Sociopsychological impact factors of depression patients during the COVID - 19 epidemic period
2023-02-23LUOZhengjieZHANGXiaomingLIUYanruLIBinbinGUOBinLIUHuaqingWANGZhiren
LUO Zheng-jie, ZHANG Xiao-ming, LIU Yan-ru, LI Bin-bin, GUO Bin, LIU Hua-qing,WANG Zhi-ren
1. Clinical Psychology Department, Beijing Huilongguan Hospital, Beijing 100096, China
2. Technology Department, Beijing Huilongguan Hospital, Beijing 100096, China
Keywords:
ABSTRACT Objective: To investigate the impact factors of the COVID-19 epidemic on the mental health of patients with depression.Methods: The relevant data of 242 residents aged 18-50 years in a certain area were collected, 118 patients and 124 healthy people were analyzed by general information questionnaire, the PsychoSocial Index(PSI) questionnaire, Social Support Rating Scale (SSRS) and Symptom Checklist 90(SCL-90).Compare the differences in social and psychological factors between the two groups.Then use logistic regression to evaluate the social and psychological influencing factors of depression patients during the epidemic.Results: Two results of logistic regression analysis showed that marital status, occupational status, abnormal pathological behavior, and utilization of support were still significantly associated with depression.Compared to working, unemployed/unemployed/retired, students are closely related to depression, followed by abnormal pathological behavior and utilization of support.Conclusion: Under the epidemic, depression groups lacking social relationships should actively pay attention to their mental health status and comprehensively enhance their social and psychological support.To avoid the exacerbation of psychological and psychological symptoms caused by the epidemic.
1.Introduction
Recently, psychiatric symptoms caused by COVID-19 have been gradually reported, and studies have shown that SARS-CoV-2 has neurotropic properties.However, the exact mechanism by which it affects brain function has not been elucidated[1]In response to the strategy of the epidemic, the body can produce stress responses,and excessive responses will directly affect physical and mental health, causing anxiety, fear, insomnia or symptoms of physical diseases.Previous studies have shown that psychiatric symptoms,including post-traumatic stress syndrome (PTSS)/post-traumatic stress disorder (PTSD), anxiety and depression, exist in patients[2]with SARS-CoV-2 infection, and psychological factors play a key role in epidemic control and pandemic public health strategies[3].This study aims to analyze the psychological factors affecting patients with depression and healthy people during the COVID-19 epidemic, so as to understand and study the psychological state of the public during the epidemic and provide important evidence for supporting and guiding professionals and governments to provide psychological interventions[4].
2.Materials and Method
2.1Materials
The relevant data of 242 residents aged 18-50 years in a district of our city in October 2021 were collected, among which 118 cases were depressed patients as the case group, and 124 cases were healthy people as the control group.Inclusion criteria: (1) age ≥18 years old;(2) normal intelligence, good comprehension ability;(3)able to cooperate with the completion of the study;(4) no physical diseases;(5) the subjects and their families informed consent to the study and signed the informed consent form.Exclusion criteria: (1)suffering from mental retardation and severe mental diseases such as schizophrenia, personality disorder, etc.;(2) suffering from major brain diseases such as brain organic diseases, brain trauma, etc.The differences in age, education level, gender, marital status and occupational status of the two groups were compared.
2.2 Methods
General information questionnaire: including gender, age, marital status, occupational status, spouse occupational status, education level and smoking.
PsychoSocial Index (PSI) was used for clinical evaluation of the unsteady state by measuring the PSI, including 55 items, which were used to evaluate stress and related mental distress[5].The PSI has 12 sociodemographic items and clinical data and the remaining 43 items are classified into 5 factors, including stress (items 13~20 and 22~30), well-being (items 31~36), psychological stress (items 37~51), abnormal sickness behavior (items 52~54) and quality of life (item 55).
The Social Support Rating Scale (SSRS) is a self-rating scale with 10 items and an overall score of 8~44, which evaluates the degree of social support of individuals in the past year.It has 3 subscales, namely subjective support (items 1 and 3~5, scores of 4~16), objective support (items 2, 6 and 7, scores of 1~16), and the utilization of social support (items 8~10, scores of 3~12).Subjective support means that people feel the support, care and help from family, friends and colleagues.Objective support means visible,practical and direct support.The utilization of support refers to the application of social support.The higher the score of each subscale indicates the higher degree of social support, where a score <20 indicates less support, a score of 20~30 indicates general social support, and a score of 31~40 indicates satisfactory social support[6].The Symptom Checklist 90 (SCL~90) has 90 items, including a wide range of psychotic symptoms, from feelings, emotions, thinking,consciousness, behavior to living habits, interpersonal relationships,diet and sleep, etc., and uses 10 factors to reflect 10 aspects of psychological symptoms, analyzing somatization, obsessivecompulsive symptoms, interpersonal sensitivity, depression, anxiety,hostility, phobia, paranoia, psychosis, other and total scores.Each item is 1~5 points, and a score ≥160 indicates mental illness, and the higher the score, the worse the psychological state.
2.3 Statistical analysis
The study used single-sample Kolmogorov-Smirnov test and histogram to test the normal distribution of data.For normally distributed measurement data, mean ± standard deviation (±s) was used to describe, and t test was used to compare the differences between the two groups;for non-normally distributed measurement data, median (interquartile range) (M[P25, P75]) was used to describe.For classified data, percentage (%) was used to describe, and chisquare test was used to compare the differences between the two groups.In order to correct for the influence of age on psychosocial factors, the study used age as a covariate and used single factor analysis of covariance (ANCOVA) to compare the differences in psychosocial factors between the two groups.In addition, for data that did not conform to normal distribution in ANCOVA, the original data were converted by log10 and compared between groups after normality test again.In order to evaluate the influencing factors of patients with depression during the epidemic period, the study used statistically significant differences between groups as independent variables and groups as dependent variables to construct logistic regression.In logistic regression, as the dependent variable was group (depression/healthy control), and the independent variable was the factor of depression in SCL-90, there was overlap between the independent variable and the dependent variable, so the depression factor in SCL-90 was removed in logistic regression analysis.This study used SPSS 22.0 (SPSS Inc., Chicago, IL, USA) for statistical analysis, and P < 0.05 was considered statistically significant.
3.Results
3.1 Analysis of the general situation of patients with depression
A total of 118 patients with depression were included in this study as the case group, and 124 normal healthy people were included as the control group.The general situation of the two groups was compared, as shown in Table 1.The results showed that there were statistically significant differences between the two groups in age, marital status, occupational status, and smoking (P<0.05);while there was no statistically significant difference in gender and education between the two groups (P > 0.05).
3.2 Analysis of PSI survey
In PSI well-being (F = 19.396, P < 0.001) and psychological stress (F = 18.745, P < 0.001), there were statistically significant differences between the two groups, followed by abnormal pathological behavior (F = 4.193, P = 0.043) and quality of life (F= 3.908, P = 0.049).In terms of PSI stress, there was no statistically significant difference between the two groups.The results are shown in Table 2.
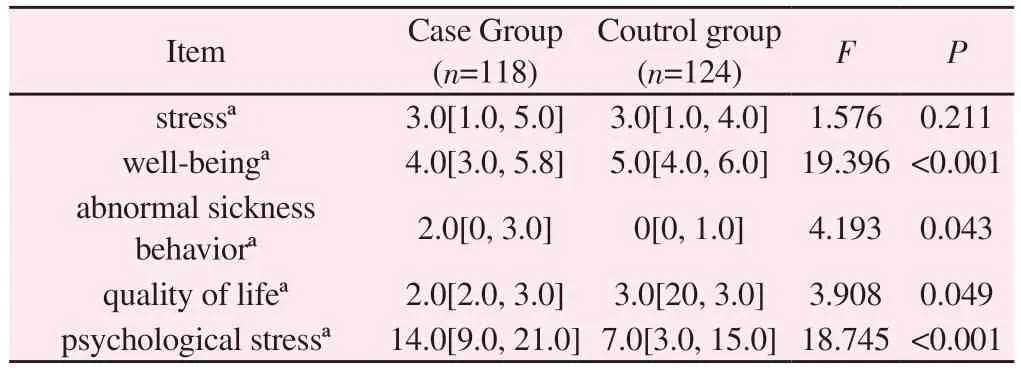
Tab 2 Results of PSI survey analysis
3.3 Analysis of SSRS questionnaire
There were statistically significant differences between patients with depression and healthy people in the total score of SSRS (F =24.475, P < 0.001), the objective support score of SSRS (F = 8.313,P = 0.004), the subjective support score of SSRS (F = 21.309, P <0.001), and the utilization of SSRS support (F = 14.964, P < 0.001)during the epidemic period (t=P<0.05), as shown in Table 3.
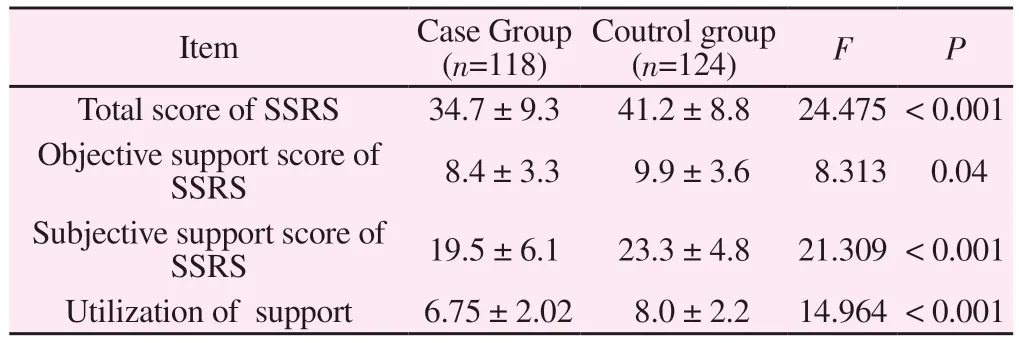
Tab 3 Results of SSRS Survey
3.4 Analysis of SCL-90 questionnaire
The differences of SCL-90 between patients with depression and healthy people during the epidemic period were compared.The results showed that compared with healthy people, the scores of somatization (F = 6.428, P = 0.012), obsessive-compulsive symptoms (F = 18.880, P < 0.001), interpersonal sensitivity (F =19.941, P < 0.001), depression (F = 32.246, P < 0.001), anxiety (F= 16.082, P < 0.001), hostility (F = 7.196, P = 0.008), phobia (F =10.213, P = 0.002), paranoia (F = 7.836, P = 0.006), psychosis (F= 20.234, P < 0.001), and others (F = 17.990, P < 0.001) in patients with depression were significantly higher, and the differences were statistically significant.The results were shown in Table 4.
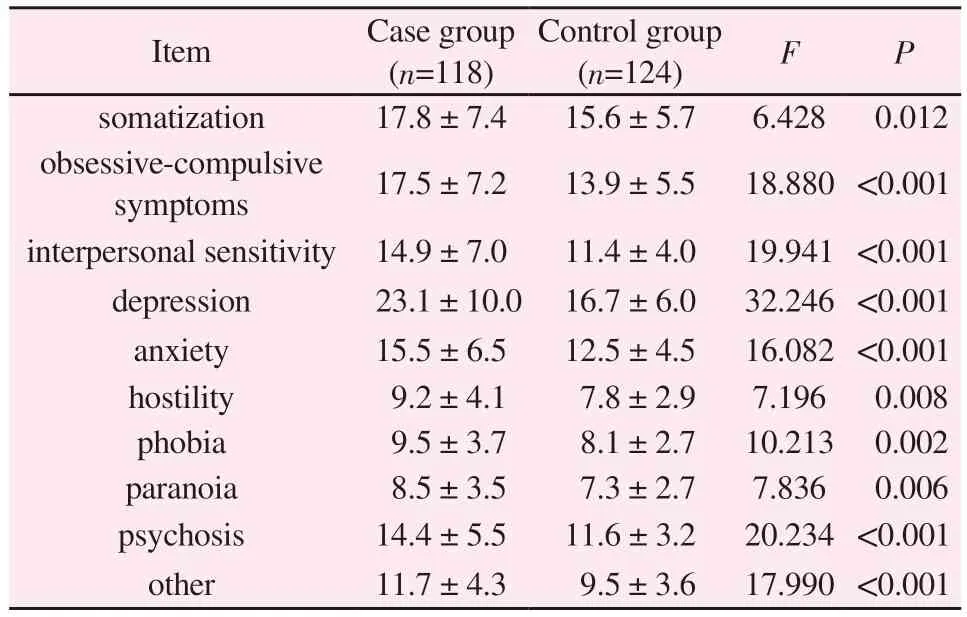
Tab 4 Analysis of SCL-90 Survey
3.5 Univariate and multivariate logistic regression analysis
In the univariate logistic regression, all the independent variables included in the analysis were significantly associated with depression.In the multivariate logistic regression, age, smoking,and all the factors of SCL-90 (except the depression factor) were no longer significantly associated with depression, while marital status,occupational status, abnormal pathological behavior, and utilization of support were still significantly associated with depression.Compared with the in-service, unemployed/retired (OR = 5.01,95%CI:1.76-15.76, P = 0.004) and students (OR = 7.25, 95%CI:2.31-24.37, P = 0.001) were closely associated with depression, followed by abnormal pathological behavior (OR = 1.37, 95%CI:1.01-1.89, P= 0.048) and utilization of support (OR = 0.82, 95%CI:0.68-1.00, P= 0.048).The results are shown in Table 5.
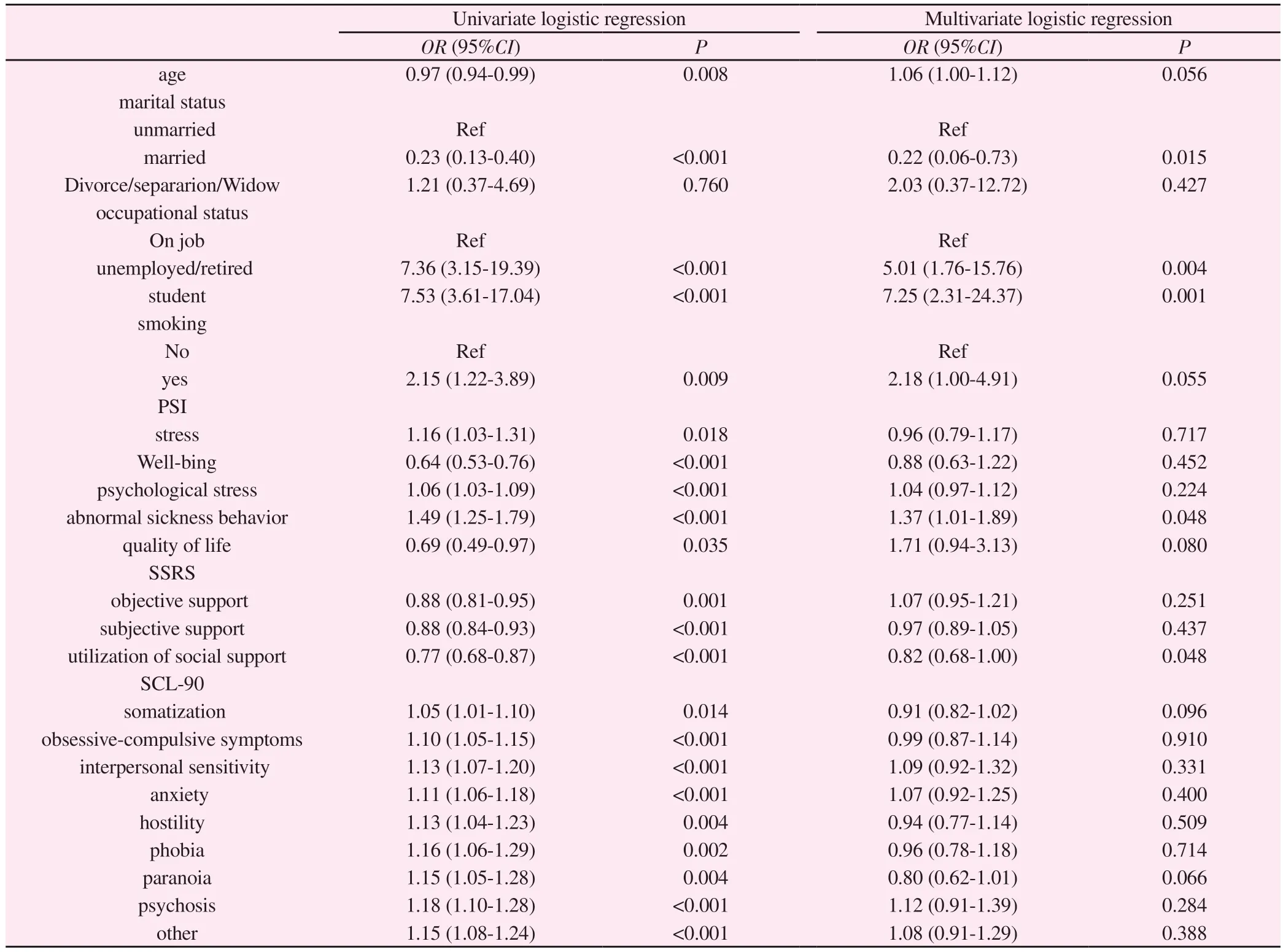
Tab 5 Univariate and multivariate analysis of influencing factors of patients with depression during the epidemic
4.Discussion
The Covid-19 not only has a serious impact on physical health,but also has a profound impact on people’s mental health and wellbeing.Although the impact of severe acute respiratory syndrome coronavirus (SARS-CoV-2) on the nervous system is still unclear,there is no doubt that the COVID-19 pandemic is harmful to mental health[7-10].In particular, the deterioration of several mental health disorders in the population of mentally ill patients will further threaten the current health care system[11].The patients with depression included in this study are themselves vulnerable to external factors, so they will be more sensitive to changes in the external environment.This study first analyzed the general situation of the included samples.The results showed that there were statistically significant differences in age, marital status, occupational status, occupational status and attraction of patients with depression,but no statistically significant differences in gender and education level.But what is the impact of COVID-19 on the risk of depression?Some studies have suggested that different groups of mentally ill patients feel anxious and depressed.Especially for people aged 18-34, women and people with children, the mental suffering is higher than expected[11].But at present, there are insufficient data in developing countries.The results suggest that patients with depression have a younger onset age, a slightly poorer ability to withstand pressure, and there are certain problems in marriage and occupational status, which will affect the condition.This study aims to understand the psychosocial factors associated with patients with depression during the epidemic.
The results showed that there were statistically significant differences between patients with depression and healthy people in PSI well-being and psychological stress, SSRS total score, SSRS objective support score, SSRS subjective support score, and SSRS utilization of support during the epidemic.Through the analysis of the SCL-90 table, it was found that compared with the healthy control group, patients with depression had statistically significant differences in obsessive-compulsive symptoms, interpersonal sensitivity, hostility, depression, paranoia, anxiety, phobia, psychosis,somatization, and others.Through logistics regression analysis, it was found that among the psychosocial factors affecting patients with depression during the epidemic, the factors with statistically significant correlations were marital status, occupational status,abnormal pathological behavior, and utilization of support; compared with in-service, unemployed/unemployed/retired, and students were closely related to depression, followed by abnormal pathological behavior and utilization of support.We consider that the relationship built in marriage and occupation is beneficial to patients with depression, which can bring support, especially during the epidemic.And such support in family work as a result of benign learning will also be beneficial to patients with depression to improve the utilization of support.We can see that the psychological support from interpersonal relationship is a very important factor, which is associated with the occurrence and recovery of many diseases.
In the future, when we encounter a large public health event again,we should pay attention to the mental health level of patients with previous depression in the current event, ensure their psychosocial support, and actively provide psychological assistance and psychological intervention, so as to avoid increasing the severity of mental illness in an adverse psychological state.In particular, we should provide psychosocial support for the only child population lacking relationships at home and at work or the students who lack social contact at home due to the epidemic.
Authors’ contribution
Luo Zhengjie: subject audit and paper writing;Wang Zhiren: quality control and paper review;Liu Yanru, Guo Bin: data collection;Zhang Xiaoming, Li Binbin: statistical analysis of data;Liu Huaqing:participated in the modification of the paper
All the authors declare that there is no conflict of interest.
杂志排行
Journal of Hainan Medical College的其它文章
- Research progress in genomics associated with prognosis of upper tract urothelial carcinoma
- A review of clinical research on using FIT screening for colorectal cancer
- Clinical efficacy of external treatment with Zi Cao Yang He Tang combined with hormone therapy for granulomatous mastitis and its effect on cellular pyroptosis proteins
- Exploring the mechanism of moist exposed burn ointment for the treatment of diabetic ulcer based on network pharmacology and molecular docking
- Clinical efficacy of leprerelin acetate with different dosage forms in central precocious puberty girls
- Pharmacodynamic study of cannabidiol on bleomycin-induced pulmonary fibrosis in rats