Predictive value of controlling nutritional status score for progression to chronic critical illness in elderly patients with sepsis
2023-03-06WANGXiaomiaoCHAIDoudouXINGBo
WANG Xiao-miao, CHAI Dou-dou, XING Bo
1. Emergency and Trauma College of Hainan Medical University, Haikou 571199, China
2. Department of Emergency, the Second Affiliated Hospital of Hainan Medical University, Haikou 570311, China
Keywords:
ABSTRACT Objective: To investigate the predictive value of controlling nutritional status (CONUT) score for progression to chronic critical illness sepsis in elderly patients, and to construct a predictive model based on CONUT score histogram.Methods: 739 elderly patients with sepsis admitted from January 2020 to December 2022 were selected as the study objects, and were divided into chronic critical illness group (n=188) and non- chronic critical illness group (n=551) according to whether chronic critical illness disease occurred.Clinical data of the patients were collected and compared.The predictive value of CONUT score, PNI and NLR in the progression of senile sepsis to chronic severe disease was compared, and the optimal threshold value was determined, which was used to convert the numerical variables into binary variables.Through univariate analysis and multivariate Logistic regression analysis, the risk factors affecting the progression of elderly sepsis patients to chronic critical illness disease were screened out,and the prediction model was built based on the nomogram.The efficacy and clinical utility of the prediction model were evaluated by the area under the ROC curve (AUC), calibration curve and decision curve analysis (DCA).Results: The best cut-off value for CONUT score in predicting elderly sepsis progressing to chronic critical illness was 4 points.The predictive performance of CONUT score (AUC=0.739) was better than that of PNI (AUC=0.609) and NLR (AUC=0.582) in elderly sepsis progressing to chronic critical illness (CONUT score vs PNI: Z=5.960, P<0.001; CONUT score vs NLR: Z=6.119, P<0.001).Univariate analysis showed that age, CCI score, SOFA score, sepsis shock, serum Lac, CONUT score, mechanical ventilation (MV), and continuous renal replacement therapy (CRRT) treatment were related to elderly sepsis progressing to chronic critical illness (P<0.05).Multivariate logistic regression analysis showed that CONUT score ≥4 points, age ≥75 years, CCI score ≥3 points, SOFA score>5 points, sepsis shock, and serum Lac ≥4 mmol/L were independent risk factors for elderly sepsis progressing to chronic critical illness (P<0.05).The nomogram showed that CONUT score had the greatest contribution value in predicting elderly sepsis progressing to chronic critical illness.Based on this, the nomogram prediction model had an AUC of 0.846 [95%CI(0.812~0.879)], with a sensitivity of 75.5% and specificity of 81.3%, indicating good predictive performance.The calibration curve was close to the ideal curve, and the DCA threshold had clinical utility advantages when ranging from 0.1 to 0.9.Conclusion: The nomographic prediction model based on CONUT score can effectively predict the risk probability of senile sepsis progressing to chronic critical illness, helpful for clinicians to identify the high risk group of chronic and severe senile sepsis, which is helpful for clinicians to identify high-risk populations of elderly sepsis with chronic critical illness.
1.Introduction
Sepsis refers to a life-threatening organ dysfunction caused by a host’s deregulated response to infection[1].In recent years, despite the effective implementation of Evidence-Based Guidelines for Sepsis resuscitation (EBGs), early acute mortality rates in sepsis patients have shown a decreasing trend, yet over 33% of sepsis survivors still experience persistent organ dysfunction of varying degrees, requiring long-term organ support therapy and progressing to Chronic Critical Illness (CCI), particularly in elderly sepsis patients[2-3].Patients with chronic critical illness not only have high mortality rates but also incur tremendous medical costs, and their quality of life significantly decreases after discharge, posing a huge burden on society, families, and individuals[4-5].Therefore, early identification of risk factors for the progression of elderly sepsis patients to chronic critical illness can help clinicians make early clinical decisions to prevent sepsis patients from progressing to chronic critical illness and improve their prognosis.Although the pathological mechanisms of sepsis progresses to chronic critical illness remain unclear, current research suggests that persistent inflammation, immunosuppression, and catabolism syndrome(PICS) may be one of the main reasons leading to chronic critical illness[6-7].Therefore, in recent years, nutritional immunological markers have become a research hotspot related to the progression of sepsis to chronic critical illness[8-9], and some studies have used the controlling nutritional status (CONUT) score to assess the short-term prognosis of elderly sepsis patients.However, there is still a lack of research on the use of the CONUT score in studying the progression of sepsis to chronic critical illness[10].Therefore, this study aims to investigate the risk factors for the progression of elderly sepsis patients to chronic critical illness and to construct an individualized predictive model for risk prediction based on the CONUT score, in order to provide effective reference for clinicians to identify highrisk patients with chronic critical illness at an early stage and take preventive measures.
2.Data and methods
2.1Research object
A retrospective study was conducted on 739 elderly patients with sepsis admitted to the ICUs of the Second Affiliated Hospital of Hainan Medical University from January 2020 to December 2022,including 536 males and 203 females, aged 65-89 years, with an average age of (73.0±5.22) years.Inclusion criteria: (1) Age ≥65 years.(2) Diagnosed with sepsis and septic shock according to the diagnostic criteria for sepsis and septic shock developed by the Third International Consensus on Sepsis-3.0[11].(3) Complete clinical data.Exclusion criteria: (1) Sepsis combined with severe comorbid diseases with a life expectancy of <3 months (such as patients with malignant tumors with a poor short-term prognosis and those receiving chemotherapy or radiotherapy within 30 days prior to sepsis).(2) Patients with immunodeficiency syndrome, autoimmune diseases, or organ transplantation status requiring long-term use of corticosteroids and immunosuppressants.(3) Patients with severe head trauma and spinal cord injury, acute coronary syndrome or cardiac arrest resuscitation; (4) Patients with sepsis who cannot be controlled due to an uncontrollable infection source (such as patients with refractory shock caused by unresectable ischemic bowel necrosis expected to die within 24 h).All patients were divided into the chronic critical illness group and the non-chronic critical illness group based on whether they developed into chronic critical illness.The diagnostic criteria for chronic critical illness included an ICU hospitalization time 14 and persistent organ dysfunction with a Sequential Organ Failure Assessment (SOFA) score 2 points[12].This study was approved by the ethics committee of the Second Affiliated Hospital of Hainan Medical University (approval number:LW2023153).
2.2 Research method
Retrospective collection of patients’ clinical data upon admission from the electronic medical record system: (1) Basic characteristics,including age, gender, body mass index (BMI), SOFA score at admission, Charlson comorbidity index (CCI) score, infection site, whether sepsis shock occurred, whether continuous renal replacement therapy (CRRT) was used, and whether mechanical ventilation (MV) was applied.(2) Laboratory indicators: serum lactate (Lac), procalcitonin (PCT), serum albumin, neutrophil count,total lymphocyte count, total cholesterol, etc.(3) Calculation of prognostic nutrition index (PNI) based on laboratory indicators= serum albumin (g/L) + 5 × peripheral lymphocyte count (109/L), neutrophil / lymphocyte ratio (NLR), CONUT score reference:serum albumin concentration (g/L) 3.5 = 0 points, 30~34.9 = 2 points, 25~29.9 = 4 points, < 25 = 6 points, total cholesterol content(mg/dL) 180 = 0 points, 140~179 = 1 point, 100~139 = 2 points,< 100 = 3 points, total lymphocyte count (109/L) 1.6 = 0 points,1.2~1.5 = 1 point, 0.8~1.1 = 2 points, <0.8=3 points.
2.3 Statistical method
A Med Calc software, SPSS23.0 software, and R Studio 4.22 version were used for statistical analysis.Quantitative data with normal distribution were expressed as mean ± standard deviation(±s), and count data were expressed as frequency or percentage.The comparison between the two groups was conducted using the chi-square test.The predictive ability of CONUT score, PNI, and NLR for elderly sepsis patients progressing to chronic critical illness was evaluated by drawing graphs and calculating or referring to the best cutoff values of each index from previous studies to convert numerical variables into binary variables.Univariate analysis and multivariate Logistic regression were used to screen risk factors for elderly sepsis progressing to chronic critical illness.The“rms” package in R Studio 4.22 software was used to construct a nomogram prediction model, and internal validation of the model was conducted using bootstrap resampling.The predictive value, consistency, and clinical utility of the prediction model were evaluated by drawing ROC curves, calibration curves, and decision curves analysis (DCA).P<0.05 was considered statistically significant.
3.Results
3.1Efficacy of CONUT score, PNI and NLR in predicting progression to chronic severe disease in elderly patients with sepsis
Using CONUT score, PNI, and NLR as test variables, ROC curves were plotted with slow severe illness as the state variable.The results showed that the predictive performance of CONUT score for elderly sepsis progressing to slow severe illness was better than that of PNI and NLR, with an AUC of 0.739 [95% CI (0.705-0.770), P<0.001].When the CONUT score predictive threshold was set at 4 points,the maximum Youden index was 0.344, Z value was 11.312, and the sensitivity and specificity were 63.8% and 70.6% respectively.The AUC for PNI predicting patient progression was 0.609 [95%CI (0.573-0.644), P<0.001], with a Youden index of 0.163, Z value of 4.586, and sensitivity and specificity of 47.3% and 68.8%respectively.The AUC for NLR predicting patient progression was 0.582 [95% CI (0.545-0.618) P<0.001], with a Youden index of 0.139, Z value of 3.404, and sensitivity and specificity of 70.7%and 43.2% respectively.CONUT score vs PNI: Z=5.960, P<0.001;CONUT score vs NLR: Z=6.119, P<0.001.The numerical variables in this study were converted into binary variables by calculating or referring to the best cutoff values of each index in previous studies related to sepsis and slow severe illness.
3.2 Comparison of clinical data between chronic critical illness group and the non-chronic critical illness group
A total of 739 elderly sepsis patients were included, of whom 188 (25.44%) progressed to chronic critical illness.There were significant differences in age, CCI score, SOFA score, sepsis shock,MV, CRRT, serum Lac, and CONUT score between the chronic critical illness and non-chronic critical illness groups (P<0.05) as shown in Table 1.

Tab 1 Comparison of clinical data between chronic critical illness group and the non-chronic critical illness group

Tab 2 Multivariate logistic regression analysis of chronic critical illness in elderly patients with sepsis
3.3 Analysis of risk factors for senile sepsis progressing to chronic and severe disease
Using the development of chronic critical illness in elderly sepsis patients as the dependent variable, univariate analysis showed that the following indicators had significant differences (P<0.05): age<75 years = 0, 75 years = 1; CCI index <3 points = 0, 3 points =1; SOFA score 2-5 points = 0, 6-9 points = 1, 10 points = 2; sepsis shock: no = 0, yes = 1; serum Lac <4 mmol/L = 0, 4 mmol/L = 1;CONUT score <4 points = 0, 4 points = 1; CRRT treatment: no= 0, yes = 1; MV: no = 0, yes = 1.Multivariate logistic regression analysis showed that age 75 years, CCI score 3 points, higher SOFA score, sepsis shock, serum Lac 4 mmol/L, and CONUT score 4 points were independent risk factors for the development of chronic critical illness in elderly sepsis patients (P<0.05), as shown in Table 2.
3.4 Construction of a nomogram prediction model for predicting the risk of sepsis progression to chronic severe disease in elderly patients
A prediction model for the development of chronic critical illness in elderly sepsis patients was constructed based on independent risk factors.The length of each variable’s corresponding line segment in the nomogram represents its predictive contribution value to the development of chronic critical illness in elderly sepsis patients.The scale on each variable’s horizontal axis segment corresponds to the “Points” value at the top of the nomogram, indicating the specific value of the variable and its corresponding single-variable score.Among them, the CONUT score has the greatest predictive contribution value for the model.For a given elderly sepsis patient admitted to the hospital, the scores for six variables were read from the graph at their corresponding points on the horizontal axis, and the sum of these six variable scores was the “Total Points”.The corresponding “Risk” value was then used to predict the probability of developing chronic critical illness in elderly sepsis patients, as shown in Figure 1.

Fig 1 Nomogram model for predicting chronic critical illness in elderly patients with sepsis
3.5 Verification and evaluation of nomogram prediction model
The validation results of the model showed that the ROC curve had a sensitivity of 75.5% and a specificity of 81.3%, with an area under the curve (AUC) of 0.846 [95% CI (0.812~0.879)].This is shown in Figure 2.The calibration curve was very close to the ideal curve,indicating good agreement between the predicted results of the model and the actual clinical outcomes, as shown in Figure 3.The decision curve demonstrated that the nomogram had clinical utility advantages in predicting the risk of elderly sepsis progressing to chronic critical illness when the threshold was between 0.1 and 0.9,as shown in Figure 4.
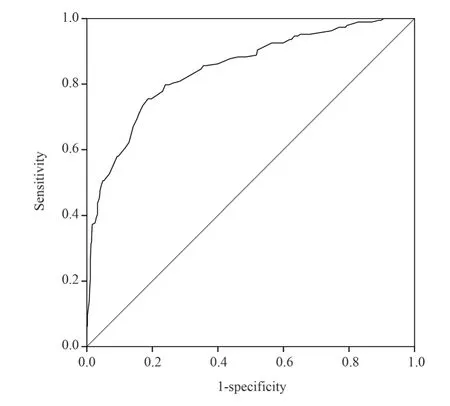
Fig 2 ROC curve of nomogram

Fig 3 Calibration curve of nomogram
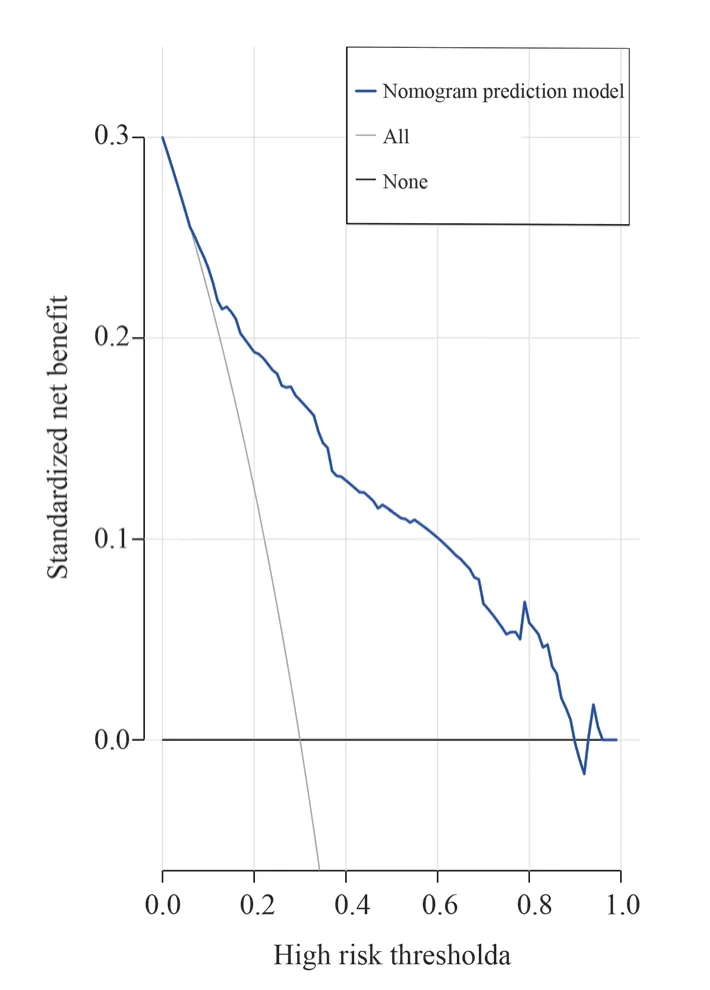
Fig 4 Decision curve analysis diagram of nomogram
4.Discussion
Sepsis is an inflammatory disease that is caused by the release of inflammatory mediators, leading to an imbalance between proinflammatory and anti-inflammatory responses.Patients who can restore normal immune regulation in the early stages can recover quickly, while those whose immune regulatory function fails to return to a stable state may develop persistent immune system disorders and abnormal catabolism, progressing to chronic critical illness.These patients mainly require long-term intensive care and continuous organ support[13].The results of this study showed that the incidence of chronic critical illness in elderly sepsis patients was 25.44% (188/739), which differed from the findings of a study on the long-term prognosis of 328 elderly sepsis patients (aged 65 years) in a surgical ICU, where the probability of developing chronic critical illness was 42%[6].One possible reason for this difference may be the different diagnostic and exclusion criteria for chronic critical illness included in this study.Chronic critical illness has become a major clinical outcome for sepsis survivors, which not only prolongs the hospital stay of sepsis patients, but also increases treatment costs, posing a serious burden on society, families, and individuals.Therefore, it is particularly important to early identify high-risk patients with elderly sepsis who are at risk of developing chronic critical illness and guide clinical interventions to prevent sepsis patients from progressing to chronic critical illness.However,there is currently no comprehensive and effective evaluation tool available.
The pathogenesis of sepsis progressing to chronic critical illness has not yet been clarified.Based on the persistent low-grade inflammation and immune suppression in sepsis survivors, PICS may be a potential pathophysiological mechanism for sepsis progressing to chronic critical illness.The CONUT score is a commonly used effective nutritional screening tool for assessing the nutritional status of cancer cachexia patients, in which serum albumin concentration serves as a protein reserve indicator, total lymphocyte count is used as an indicator of impaired immune defense, and serum total cholesterol concentration serves as a parameter for calorie consumption, involving various metabolic and immunological functions in the body[14-15].Studies have found that in the acute inflammatory response state, sepsis patients have reduced albumin levels due to various inflammatory effects.When the immune system is in a state of sustained stimulation, the nutritional status will progressively worsen and the immune system will be continuously suppressed, leading to decreased cholesterol and lymphocyte counts.Albumin, cholesterol levels, and lymphocyte counts are all related to the pro-inflammatory and anti-inflammatory responses of sepsis[16-18].Recent studies have shown that the CONUT score can be used to assess the severity and nutritional status of sepsis patients[19].Godinez-Vidal AR et al[20]showed that the CONUT score is a more reflective biochemical indicator of the nutritional status of sepsis patients in acute disease states.It is a comprehensive indicator that can reveal the patient’s immune and inflammatory status, and a high score is correlated with a poor prognosis.Therefore, the CONUT score may be an effective indicator for identifying high-risk elderly sepsis patients who are at risk of developing chronic critical illness.This study used the CONUT score to predict the risk factors for elderly sepsis patients progressing to chronic critical illness, and then conducted individualized assessments and interventions for elderly sepsis patients in order to reduce the incidence of chronic critical illness.
This study identified age 75 years, CCI score 3 points, SOFA score > 5 points, combined sepsis shock, serum Lac 4 mmol/L,and CONUT score 4 points as independent risk factors for elderly sepsis patients progressing to chronic critical illness, and they were positively correlated overall.Mankowski RTet al[6]reported that advanced age is a risk factor for elderly sepsis patients progressing to chronic critical illness, which is consistent with the findings of this study.Research has shown that although elderly sepsis patients produce pro-inflammatory responses in innate immunity and adaptive immune suppression responses in a short period of time, similar to young patients, elderly patients have a more difficult time recovering immune homeostasis.This may be due to the fact that elderly sepsis patients have more underlying diseases, higher nutritional risks,longer inflammation, immune suppression, and catabolic reactions compared to young patients, resulting in delayed recovery of immune homeostasis and longer organ function recovery times[21-22].The CCI score is calculated based on the underlying disease status, Recent studies have shown[23] that a CCI score of 3 points is an independent risk factor for elderly sepsis patients progressing to chronic critical illness.This study’s results are consistent with this finding, and the main reason may be that elderly sepsis patients with multiple underlying diseases experience more pronounced persistent inflammation, immune suppression, and catabolic syndrome due to infection, which makes it more likely for them to develop organ dysfunction and requires a longer recovery time, increasing their risk of progressing to chronic critical illness.The SOFA score evaluates organ dysfunction by a limited number of objective indicators,including respiratory, blood, liver, and circulatory organ functions.A higher SOFA score indicates more severe organ dysfunction and possible involvement of multiple organs[24-25], which can hinder rapid recovery in elderly sepsis patients and increase their risk of progressing to chronic critical illness.Previous studies have reported[26] that mechanical ventilation (MV) may be necessary for severely ill sepsis patients with organ dysfunction.Among patients with chronic critical illness, prolonged mechanical ventilation is a common reason for increased ICU stays.However, in this study,the need for MV was not an independent risk factor for elderly sepsis patients progressing to chronic critical illness.This may be due to differences in the cases included in this study; specifically,whether MV was used on admission rather than during the ICU stay.The latest diagnostic criteria for sepsis shock include serum Lac > 2 mmol/L.Septic shock patients experience organ tissue hypoperfusion, leading to tissue hypoxia and metabolic dysfunction,which explains in traditional terms why serum lactate is increased in sepsis patients.However, due to the complexity of sepsis, increased serum lactate may also be a result of inflammatory mediators[27].The results of this study showed that serum Lac 4 mmol/L is an independent risk factor for elderly sepsis patients progressing to chronic critical illness.In combination with previous studies, it has been demonstrated that elevated serum lactate levels in sepsis patients early on predict more severe tissue hypoxia and metabolic dysfunction, as well as a higher risk of developing circulatory failure and organ dysfunction due to difficulties in clearing inflammatory mediators.This increases the likelihood of progressing to chronic critical illness.A study[28]has confirmed that patients with sepsis shock are more prone to progress to chronic critical illness, which is consistent with the findings of this study.This may be due to the fact that the immune system is more severely affected when sepsis shock is present, and it may take longer for the immune system to recover once it becomes dysfunctional.The results of this study showed that the CONUT score is an independent risk factor for elderly sepsis patients progressing to chronic critical illness, and it had the greatest predictive value for the development of chronic critical illness in elderly sepsis patients in this study.This may be related to the fact that the CONUT score can comprehensively reflect the nutritional and immunological status of sepsis patients and may more easily reflect the nutritional and immunological indicators of PICS patients.PICS can regulate inflammation and immunosuppression through multiple pathways: sustained inflammatory stimuli can produce high levels of pro-inflammatory cytokines, often requiring catabolism to meet the demand, which can be manifested as increased breakdown or reduced synthesis of albumin.The final result of sustained inflammation may lead to T-lymphocyte exhaustion and a decrease in lymphocyte count.In sepsis patients, low cholesterol levels are associated with its involvement in immune regulation and antibacterial activity, and cholesterol levels are also influenced by albumin levels.Low cholesterol levels and decreased lymphocyte counts may further lead to uncontrolled inflammation and immune reactions, exacerbating organ dysfunction[29-31].Therefore, there may be a mutual influence between the levels of albumin, cholesterol,and lymphocyte count in sepsis patients, leading to their decline and predisposition to progression to chronic critical illness.
A nomogram is a prediction model based on relevant risk factors that can visualize predictions and quantify the risk of clinical events.By incorporating risk factors, clinical practitioners can use nomograms to more accurately identify high-risk patients and select treatment strategies, potentially leading to higher probability of therapeutic benefits.In this study, the ROC curve had an AUC of 0.846 [95% CI (0.812~0.879)], indicating good predictive performance and the ability to effectively identify elderly sepsis patients at high risk of developing chronic critical illness.The decision curve analysis showed that the nomogram had a net benefit for predicting elderly sepsis progression to chronic critical illness when the threshold was between 0.1 and 0.9, suggesting good clinical utility and potential advantages for clinical prediction.
This study still has some limitations: Firstly, it is a retrospective single-center study, and the predictive performance of the nomogram prediction model has not been externally validated.Secondly, the CONUT score and other indices were only determined at admission in this study.The use of statins may affect the CONUT score through dose-related effects on cholesterol, but this data was not collected in our patients.It is unclear whether the score changes over time and is influenced by medication.Therefore, in the next step, we will expand the sample size, include multi-center patients for validation,perform external validation, explore the inclusion of other potential predictive molecules and dynamic monitoring to further improve the accuracy and predictive value of the model, and further confirm this finding.
In summary, the CONUT score may better reflect the nutritional status of elderly sepsis patients compared to other nutritional immunological indicators, and it may be a useful biomarker for risk stratification and management of elderly sepsis patients progressing to chronic critical illness.In this study, a nomogram prediction model for elderly sepsis progressing to chronic critical illness was constructed based on univariate and multivariate screening of six predictive indicators, including age 75 years, CCI score 3 points, SOFA score > 5 points, sepsis shock, serum Lac 4 mmol/L, and CONUT score 4 points.The model had good predictive performance and clinical applicability, was similar to the actual accuracy, and could early identify high-risk patients for chronic critical illness, which would help clinicians take individualized clinical interventions in the early stage to prevent the transformation of elderly sepsis to chronic critical illness and improve patient outcomes.
Authors’ contributions
WANG Xiaomiao: Designed the article, collected and organized data, analyzed/interpreted data, wrote the paper.
CHAI Doudou: Conducted the research, collected data, performed statistical analysis.
XING Bo: Controlled the overall content of the article and reviewed it, guided statistical analysis, made supporting contributions.
All authors declare no conflict of interest.
杂志排行
Journal of Hainan Medical College的其它文章
- Advances in molecular mechanisms of oral submucosal fibrogenic carcinogenesis
- Research progress of ICOSL/ICOS pathway in maternal-fetal immune tolerance
- Effect and drug sensitivity analysis of PRPF18 on HCC
- Research progress of sphingosine 1-phosphate and its signal transduction in central nervous system diseases
- Meta-analysis of the effects of high-intensity intermittent exercise on cardiopulmonary function rehabilitation in patients with stroke
- SPHK1 expression in gastric cancer and clinical value based on bioinformatics analysis
