Posterior sub-Tenon triamcinolone acetonide injection for annular choroidal detachment resistant to systemic immunosuppressive treatment
2023-02-11DaeJoongMa
Dae Joong Ma
Department of Ophthalmology, Hallym University Kangnam Sacred Heart Hospital, Seoul 07441, Republic of Korea
Dear Editor,
I report two cases of annular choroidal detachment, which was resistant to systemic immunosuppressive treatment and presented a diagnostic dilemma but responded to posterior sub‐Tenon triamcinolone acetonide (PSTA) injections.
Annular choroidal detachment is known to occur in uveal effusion syndrome (UES)[1], Vogt‐Koyanagi‐Harada (VKH)disease[2], posterior scleritis[3], sympathetic ophthalmia[4],and tumor metastasis[5]. Inflammation serves as an important contributor to some of these conditions; therefore, systemic immunosuppressive therapy is often attempted in such cases[2]. Usually, UES shows a poor response to systemic immunosuppressive therapy and requires surgical management,including vortex vein decompression, sclerectomy, and sclerotomy[1].
The etiology underlying annular choroidal detachment remains unclear, and it is difficult to establish a definitive treatment strategy and assess the treatment response in many patients. Refractoriness to systemic immunosuppressant administration often presents a diagnostic dilemma, and it is necessary to distinguish between the possibility of insufficient immunosuppression and misdiagnosis, which may require a surgical approach, such as in patients with UES.
Ethical ApprovalThis study was approved by the Hallym University Kangnam Sacred Heart Hospital (approval number:2020‐10‐013). Written informed consent to participate and allow publication was obtained from the patients.
CASE REPORT
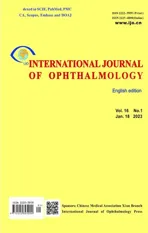
Case 1 A 48‐year‐old woman was referred for evaluation of serous retinal detachment in the right eye. She presented with a one‐week history of painless blurry vision in the right eye. Her medical and ocular histories were unremarkable. Examination showed no neurological or dermatological abnormalities. Slit‐lamp examination revealed granulomatous keratic precipitates in both eyes and trace cells in the anterior chamber and anterior vitreous in the right eye. Fundus examination revealed nearly 360° peripheral annular choroidal detachment and inferior bullous serous retinal detachment in the right eye(Figure 1A). The left eye had mild choroidal folds. Optical
coherence tomography showed subretinal and intraretinal fluid,intraretinal, subretinal, and choroidal hyper‐reflective dots in
the right eye, a wavy retinal pigment epithelium (RPE) line,and choroidal thickening in both eyes (Figure 1B). B‐scan ultrasonography revealed low reflectivity of the thickened choroid without the “T” sign in both eyes (Figure 1C). The ocular axial length was 23.4 mm in the right and 23.2 mm in the left eye. Ultrawide field (UWF) fluorescein angiography revealed diffuse discrete hypofluorescent dots involving the entire retina and a few pin‐point dye leakages from the RPE at the posterior margin of the choroidal detachment in the right eye (Figure 1D). UWF indocyanine green angiography revealed patchy choroidal hyperpermeability in the right eye and dilated choroidal veins in both eyes (Figure 1E).
She was treated with two courses of high‐dose intravenous corticosteroid (methylprednisolone 1 g/d) for 3d and followed by oral prednisolone (1 mg/kg). Thereafter, oral prednisone was reduced by 5 mg per week in combination with the initiation of immunomodulation with oral cyclosporine A 2.5 mg/kg twice daily and oral mycophenolate mofetil 1500 mg twice daily.This systemic immunosuppressive treatment was continued for 11mo, and subcutaneous adalimumab 20 mg injections every 2wk were added during the last 3mo. However, the subretinal fluid and annular choroidal detachment persisted (Figure 2A).In view of the poor response to systemic immunosuppressive treatment, UES appeared to be the probable diagnosis, and surgical treatment was planned. However, a PSTA (40 mg/1.0 mL)injection led to significant improvement (Figure 2B) in symptoms. Two additional consecutive PSTA (40 mg/1.0 mL)injections with 2 month‐interval resulted in complete resolution of the subretinal fluid and choroidal detachment (Figure 2C,2D). There was no recurrence of subretinal fluid or choroidal detachment during follow‐up for 2y.
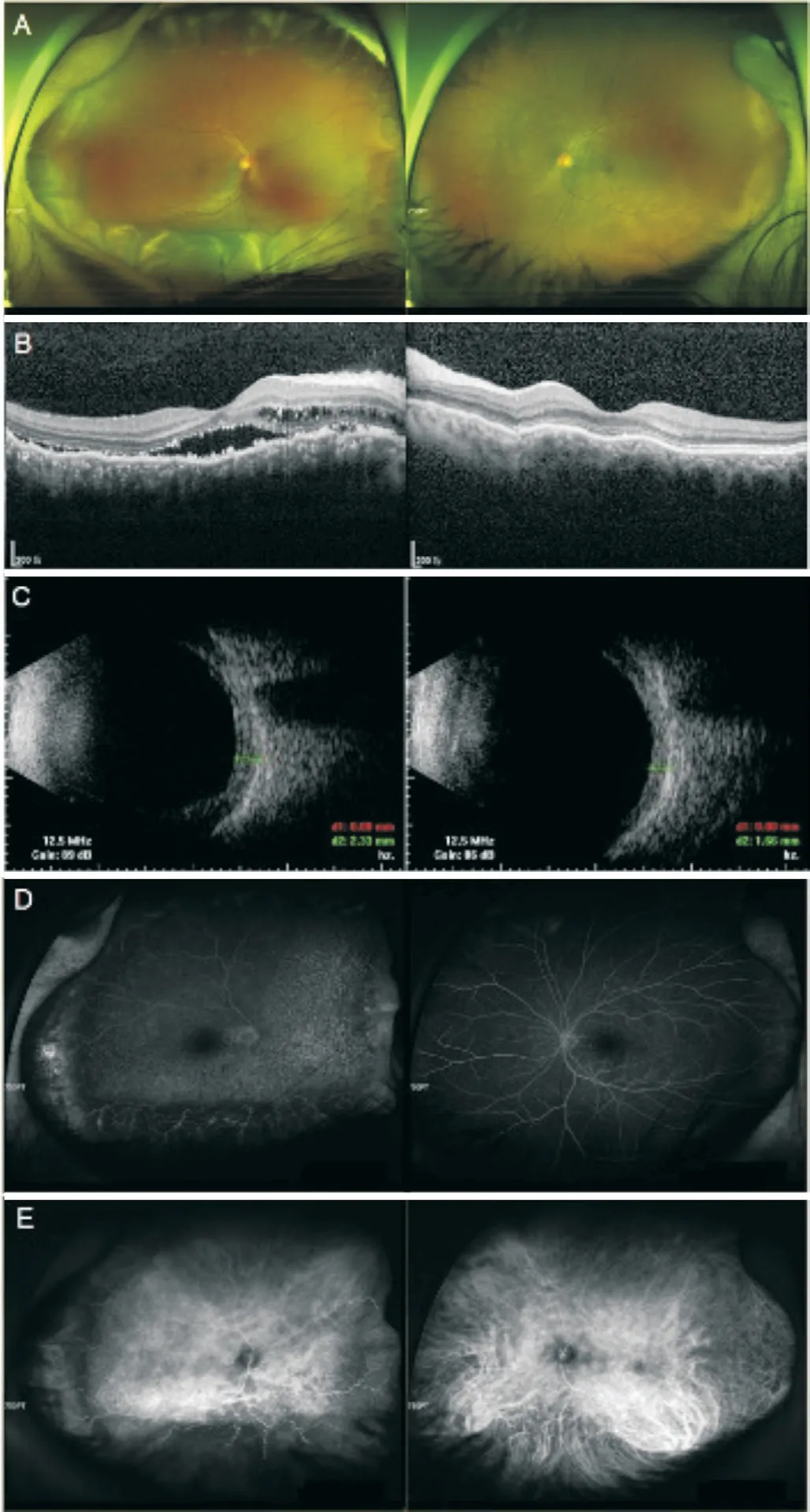
Figure 1 Images at initial visit A: Nearly 360° peripheral annular choroidal detachment with inferior bullous serous retinal detachment in the right eye and mild choroidal folds in the left eye; B: A wavy retinal pigment epithelium line with choroidal thickening in both eyes and subretinal and intraretinal fluid, intraretinal, subretinal, and choroidal hyper-reflective dots in the right eye; C: Low reflective choroidal thickening without the “T” sign in either eye; D: Diffuse hypofluorescent dots and pin-point dye leakages at the posterior margin of the choroidal detachment in the right eye; E: Dilated choroidal veins in both eyes and patchy choroidal hyperpermeability in the right eye.
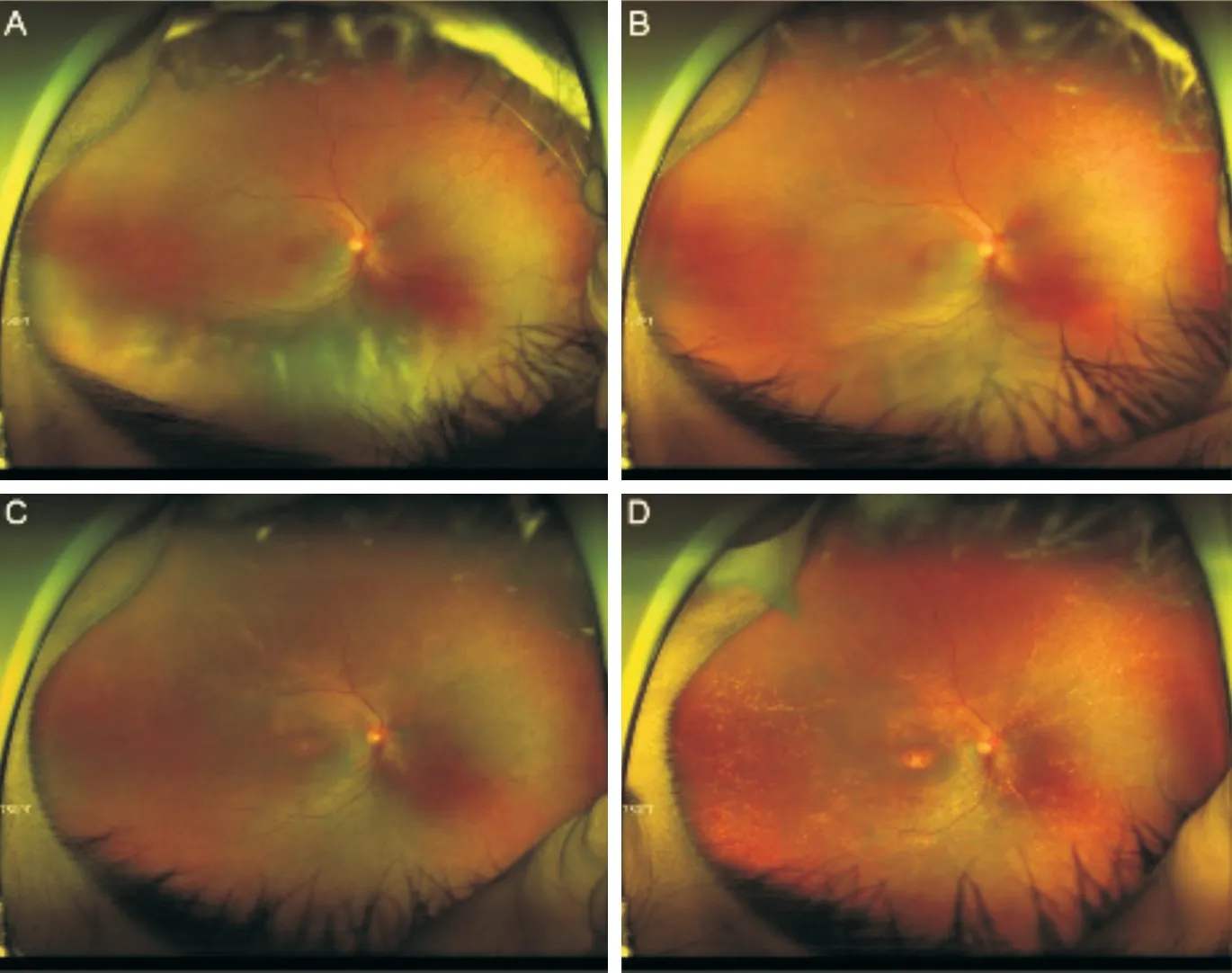
Figure 2 Follow-up fundus photographs of the right eye A: Two courses of corticosteroid pulse therapy, 3-month adalimumab therapy,and 11-month systemic immunosuppressive treatment did not result in resolution of the subretinal fluid and choroidal detachment; B-D:Results of three consecutive posterior sub-Tenon triamcinolone acetonide injections showing complete resolution of the subretinal fluid and choroidal detachment.
Case 2A 46‐year‐old man was referred for treatment of a 4‐month history of peripheral annular choroidal detachment with serous retinal detachment in the right eye. He was diagnosed with suspected unilateral VKH disease and received systemic corticosteroid treatment at a previous hospital.Although he initially showed improvement in peripheral annular choroidal detachment and serous retinal detachment,a steroid taper led to aggravation of his condition. The patient’s medical history was unremarkable. Examination upon presentation showed no neurological or dermatological abnormalities. Slit‐lamp examination revealed no cells in the anterior chamber or anterior vitreous in either eye. Fundus examination revealed 360° peripheral annular choroidal detachment in the right eye (Figure 3A). Optical coherence tomography revealed subretinal fluid, intraretinal, subretinal,and choroidal hyper‐reflective dots, a slightly wavy RPE line in the right eye, and choroidal thickening without patchy vessels in both eyes (Figure 3B). B‐scan ultrasonography revealed mild thickening of the choroid without the “T” sign in both eyes (Figure 3C). The ocular axial length was 23.1 mm in the right and 23.3 mm in the left eye. On UWF fluorescein angiography, multiple window defects, and dye leakages at the posterior pole and the posterior margin of choroidal detachment were observed in the right eye (Figure 3D). One site of leakage near the upper temporal vascular arcade was observed in the left eye.
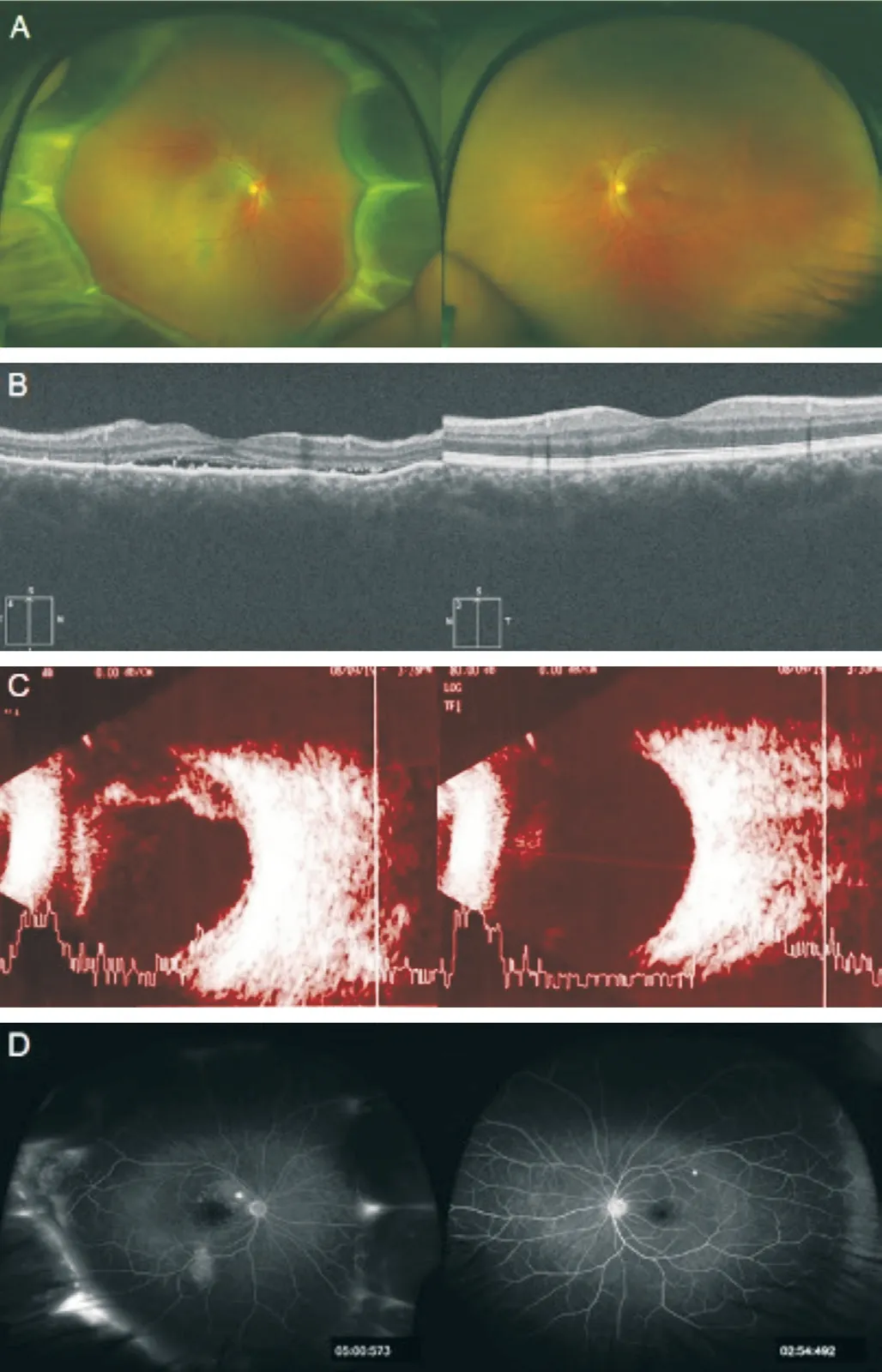
Figure 3 Images at initial visit A: A 360° peripheral annular choroidal detachment in the right eye; B: Choroidal thickening without patchy vessels in both eyes and subretinal and intraretinal fluid, intraretinal,subretinal, and choroidal hyper-reflective dots in the right eye; C: A low reflective mild thickening of the choroid without the “T” sign in either eye; D: Multiple window defects and dye leakages at the posterior pole and at the posterior margin of the choroidal detachment in the right eye; one site of leakage is observed in the left eye.
He was treated with high‐dose intravenous corticosteroid(methylprednisolone 1 g/d) for 3d and followed by oral prednisolone (1 mg/kg). Thereafter, oral prednisone was reduced by 5 mg per week in combination with the initiation of immunomodulation with oral mycophenolate mofetil 1000 mg twice daily. This systemic immunosuppressive treatment was continued for 5mo, during which time local treatment including intravitreal dexamethasone implant injection, intravitreal bevacizumab injection, and focal laser photocoagulation were performed. After treatment, subretinal fluid was resolved but peripheral annular choroidal detachment persisted in this patient (Figure 4A). Owing to the poor response to systemic immunosuppressive treatment, UES appeared to be a more probable diagnosis, and surgical treatment was planned.However, PSTA (40 mg/1.0 mL) injection was attempted and led to near‐complete absorption of the peripheral annular choroidal detachment (Figure 4B). The patient developed a posterior subcapsular cataract, 4mo later with aggravation of peripheral annular choroidal detachment (Figure 4C). Two additional PSTA (40 mg/1.0 mL) injections with 3 month‐interval resulted in complete absorption of peripheral annular choroidal detachment. Peripheral annular choroidal detachment did not recur after cataract surgery and following withdrawal of systemic immunosuppressive treatment for 6mo (Figure 4D).

Figure 4 Follow-up fundus photographs of the right eye A:Corticosteroid pulse therapy, intravitreal dexamethasone implant placement, intravitreal bevacizumab injection, focal laser photocoagulation, and 5-month systemic immunosuppressive treatment did not achieve complete resolution of the choroidal detachment;B-D: Two consecutive posterior sub-Tenon triamcinolone acetonide injections led to complete resolution of the choroidal detachment.
DISCUSSION
Several pathophysiological mechanisms are implicated in the pathogenesis of annular choroidal effusion with serous retinal detachment. UES involves relative obstruction to venous outflowviathe vortex veins secondary to thickened sclera, which results in choriocapillaris congestion and alteration in the transmural hydrostatic pressure gradient, which favors suprachoroidal space fluid retention[6]. Increased choroidal permeability, intrinsic choroidal changes, and decreased scleral permeability may individually contribute to the pathogenesis of choroidal effusion[7], which may also be attributable to a relatively short axial length because choroidal thickness and scleral rigidity are shown to be greater in eyes with a shorter axial length[8].
Choroidal inflammation, which causes hyperpermeability of the choriocapillaris results in fluid and albumin extravasation into the extravascular space and finally into the suprachoroidal space in VKH disease, posterior scleritis, and sympathetic ophthalmia[9]. Additionally, a thickened choroid layer may cause mechanical compression of the vortex veins, followed by choroidal outflow obstruction, increased extravascular fluid retention,and choroidal detachment[10]; dilated choroidal veins observed on UWF indocyanine green angiography in previous studies,as well as in the current study, support this conclusion[2].UES is a diagnosis of exclusion; therefore, other causes of annular choroidal effusion and serous retinal detachment,including VKH disease, posterior scleritis, sympathetic ophthalmia, and tumor metastasis should initially be ruled out.However, differential diagnosis is challenging, particularly in patients with early‐stage disease. Treatment response may serve as a diagnostic clue; for example, VKH disease, posterior scleritis, and sympathetic ophthalmia usually respond to systemic immunosuppressive treatment. However, refractoriness to systemic immunosuppressive treatment presents a diagnostic dilemma. In such cases, it is necessary to distinguish between the possibility of insufficient immunosuppression or misdiagnosis, which often necessitates surgery, such as UES.Posterior sub‐Tenon steroid injection, which delivers a high concentration of steroids near the posterior segment of the globe ensures entry of a high concentration of steroids into the posterior segment (which shows significant inflammation)viatrans‐scleral absorption. Posterior sub‐Tenon steroid injections achieve higher intraocular concentrations of steroids than those obtainedviasystemic administration, with minimal risk of systemic adverse effects[11]. These injections do not alleviate the underlying etiology of annular choroidal effusion in UES which is relative obstruction to venous outflowviathe vortex veins secondary to thickened sclera. As a result,I was able to rule out UES and diagnose my patients with choroidal inflammation such as VKH disease. Insufficient immunosuppression may have contributed to resistant annular choroidal effusion and serous retinal detachment, which responded to higher intraocular concentrations of corticosteroid delivered by PSTA injections in my patients. However, since posterior sub‐Tenon steroid has a limited duration of action,additional injections or systemic immunosuppressive treatment may be required in some cases, like my patients.
In this study, I report two cases of annular choroidal detachment resistant to systemic immunosuppressive treatment that responded to PSTA injections. This approach was associated with favorable treatment outcomes and avoided unnecessary surgery.
ACKNOWLEDGEMENTS
Foundation:Supported by the Hallym University Medical Center Research Fund and the National Research Foundation of Korea (NRF) grant funded by the Korea government (MSIT;No.2021R1G1A1093576).
Conflicts of Interest: Ma DJ,None.
杂志排行
International Journal of Ophthalmology的其它文章
- Visual perception alterations in COVID-19: a preliminary study
- COVID-19 pandemic impact on ocular trauma in a tertiary hospital
- Apolipoprotein A1 suppresses the hypoxia-induced angiogenesis of human retinal endothelial cells by targeting PlGF
- Comparison of vegetable oils on the uptake of lutein and zeaxanthin by ARPE-19 cells
- Identifying a novel frameshift pathogenic variant in a Chinese family with neurofibromatosis type 1 and review of literature
- Recurrence risk factors of intravitreal ranibizumab monotherapy in retinopathy of prematurity: a retrospective study at one center