Vaccine-associated myocarditis: a case report and summary of the literature
2022-11-15JoshuaDavisLaurenJennings
Joshua Davis, Lauren Jennings
1 University of Kansas School of Medicine, Wichita 67214, USA
2 Vituity, Wichita 67214, USA
3 American Red Cross in Hazelwood, Missouri 63042, USA
Dear editor,
Myocarditis is a known complication of vaccines for COVID-19, particularly mRNA vaccines. While it is rare,the exact incidence of vaccine-associated myocarditis is unknown. Proponents of personal choice in vaccination decisions often cite the risk of myocarditis as a reason one might choose not to receive the COVID-19 vaccination.Herein, we describe a case of focal myocarditis associated with the Pfizer-BioNTech COVID-19 vaccine and review the literature on the incidence and risk of COVID-19 vaccine-associated myocarditis.
CASE
A 24-year-old male with a past medical history of seizure disorder presented to the emergency department with a chief complaint of chest pain. The patient woke up in the morning and noted chest pain radiating to his left arm with associated left arm tingling. He did an internet search and was alerted he had symptoms of a heart attack and presented to the emergency department. He had no personal history of coronary disease, hypertension,diabetes, or dyslipidemia. He has no family history of early cardiac disease or sudden death. He had no diagnosed psychiatric conditions, but he believes he may have undiagnosed anxiety. He denies any tobacco use,recent substance abuse, or life stressors. His medications include levetiracetam and oxcarbazepine, and he also has a vagal nerve stimulator. His review of symptoms was negative, including no fever, cough, dyspnea, nausea,vomiting, or sweating. He has not had any recent sick contacts or significant trauma. He received his second Pfizer-BioNTech COVID-19 vaccine 3 d ago.
On physical examination, the patient appears anxious but is in no distress. His vital signs included a heart rate of 78 beats per minute, respiratory rate of 18 breaths per minute, blood pressure of 129/77 mmHg (1 mmHg=0.133 kPa), oral temperature of 37.2 °C, and oxygen saturation(SpO2) of 100% on room air. His heart, lung, abdomen,and pulse examination revealed no abnormalities. The inspection and palpation of the chest was normal.
On arrival, an electrocardiogram (ECG) was obtained and is presented in Figure 1. ECG showed normal sinus rhythm with concave upward ST segment elevation in leads II, III, aVF, and V4-V6. There was ST depression in lead aVR and subtle ST depression in leads VII and VIII. Spodick’s sign (a down-sloping of the TP segment commonly seen in pericarditis) was also present as well as PR depression. No prior ECG was available for comparison.
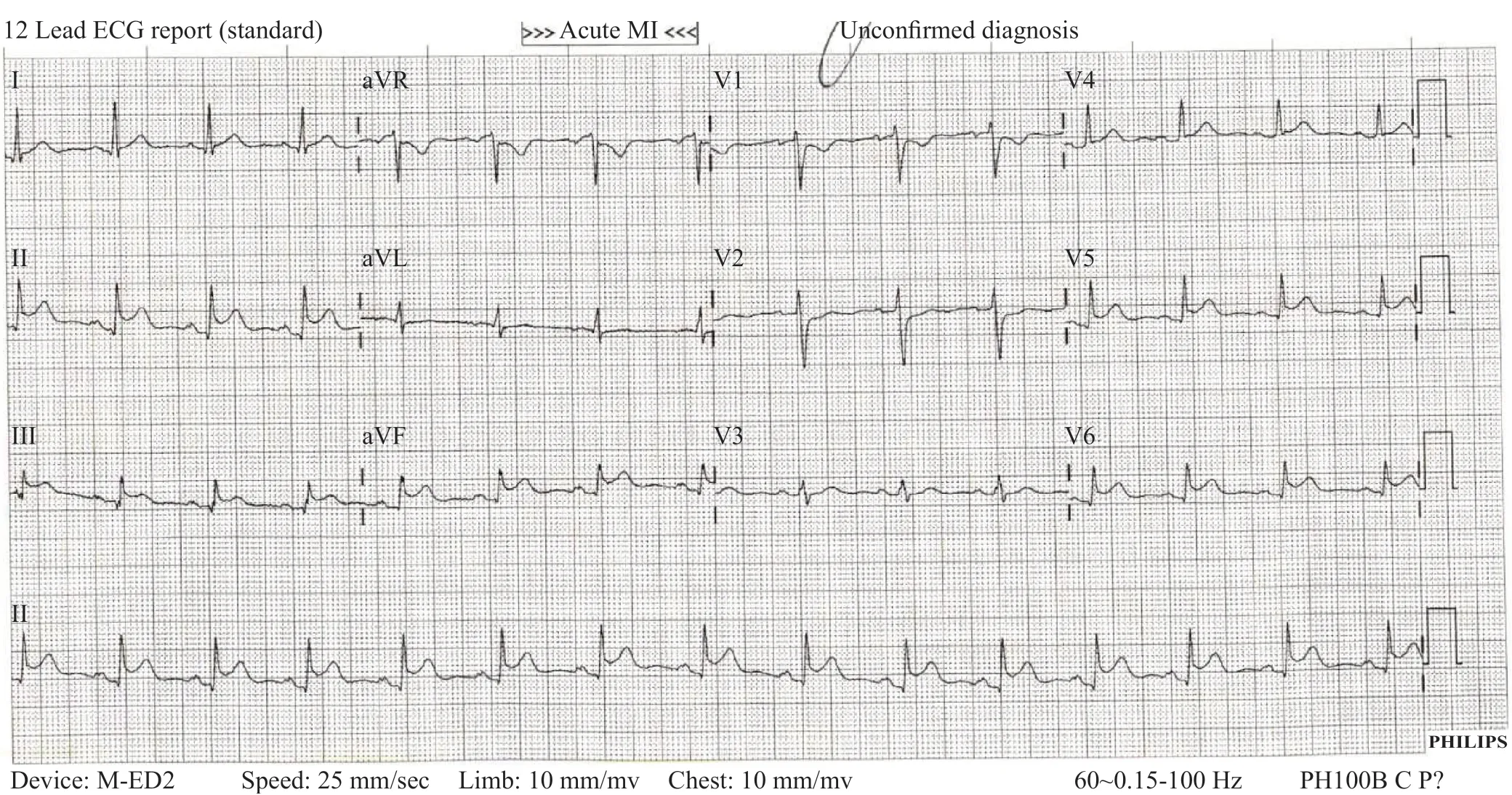
Figure 1. The electrocardiogram of the patient on emergency department arrival. MI: myocardial infarction.
The patient was discussed with the cardiology department at the local referral hospital. The cardiologist recommended transfer for urgent catheterization to rule out occlusive coronary artery disease. The patient was given 324 mg of aspirin, started on a heparin infusion, and transferred to the referral center. In the meantime, labs resulted and were significant for a troponin I level of 9.01 ng/mL (normal <0.04 ng/mL) and a white blood cell count of 14,200 cells/µL (normal 4,000-10,000 cells/µL).
The patient arrived at the outside hospital, and a repeat ECG was obtained, which was largely unchanged.His repeat troponin I was 14.70 ng/mL. The patient was taken for cardiac catheterization where he was found to have no significant coronary disease and a right coronary artery fistula to the coronary vein, felt to be an incidental finding. Echocardiography showed an ejection fraction of 45% and focal hypokinesis of the apical inferior wall.
The patient was diagnosed with myopericarditis and admitted to the hospital. Magnetic resonance imaging (MRI) was contraindicated due to the presence of his vagal nerve stimulator, and both MRI and endomyocardial biopsy were considered unnecessary given the clear clinical picture. His troponin I peaked at 24.42 ng/mL on hospital day 2. His C-reactive protein(CRP) was elevated at 4.9 mg/dL, and his erythrocyte sedimentation rate (ESR) was normal at 5 mm/h. He was started on oral colchicine 0.6 mg. He then had a serum“myocarditis panel” for antibodies to Coxsackievirus,Echovirus, Influenza, andChlamydia pneumoniae, all of which were negative. He also had a nasopharyngeal multiplex polymerase chain reaction (PCR) respiratory viral panel that was negative and a separate negative COVID-19 PCR test. He was discharged on hospital day 3 with no significant chest pain for over 24 h with a diagnosis of vaccine-associated myocarditis.
DISCUSSION
Pfizer-BioNTech and Moderna were given emergency use authorization (EUA) by the U.S. Food and Drug Administration (FDA) in December 2020 for the prevention of COVID-19 in adults 16 years and older. Since then, the Pfizer-BioNTech vaccine has been granted EUA for children as young as 5 years old.Myocarditis has increasingly become recognized as a complication associated with both COVID-19 infection and vaccination against COVID-19, particularly with mRNA vaccines. In May 2021, the Centers for Disease Control and Prevention (CDC) described a link between myocarditis and the two mRNA vaccinations, as reported in the Vaccine Adverse Event Reporting System.[1]Subsequently, in June 2021, the FDA added a warning label about this risk.[2]Cardiac MRI is generally useful for the definitive diagnosis of myocarditis and pericarditis.MRI findings in myocarditis associated with mRNA vaccination against COVID-19 show similar findings to other causes of myocarditis, i.e., early and late gadolinium enhancement and myocardial edema.[3]However, MRI was contraindicated and was not performed in this case because a vagal nerve stimulator was in place for his seizure disorder.
The typical presentation for peri-myocarditis associated with vaccination against COVID-19 is a young male who presents with chest pain 3 d after receiving the second dose of an mRNA vaccination.[4,5]They often have a positive troponin I level and ECG changes suggestive of peri-myocarditis, i.e., diffuse concave upward ST elevation with PR depression. The case described above is unique in that the myocarditis appears to have been focal. Thus, coronary angiography was pursued, which showed normal coronaries. One review of 17 cases of COVID-19 vaccine-induced myocarditis noted that 13/17 patients (76%) had a coronary angiography performed and all of them had no obstructive lesions.[6]The ECG showed ST elevation only in the inferolateral leads, with reciprocal depression in aVL, and the echocardiogram showed focal hypokinesis of the inferior apical wall.
Several case reports and case series have documented myocarditis and pericarditis associated with mRNA vaccines for COVID-19.[7]More rarely, myocarditis after adenovirus (Johnson and Johnson) vaccination against COVID-19 has also been reported.[8]Population studies have shown that there is an increased risk of myocarditis,particularly in young males, after the second dose of the vaccine.[9]The mechanism for vaccine-induced myocarditis remains unclear. When biopsy or autopsy is performed on these patients, there appears to be a predominance of macrophages, sometimes admixed with eosinophils, plasma cells, and B cells.[10]Some proposed mechanistic hypotheses include molecular mimicry of the spike protein and selfantigens, direct immune activation from mRNA or lipid nanoparticles, and activation of previously subclinically dysregulated immune systems or cytokine pathways in certain predisposed individuals. The predominance of this disease in young males suggests a relationship between autoantibodies and sex hormone differences.Myocarditis associated with COVID-19 infection may have an autoimmune component, but mechanisms such as microthrombosis, endothelial dysfunction, and sepsisrelated cardiomyopathy have also been suggested. Given the novel nature of both COVID-19 and mRNA vaccinations,all of these proposed mechanisms remain speculative.
The rates of myocarditis after a second mRNA dose ranged from 5.8 to 24 per one million doses. Most reported cases are mild and resolve on their own with a few brief hospitalizations of less than 4 d.[11]Alternatively, the rates of myocarditis following COVID-19 infection are up to 20-fold higher than those following vaccination.[12,13]Thus,while peri-myocarditis is associated with the second dose of mRNA vaccination, the risk is significantly lower than that of infection with COVID-19.[14]
CONCLUSION
We present a case of focal myocarditis following mRNA vaccination for COVID-19. Myocarditis is a known rare complication of mRNA vaccination, but this risk is significantly lower than the risk of myocarditis following COVID-19 infection. Although it is highly likely, causation with the vaccine cannot be proven.
Funding:There is no funding to report for this study.
Ethical approval:Not needed.
Conflicts of interest:We have no conflicts of interest, financial or other, to declare regarding this manuscript.
Contributors:JD and LJ drafted the manuscript, edited for key content, take responsibility for the data, and approve the final version for publication.
杂志排行
World journal of emergency medicine的其它文章
- Factors related to early and rapid assessment of in-hospital mortality among older adult trauma patients in an earthquake
- Comparing the demographic data and outcomes of septic shock patients presenting to teaching or non-teaching metropolitan hospitals in the United States
- The procalcitonin-to-cortisol ratio is a potential prognostic predictor in sepsis with abdominal source:a retrospective observational study
- Early changes in white blood cell, C-reactive protein and procalcitonin levels in children with severe multiple trauma
- Exploratory COVID-19 death risk score based on basic laboratory tests and physiological clinical measurements
- Medical services for sports injuries and illnesses in the Beijing 2022 Olympic Winter Games
