Efficacy of electroacupuncture for patients with dry eye syndromes: a randomized controlled trial
2022-12-28ZHANGDan张丹ZHAOYan赵嬿YANGYanting杨延婷Xiaoxu刘晓旭ZHAOYue赵越SHZheng施征HONGJue洪珏Jie刘婕MAXiaopeng马晓芃
ZHANG Dan (张丹), ZHAO Yan (赵嬿), YANG Yanting (杨延婷), LⅠU Xiaoxu (刘晓旭), ZHAO Yue (赵越),SHⅠ Zheng (施征), HONG Jue (洪珏), LⅠU Jie (刘婕), MA Xiaopeng (马晓芃)
1 Laboratory of Acupuncture-moxibustion and Ⅰmmunology, Shanghai Research Ⅰnstitute of Acupuncture and Meridian, Shanghai 200030, China
2 School of Acupuncture-moxibustion, Tuina and Rehabilitation, Yunnan University of Traditional Chinese Medicine, Kunming 650500, China
3 Department of Acupuncture and Moxibustion, Guang’anmen Hospital, China Academy of Chinese Medical Sciences, Beijing 100053, China
Abstract
Keywords: Acupuncture Therapy; Electroacupuncture; Point, Cuanzhu (BL2); Point, Taiyang (EX-HN5); Dry Eye Syndromes;Quality of Life; Emotional Regulation; Randomized Controlled Trial
Recently, with a continuously rising incidence, dry eye syndromes (DES) have become a common ophthalmological disease[1-2]. In 2017, the International Dry Eye Workshop (DEWS) redefined DES as a multifactorial disease of the ocular surface characterized by a loss of homeostasis of the tear film accompanied by ocular symptoms, in which tear film instability and hyperosmolarity, ocular surface inflammation and damage, and neurosensory abnormalities play etiological roles[3]. DES usually causes obvious subjective eye symptoms, including dryness, irritation, pain, and burning or itchy sensation,which severely affect the quality of life (QOL) and may lead to emotional disorders, even the loss of living or working capabilities[4-5]. Thus, finding a safe, effective treatment to mitigate the ocular symptoms and improve the QOL of patients with DES is urgent.
Currently, topical use of artificial tear drops is taken as one of the most common solutions for DES despite possible mechanisms and clinical classifications, though the consistency of its effectiveness and safety expect further observation[6]. Meta-analyses have shown that compared with artificial tear drops, acupuncture has a more significant effect on treating DES[7-10].Furthermore, acupuncture can improve tear secretion and tear film stabilization. With gentle action and consistent effectiveness, this treatment has been wellaccepted by the patients. Based on acupuncture,electroacupuncture (EA) has been used to treat diseases by connecting needles with electrical stimulation, which provides more intensive stimulation to points to improve local blood circulation[11]. Topical electrical stimulation was reported to be able to regulate the function of the ocular surface in DES[12-13].Therefore, it is worth trying to discover whether EA can further enhance the efficacy of acupuncture in treating DES.
We adopted this randomized controlled clinical trial to evaluate the efficacy of acupuncture combining low-frequency electrical stimulation in treating patients with DES by observing the changes in multiple aspects,including subjective symptoms, tear secretion, tear film stability, QOL, and emotional status. Taking acupuncture as the control, this study aimed also to discover whether additional low-frequency electrical stimulation can improve the efficacy of acupuncture in treating DES,thus providing clinical evidence for using acupuncture plus low-frequency electrical stimulation to treat DES.
1 Materials and Methods
1.1 Study design
This was a single-center, randomized, parallelcontrolled clinical study conducted in China. It aimed to discover whether low-frequency electrical stimulation can reinforce the efficacy of acupuncture in treating DES.This trial was approved by the Ethics Committee of Yueyang Hospital of Integrated Traditional Chinese and Western Medicine, Shanghai University of Traditional Chinese Medicine (Approval No. 038, 2014).Participants were recruited from the DES specialist clinic of Shanghai Research Institute of Acupuncture and Meridian between July 1, 2014 and August 31, 2015.Figure 1 shows the process of the trial.
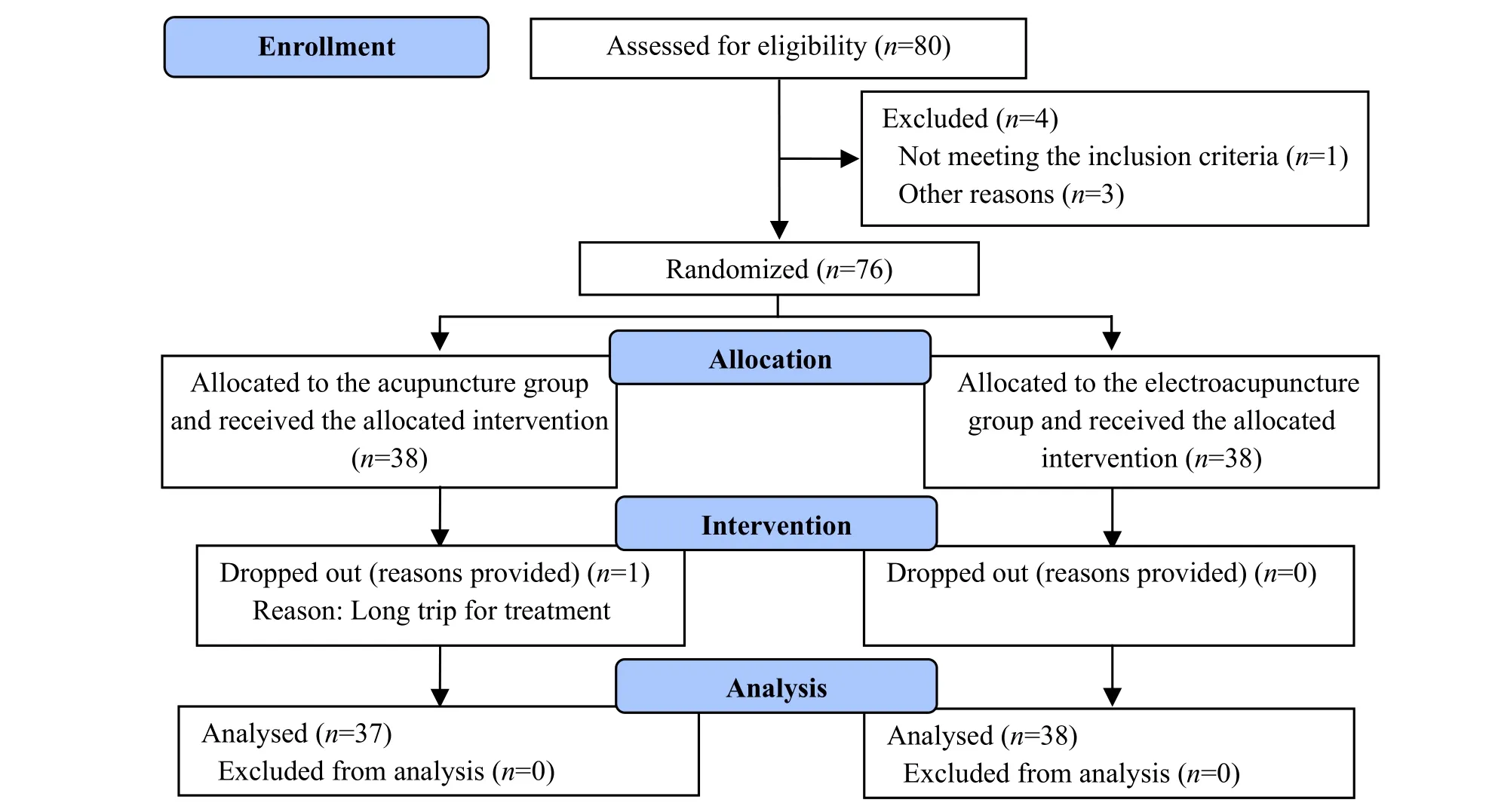
Figure 1 Flow chart of the study
1.2 Diagnostic criteria
TheExperts’ Consensus about Clinical Diagnosis and Treatment of Dry Eye[14]was referred to diagnose DES:presence of one of the subjective eye symptoms, such as dryness, irritation, burning sensation, fatigue,discomfort, and change in vision, and tear-film break-up time (TF-BUT) ≤5 s or Schirmer tear test-1 (STT-1)(without topical anesthesia) ≤5 mm in 5 min or a positive cornea fluorescein staining (CFS) test plus one of the subjective eye symptoms, such as dryness,irritation, burning sensation, fatigue, discomfort, and change in vision, and TF-BUT >5 s, but ≤10 s or STT-1(without topical anesthesia) ≤10 mm in 5 min.
1.3 Inclusion criteria
Participants were included according to the following inclusion criteria: conforming to the diagnostic criteria of DES; aged between 18 and 65 years; willing to join in the study; signed the informed consent form.
1.4 Exclusion criteria
Patients in the following conditions were excluded:Sjögren syndrome; coupled with other ocular diseases;active ocular lesion or ocular surgery during the previous 3 months; on medications for ocular diseases,either oral or external use; pregnant or breast-feeding women; with severe systemic diseases involving cardiovascular or cerebrovascular system or liver, kidney,or hematopoietic system; accompanied by mental diseases.
The included cases were not involved in the evaluation of efficacy if the following conditions occurred: poor compliance and failure to accomplish the whole intervention; using medications that may affect efficacy evaluation; severe adverse events (not involved in efficacy evaluation but recorded).
1.5 Randomization and blinding
In this study, a simple random allocation method was applied. Eligible patients were randomly assigned to receive acupuncture combining low-frequency electrical stimulation or acupuncture alone at an equal ratio.Randomization numbers were generated using the SPSS version 18.0 statistical software. Each number was written on a piece of card and put into a numbered opaque envelope. Each participant was given an envelope at the recruitment by following their visiting sequence. If the number was even, the participant would be allocated to the acupuncture group (AG), and if the number was odd, the participant would be allocated to the EA group (EAG). The examiners and statisticians were blinded to group allocation.
1.6 Intervention
The point selection was according to the previous reports and summarized over long-term clinical practice based on traditional Chinese medicine theory, generally used for all patterns of DES. For each patient, 11 points,namely, Cuanzhu (BL2), Taiyang (EX-HN5), Sizhukong(TE23), Sibai (ST2), Fengchi (GB20), Baihui (GV20), Hegu(LI4), Zusanli (ST36), Guangming (GB37), Sanyinjiao(SP6), and Taichong (LR3) were used. Figure 2 shows the point locations. The points other than those prescribed were not allowed. Furthermore, moxibustion, cupping,herbs, or other therapies were not allowed either.Acupuncture was performed by one specific licensed acupuncturist with more than 10 years of clinical experience.
In the EAG, the patients received acupuncture and low-frequency electrical stimulation. Periocular points,Cuanzhu (BL2), Sizhukong (TE23), Taiyang (EX-HN5), and Sibai (ST2), were punctured by disposable filiform needles of 0.30 mm in diameter and 25 mm in length,while the other points, Fengchi (GB20), Baihui (GV20),Hegu (LI4), Zusanli (ST36), Guangming (GB37),Sanyinjiao (SP6), and Taichong (LR3), were punctured by needles of 0.30 mm in diameter and 40 mm in length(Yunlong Medical Appliances Co., Ltd., China). After standard sterilization, Cuanzhu (BL2), Sizhukong (TE23),Taiyang (EX-HN5), and Sibai (ST2) were needled with swift twirling and lifting-thrusting manipulations applied after insertion until eyeballs became moist. Fengchi(GB20), Baihui (GV20), Hegu (LI4), Zusanli (ST36),Taichong (LR3), Guangming (GB37), and Sanyinjiao (SP6)were needled with twirling manipulation applied for 30 s after Deqi (sensation of soreness, numbness,distention, or radiating, which is considered to indicate effective needling) was obtained. HAN’s EA appliance(HANS-100A, Nanjing Jisheng Medical Science and Technology Co., Ltd., Nanjing, China) was then connected with bilateral Cuanzhu (BL2) and Taiyang(EX-HN5), with a continuous wave, frequency of 2 Hz,and current intensity of 1-2 mA. The stimulation should be within the patient’s tolerance. The needles were all retained for 30 min. The needles were then removed carefully, and the needled areas were pressed with sterile cotton balls to prevent bleeding. In the AG, the patients received the same acupuncture treatment without electrical stimulation. For both groups, the intervention was conducted 3 times a week for 4 weeks.
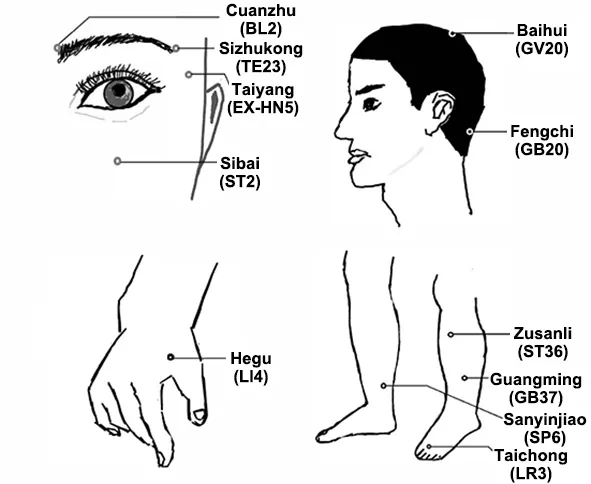
Figure 2 Location of the points
1.7 Outcome assessment
1.7.1 Primary outcomes
The primary outcomes included the ocular surface disease index (OSDI), STT-1, and TF-BUT. The ocular symptoms, visual function, and environmental factors were majorly estimated using a 12-question scale[15-16].Each item was scored 0-4 points, and the aggregate score = the sum of all component scores × 25 ÷ the number of answered questions. The aggregate score ranges from 0 to 100 points. The higher the score, the more serious the symptoms. The patients accomplished this assessment on their own. Tear secretion was measured by STT-1 (without topical anesthesia). In this test, a strip of filter paper of 5 mm × 35 mm, which has a scale on it, was gently placed inside the inferior fornix at the outer one-third. The paper was removed 5 min later, and the moisture amount was measured. A decrease in tear secretion was confirmed when the paper was moistened <10 mm[17]. In the test of TF-BUT,fluorescein sodium ophthalmic strips (Tianjin Jingming New Technological Development Co., Ltd., China) were used to dye the eye, which was then examined by a split lamp (66 Vision Tech Co., Ltd., China) to measure the time till the appearance of the first dry spot on the cornea. To obtain a mean value, the examination was repeated 3 times. An unsteady tear film lasts <10 s, and an abnormal tear film lasts < 5 s[18]. This test was also performed by the same doctor.
1.7.2 Secondary outcomes
Other parameters were used as the secondary measurements. After the examination of TF-BUT, the CFS test was run. Under a split lamp, eyes with corneal abrasions will present spotted dye. The test result was scored by a 12-point method with the cornea divided into 4 quadrants: no dye scored 0, mild dye scored 1,moderate scored 2, and severe scored 3. Thus, the total score ranges from 0 to 12 points. The higher the score,the severer the corneal damage[19]. Corneal sensitivity(CS) was tested using a specific apparatus (Luneau Technology, France), with a filament of 0.12 mm in diameter and 60 mm in length. Patients were asked to look forward. Meanwhile, the doctor held the apparatus to perpendicularly touch the center of the cornea with the end of the filament. The positive test result was defined as a slight bending of the filament and the patient’s feeling of a foreign object. The test started with the maximal length, at a reduction of 5 mm each time, until a positive result was obtained. The readings were then recorded[20]. A value of <60 mm indicates a decreased sensitivity. The lower the value,the worse the CS. Each test was examined by the same doctor.
The QOL was evaluated using the short-form 36-item health survey (SF-36)[21-22], which consists of 8 domains,including physical functioning, physical role functioning,bodily pain, general health perception, vitality, social role functioning, emotional role functioning, and mental health. The score ranges from 0 to 100 points.The higher the score, the better the result. The state of anxiety and depression was estimated using the hospital anxiety and depression scale (HADS)[23-24]. This scale contains two parts, anxiety and depression, made up of 14 items that are scored 0-3 points each. The score for either anxiety or depression ranges between 0 and 21, and a score of 7 is taken as the demarcation;that is, a value of >7 indicates having anxiety or depression emotions.
In this study, the order of the clinical examinations is as follows: first, TF-BUT was measured, and corneal injury was observed and scored right after fluorescein staining; second, the OSDI questionnaire was completed; then, the corneal sensation was estimated;after that, SF-36 and HADS were done; finally, tear secretion was detected by test papers.
1.8 Adverse events
The evaluation of adverse events was based on the toxic effect grading stipulated by the World Health Organization. The beginning time, symptoms, duration,severity, intervention measure, and ending time of the events were recorded, and their possible association with acupuncture was judged[25]. The adverse events were graded from 1 to 4: grade 1 indicates the absence of any adverse events; grade 2 indicates general safety,and the adverse event did not interrupt the observation,but treatment was unnecessary; grade 3 indicates the existence of safety concern, and the adverse event was moderate and required to be addressed before the continuation of the observation; grade 4 indicates that the observation had to stop because of the presence of the adverse event. Any adverse events or reactions were authentically recorded, and proper treatment was provided accordingly.
1.9 Statistics
All statistical analyses were performed using the SPSS version 18.0 software. The worse eye of each patient was used for statistical analysis. First, the measurement data were run for a normal distribution test. The data in or substantially in normal distribution were presented by mean ± standard deviation (±s); if the data were not in normal distribution, they were presented by median (lower quartile, upper quartile) [M (QL, QU)].The OSDI, STT-1, TF-BUT, CFS, and CS data were in nonnormal distribution, and their between-group and within-group comparisons and the interaction effect(group and treatment) were analyzed by the general linear mixed model. The changes in OSDI, STT-1, TF-BUT,CFS, and CS from baseline were in nonnormal distribution, and their between-group comparisons were analyzed using Mann-WhitneyU-test. The HADS and SF-36 data were in nonnormal distribution, and the post-treatment inter-group comparisons were tested using Wilcoxon test.P<0.05 indicated statistical significance.
2 Results
2.1 Participants recruitment
A total of 80 patients with DES were recruited between July 1, 2014, and August 31, 2015. Four cases(1 case with acute conjunctivitis and 3 with suspected Sjogren’s syndrome) were excluded, and the remaining 76 participants were included and randomized into two groups, with 38 cases in each group. In the AG, 37 cases accomplished the study, and one person dropped out(quit because of living far away). In the EAG, all cases finished the intervention with no dropouts. No significant differences were observed in the ratio of gender, age, or disease duration at baseline between the two groups (P>0.05), indicating the comparability(Table 1).
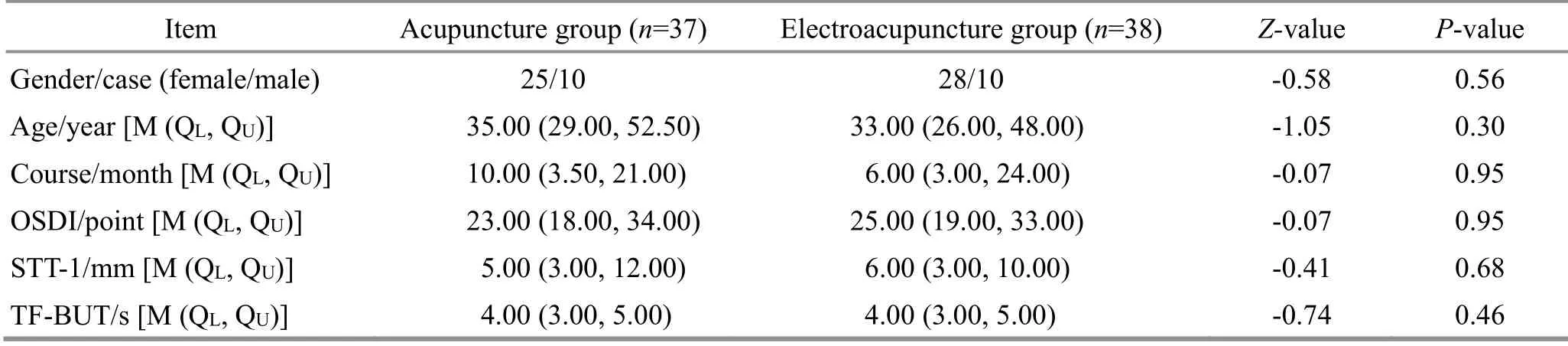
Table 1 Baseline characteristics
2.2 OSDI
After treatment, the OSDI score dropped significantly in both the AG and the EAG, indicating improvements in eye symptoms, as shown in Table 2 and Figure 3. No significant interaction effect was observed between group and time. Additionally, no significant difference was observed between the two groups in the change of OSDI score, as shown in Figure 3.
2.3 STT-1
After treatment, acupuncture did not promote tear secretion in patients with DES, while EA significantly increased tear secretion, as shown in Table 2 and Figure 3. No significant interaction effect was observed between group and time. The result analysis also detected a significant difference in the change of tear secretion between the two groups, indicating a more significant effect in the EAG.
2.4 TF-BUT
Both acupuncture and EA extended the TF-BUT in patients with DES and improved tear film stability, as shown in Table 2 and Figure 3. After treatment, the TF-BUT was extended significantly in both groups. No significant interaction effect was observed between group and time. Furthermore, no significant difference was observed in the change of TF-BUT between the two groups.
2.5 CFS
The two acupuncture approaches improved the repair of the cornea in DES and reduced the CFS score,as shown in Figure 3. Further analysis showed that, of the 15 eyes in the AG with positive CFS at baseline, 10 eyes were improved, while 5 eyes remained at a similar level after treatment. In the EAG, 22 eyes scored >0 in the CFS test at baseline, of which 18 eyes showed improvement, while 4 eyes remained unchanged after intervention. To conclude, in both groups, the CFS score dropped significantly after treatment. Furthermore, no significant difference was observed in the repair of the cornea between the two groups.
2.6 CS
Both acupuncture and EA improved CS, as shown in Figure 3. In the AG, of the 13 eyes measured <60 mm by the CS test at baseline, 11 eyes showed significant improvements after treatment. In the EAG, 8 eyes measured <60 mm by the CS test at baseline all recovered after EA treatment. However, no significant difference was observed in the change of the CS test between the two groups.
2.7 Evaluation of QOL
Both acupuncture and EA improved the QOL of patients with DES, as shown in Table 3. After treatment,the scores of physical role functioning, general health perception, emotional role functioning, and mental health increased in both groups. The physical function,bodily pain, vitality, and social role functioning presented an improving tendency but without statistical significance in the two groups.
2.8 Assessment of anxiety and depression
There was no significant difference in SF-36 or HADS scores between the two groups before treatment. After intervention, the scores of the anxiety domain in HADS dropped significantly in the AG and EAG, while the scores of the depression domain remained the same, as shown in Table 3.
2.9 Adverse events
Rich capillaries are distributed subcutaneously in the face and head, which makes it easy to cause bleeding from acupuncture in periocular, temporal, and crown areas and behind the ears. Therefore, it is necessary to press with sterile cotton balls immediately after the needle removal for a long enough time to prevent bleeding. Otherwise, a bruise may occur. Topical bruise does not interfere with acupuncture and is usually gone within one to two weeks without treatment. In this study, two participants in the AG got a bruise at Cuanzhu (ST2) because of the delayed pressing, and one participant in the EAG got a bruise at Taiyang(EX-HN5) because of the same reason, while another participant had mild ecchymosis at Fengchi (GB20)because of insufficient pressing, which was judged as grade 2 adverse event but did not interfere with the trial. In the later period of the observation, the above patients did not complain of any noticeable discomforts and the lesions healed within one to two weeks.
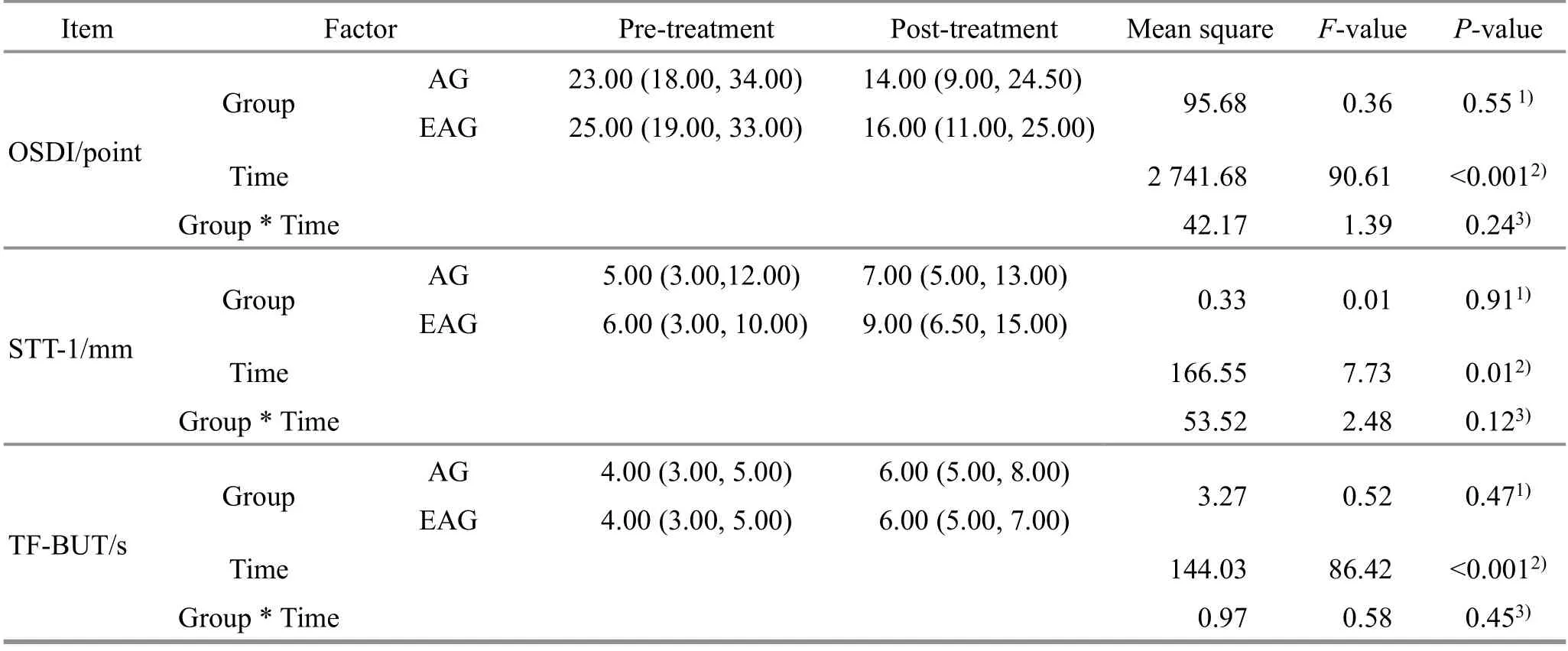
Table 2 Comparison of OSDI, STT-1, and TF-BUT before and after treatment in two groups [M (QL, QU)]
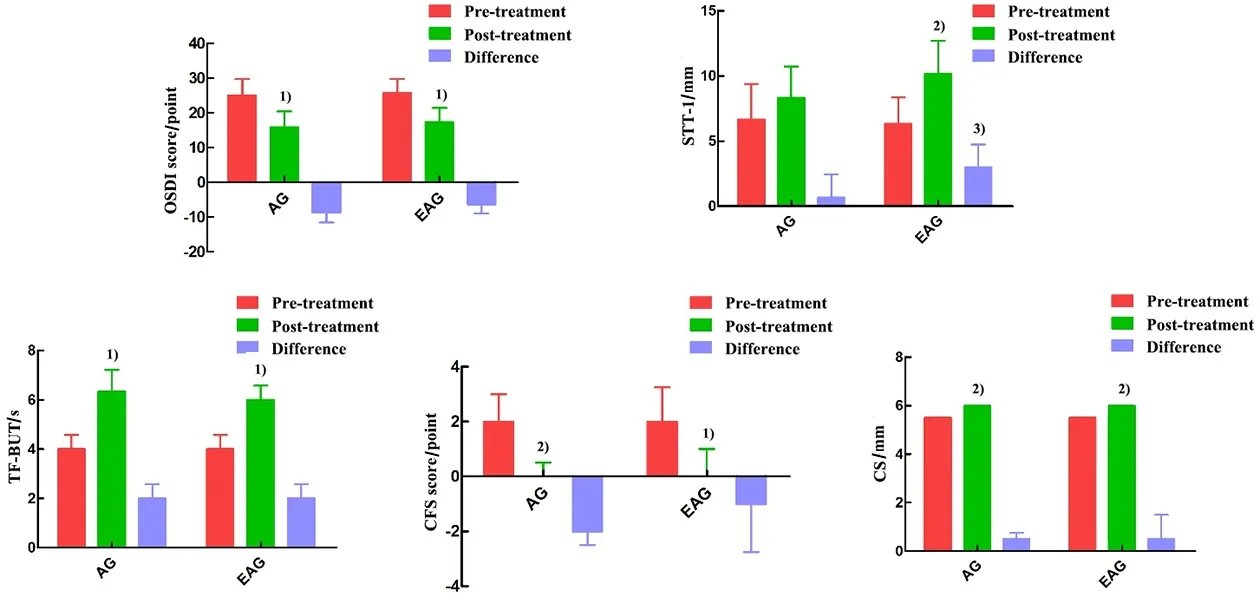
Figure 3 Comparison of OSDI, STT-1, TF-BUT, CFS, and CS before and after treatment

Table 3 Changes in SF-36 and HADS scores [M (QL, QU)] Unit: point
3 Discussion
The focus of clinical research has always been on finding a practical, stable, safe, and effective treatment method for DES. Studies have shown that acupuncture,either used independently or as an adjunct, can produce valid effects in treating DES, majorly manifested by improvement in ocular symptoms,decrease in OSDI score, promotion of tear secretion,and tear film stability[7,10,26-27]. The study results showed that patients with DES showed significant improvements in ocular symptoms, tear film stability,and corneal impairment after acupuncture, which was in accordance with the above reports. Moreover, this study also revealed that acupuncture improved CS, QOL,and anxiety state of patients with DES. Compared with artificial tear drops that depend on the external supply,acupuncture can activate the self-repair ability of the body to improve the topical microenvironment and function of the ocular surface. As an external nonmedication therapy, acupuncture also avoids the safety and dependency concerns that the medicinal artificial tear drops may have[10]. Hence, it is worth recommending that acupuncture is a conventional treatment for DES.
Recently, electrical stimulation to periocular areas has been considered a novel treatment for DES due to its positive regulation on the production of tears, tear film stability, hyperosmolarity, corneal repair, and lipid secretion[12-13,28]. Based on acupuncture combining electrical stimulation of various parameters (frequency,intensity, waveform, and time length), EA enhances the effect of acupuncture and displays a prominent advantage in alleviating pain and improving microcirculation and neuromuscular function[29-32].Therefore, it attracted our attention to see whether EA can elevate the effect of acupuncture in treating DES. In this study, we compared two types of acupuncture in treating DES. The results showed that EA improved ocular symptoms, ocular surface function, QOL, and anxiety state, and its effect was more significant in increasing tear secretion compared with acupuncture.DES occurs when either eyes do not produce enough tears or tears evaporate too quickly; decreased tear production and tear film instability are the key features of the two types of DES, respectively. Thus, this study may indicate that EA can enhance the clinical efficacy of increasing tear secretion.
In this study, a total of 75 participants were included for the statistical evaluation of therapeutic efficacy by strictly following the randomized controlled design with two arms. By adopting subjective questionnaires (OSDI,SF-36, and HADS) and objective tests (STT-1, TF-BUT,CFS, and CS), this trial comprehensively observed the efficacy of acupuncture and EA in treating DES from the aspects of ocular surface function and QOL, providing reliable evidence for the use of EA in elevating the efficacy of acupuncture. Although some previous studies have reported the efficacy of EA in treating DES,they more or less had some shortcomings, such as small sample size, insufficient outcome measures, improper controls, or unclear description of randomization method[33-35]. In this study, the problems were addressed by offering comparatively sufficient and convincing evidence to confirm the significance of using EA to treat DES. Meanwhile, the processes of test,treatment, and statistical analysis were all discrete to guarantee the objectivity of the observation and analysis, thus providing reliable results and conclusions.
The observation of CS showed that both EA and acupuncture ameliorated CS of patients with DES,taking the lead in verifying the treatment efficacy of the two types of acupuncture in treating DES from the perspective of neural regulation. Compared with the visual analog scale that reflects the eye discomfort intensity in a subjective way, the CS test can more objectively determine the CS and neural function of patients with DES and study the possible mechanism of the control of tear production and the action of acupuncture[36]. In 2017, DEWS initially emphasized the crucial role of abnormal neurosensation in the onset of DES. Undoubtedly, the corneal nerve is the key component in the reflex arc of lacrimal and accessory lacrimal glands in producing tears. Abnormal CS has been found in patients with DES; that is why corneal nerve dysfunction is considered a causing factor of decreased tear production and DES[37-38]. Besides,impaired corneal nerve is hard to be separated from pain and hypersensitivity of the eye[39]. The study results suggest that the regulation of acupuncture therapy (including EA) on ocular symptoms and ocular surface function may link with the repair of the corneal nerve. However, the conclusion still expects further research.
It has been pointed out that the relief of ocular symptoms and the improvement of QOL should be the fundamental goal of clinical treatment of DES compared with the recovery of functional indicators[40]. In this study, the effect of the two types of acupuncture on QOL and mood of patients with DES was also observed.It has been found that DES sufferers have higher scores of Pittsburgh sleep quality index and HADS compared with patients with other eye diseases and have a higher risk of experiencing insomnia and emotional disorders[24]. In 2012, KIM T H,et al[7]found no significant change in DES-related QOL after the intervention of acupuncture. Nevertheless, the present study discovered significant improvements in physical role functioning, general health perception, emotional role functioning, mental health, and anxiety after acupuncture treatment (including EA), indicating that acupuncture can effectively elevate the general QOL and release anxiety. We suspect that the differences in points selection, acupuncture skill, and stimulation dose should be the cause of the controversial results. Further analysis showed that the two types of acupuncture produced equivalent effects on SF-36 and HADS scores,which indicates that based on the same acupuncture protocol, electrical stimulation fails to enhance the efficacy in improving QOL and anxiety. However, neither EA nor acupuncture produced a significant effect on the depression state, which may be due to the different features of the two emotional states. Anxiety is a type of somatic neurosis, while depression belongs to emotional dysfunction[41-42]. The latter may require longer treatment with a combination of points for regulating the mind, which also needs more studies to verify.
4 Conclusion
This study aimed to verify the treatment effect of both acupuncture and EA on treating DES, by the improvements in ocular symptoms, TF-BUT, cornea repair, QOL, and anxiety state. EA shows an advantage in promoting tear secretion. It has provided some pieces of evidence and materials for how to more effectively and reasonably use EA to treat DES. During the study, the patients all responded well to the two types of acupuncture, and there did not occur any severe reactions except accidental bruises or mild ecchymosis due to improper pressing after needle removal.
EA is better than manual acupuncture in promoting the secretion of tears, suggesting that electrical stimulation can enhance the efficacy in the treatment of DES based on the same acupuncture protocol. However,the efficacy and indications of EA depend much on the parameters, including current intensity, waveform, and stimulation frequency. Although a frequency of 2 Hz,current intensity of 1-2 mA, and continuous wave were selected in this study, further investigations are expected to understand how EA will act with other parameters, which will be more beneficial to the treatment of DES.
Conflict of Interest
Author MA Xiaopeng is a member of the Editorial Board ofJournal of Acupuncture and Tuina Science, and authors LⅠU Jie and HONG Jue are the editors serving for
Journal of Acupuncture and Tuina Science. The paper was handled by other editors and has undergone a rigorous peer review process. Authors MA Xiaopeng, HONG Jue, and LⅠU Jie were not involved in the journal’s review or decisions related to this manuscript.
Acknowledgments
This study was supported by the Research Projects of Shanghai Municipal Health Bureau (上海市卫生健康委员会项目, No. 202040249, No. 201940130); Shanghai Leading Talent Program (上海领军人才项目, No. 060);Shanghai Sailing Program (上海市青年科技英才扬帆计划项目, No. 19YE1445000).
Statement of Informed Consent
Ⅰnformed consent was obtained from all individual participants.
Received: 19 October 2021/Accepted: 23 February 2022
猜你喜欢
杂志排行
Journal of Acupuncture and Tuina Science的其它文章
- Clinical observation of Tiao Shen Tong Du Tuina in promoting neuropsychological development of premature infants
- Clinical observation of acupuncture combined with sitting-position knee-adjustment manipulations for patellofemoral arthritis
- Clinical observation of acupuncture and moxibustion for functional dyspepsia due to Yang deficiency of the spleen and stomach
- Clinical study of acupuncture combined with medication for the elderly with Alzheimer disease
- Effects of herbal cake-partitioned moxibustion on the expression of thyroid autophagy-related factors LC3B and Beclin-1 in rats with autoimmune thyroiditis
- Effects of Tuina on serum creatine kinase and skeletal muscle mitochondria in delayed onset muscle soreness model rats