of IVC at 84.2 % to 90.0%[5,11-13].Our results are slightly lower than the previously reported data.The recurrence rate after the first treatment was 26.9% (18/67 eyes),which was slightly higher than previously reported responses of 6.6% to 16.7%[12,14].These differences may be related to the lesion zone and the degree of disease.The reactivation of ROP is related to zoning and the stage of the disease.The reactivation rate of Zone Ⅰ lesions is higher than that of Zone Ⅱ lesions,and the reactivation rate of A-ROP is higher than that of Type Ⅰ lesions.Fengetal[13]reported that the degree of eye lesions significantly impacts the primary success rate.In our study,A-ROP (lesions in area Ⅰ) accounted for 32.4%,which was higher than A-ROP reported by Lietal(10.5%)[14]and Huangetal(17.1%)[4].Our study further confirmed that the single treatment efficiency of IVC was higher than intravitreal injection of Ranibizumab (IVR) (46.4%-61.0%)[4,12].
A total of 18 retreated eyes exhibited evident ridge proliferation,thickening,and distortion of the blood vessel diameters.The average recurrent GA was 5.6±0.5wk (5-7wk) after treatment,which was consistent with the reported similar half-life of Conbercept serum (20 days of serum)[15].However,the recurrence time was shorter compared to previous reports with an average of 12.9wk after injection (corrected GA of 49.0wk)[14].In our previous studies on the anti-VEGF treatment of ROP,we confirmed that GA is the main factor affecting the effect of ROP treatment[16].Hittneretal[17]reported that the risk factors of recurrence after single intravitreal injection of Bevacizumab (IVB) treatment include A-ROP,long hospital stays,and low BW.Huangetal[4]found that relapse is more frequent after IVR treatment for gestational times ≤29.5wk.Huetal[18]found that recurrence after IVR treatment of Stage 3 lesions in Zone Ⅱ was related to preretinal hemorrhage.These data indicate that the stability of the disease may be related to the severity of ROP after anti-VEGF treatment.Reactivation is likely to be more severe in Zone Ⅰ compared to Zone Ⅱ.Gestational times of ≤29.5wk and preretinal hemorrhage are also associated with recurrence.In this study,the cases of retreatment were all A-ROP children with severe conditions.Premature children with lower BW and lower GA had a higher frequency of re-treatment,which is in agreement with previous studies[16].
In the recurrent cases,8 eyes received a repeated injection of Conbercept to control the condition.The other 10 eyes received laser photocoagulation that eventually resulted in scaring of the surrounding retina.During the follow-up,ROP was controlled in 49 eyes following one treatment with IVC.Vascularization was completed in Zones Ⅱ and Ⅲ.These included 10 eyes (20.4%) without vascularization,29 eyes (59.2%) with vascularization,and 10 eyes (20.4%) with white lesions around the temporal retina.A comparison of the disease zones showed that the rate of Type 1 vascularization in Zone Ⅱ was significantly shorter than in A-ROP.Further,the completion rate of vascularization in the Zone Ⅰ group was lower than that in Zone Ⅱ and the posterior Zone Ⅱ groups.A previous study showed that the non-vascularization rate (non vascularization of the peripheral retina) in the peripheral retina varied from 3%-80% after anti-VEGF treatment in children with ROP[19].Our results show that the rate of vascularization after IVR treatment was higher than that reported by Huangetal[4].We hypothesize that this may be related to the effect of multi-targeting and high-affinity of Conbercept to the anti-VEGF receptor.The regression characteristics of ROP lesions include whitening of the neovascular tissue.The vascular abnormalities after anti-VEGF drug treatment include capillary loss and arteriovenous short circuits in the completed vascularization area[8].During follow-up,the white lesions around the retina appear similar to areas of vascular reconstruction in the surrounding avascular retina.The residual vascular fibrosis at the original ridge did not resemble recurrence.Previously,we reported that vascularization after anti-VEGF treatment is not related to the drug dose.A comparison of anti VEGF drugs (Bevacizumab,Ranibizumab,and Conbercept) in the treatment of retinopathy of preterm infants has shown that lower doses exhibit better retinal vascularization with no significant differences in the curative effects[19-23].
Complete retinal vascularization after anti-VEGF treatment can maximize retinal visual function without the reactivation of ROP caused by the overexpression of VEGF.The time of anti-VEGF treatment significantly affects the natural course of the disease.The role of anti-VEGF drugs in the inhibition of angiogenesis remains to be fully understood.Prolonging the observation period and increasing the frequency of follow-ups will contribute toward a better understanding of the impact of anti-VEGF treatments on the visual function development in children.