The interaction effect of grip strength and lung function(especially FVC) on cardiovascular diseases: a prospective cohort study in Jiangsu Province,China
2022-10-17JiaLiLIUJiaQiWANGDanWANGYuQINYongQingZHANGQuanYongXIANG
Jia-Li LIU ,Jia-Qi WANG ,Dan WANG ,Yu QIN ,Yong-Qing ZHANG ,Quan-Yong XIANG,,✉
1.School of Public Health,Southeast University;Nanjing,Jiangsu Province,China;2.Department of Chronic Non-communicable Disease Control,Jiangsu Province Center for Disease Control and Prevention;Nanjing,Jiangsu Province,China
ABSTRACT OBJECTIVE Lung function and grip strength (GS) are associated with cardiovascular disease (CVD),but whether these risk factors interact to affect CVD is unknown.This study aimed to explore the interactions between lung function and GS with major CVD (defined as fatal/non-fatal myocardial infarction,stroke,and heart failure) incidence.METHODS We conducted a prospective cohort study on the Chinese population in Jiangsu Province.Cox proportional hazards models were used to explore the associations between GS,lung function,and major CVD incidence.RESULTS A total of 5967 participants were included in our study;among them,182 participants developed major CVD.Participants with low forced vital capacity (FVC) had a higher risk of major CVD (hazard ratio (HR)=1.45;95% confidence interval(CI): 1.05-2.01;P <0.05) compared with normal FVC.The risk of major CVD incidence (HR=0.54;95% CI: 0.35-0.83;P <0.01) was significantly lower in participants with high GS than in individuals with low GS.The interaction between FVC and GS for major CVD incidence (P=0.006) was statistically significant.Compared with normal FVC participants with high GS,low FVC participants with low GS had the highest risk of major CVD incidence (HR=2.50;95% CI: 1.43-4.36;P <0.01).CONCLUSION Among people with low FVC,the risk of major CVD is lower with high GS.Participants with low FVC and low GS have the highest risk of major CVD.Therefore,more attention should be paid to the incidence of major CVD in individuals with low FVC,especially those who have lower GS.
Cardiovascular disease (CVD) comprises heart and vascular disease and is the main cause of global mortality and disability.In developing countries,the social and economic burden due to cardiovascular events increases yearly.[1]Some studies have shown that low muscle function as measured by grip strength (GS)[2]is associated with an increased risk of all-cause mortality,cardiovascular mortality,and CVD.[3,4]A study from the Prospective Urban Rural Epidemiology (PURE) (n=139,691 adults aged 35-70 years median follow-up for four years) showed that GS was inversely associated with all-cause mortality,cardiovascular mortality,and CVD.[4]However,muscle function decline is correlated with aging,and aging is getting more attention in modern society.Sarcopenia refers to the age-related loss of muscle mass during healthy aging and curtailing active.[5]This loss of muscle function appears to be accelerated in people with low lung function.Low GS has been associated with the risk of low lung function.[6,7]A case-control study (58 participants with stable chronic obstructive pulmonary disease(COPD) and 25 participants without respiratory problems) showed that people with COPD have lower GS.[8]Low lung function has also been associated with future risk of mortality and CVD.[9-11]However reports on the association between lung function and increased risk for CVD have conflicted in several studies.A study demonstrated that forced expiratory volume in one second (FEV1) and forced vital capacity (FVC) were associated with CVD.[11]However,a previous study pointed out that FEV1 and FVC had not associated with CVD in patients with COPD.[12]Because skeletal muscle function is associated with health outcomes,this lower muscle function could contribute to the greater risk of developing comorbidities in people with low lung function.So far,no studies have investigated the associations of muscle strength with CVD among patients with low lung function.Given the gaps in current research,we aimed to examine the associations between lung function and GS for the risk of major CVD incidence in Jiangsu province,China,in a 10-year prospective cohort study of 5967 Chinese participants aged 35-70 years.
METHODS
Study Design and Participants
The data came from a cohort study in Jiangsu Province,China.Multi-stage sampling method,community-household-individual,was used to select participants representing Jiangsu Province populations.The first stage,nine counties or districts were selected according to the geographic regions(North,Midland,and South area of Jiangsu Province),urban/rural location,socioeconomic status,and probability proportional to size.In the second stage,four townships were selected using random number tables from each county or district.The third stage,four neighborhood communities or administrative villages were selected with probability proportional to size,and 50 households were randomly chosen from each neighborhood communities or administrative villages.Finally,one person who was 35-70 years old was recruited for this study using a Kish selection table.[13]A total of 7200 participants were recruited in this study at baseline.Socio-demographic factors (age,sex,education,and occupation),health-related variables (anthropometric indicators,including height,weight),medication history,disease history,lifestyle factors (total physical activity (PA),tobacco and alcohol use),laboratory data and lung function data at baseline were collected from Jan 2008 to Dec 2008 by a standard protocol.The participants were follow-up per year from Jan 2009 to Dec 2019.In this study,the incidence of major CVD (defined as fatal/non-fatal myocardial infarction,stroke,and heart failure) was determined by hospital diagnosis under certain criteria.[11]Lung function and GS were the exposures of interest.In our analyses,we included all outcome events known until Dec.2019.We excluded 268 participants who lost to follow-up;174 who did not have complete data on weight,height,age,GS,lung function,blood pressure;349 who had CVDs,chronic respiratory disease and other severe diseases at baseline (such as cancer or their life expectancy less than one year);189 who did not have complete data on tobacco use,alcohol use,education,PA,occupation;and 253 who did not have complete data on laboratory including serum total cholesterol (TC),triglyceride (TG),high density lipoprotein cholesterol (HDL-C),low density lipoprotein cholesterol (LDL-C),fasting blood glucose (FBG).Eventually,a total of 5967 participants were analyzed in this study.Participants were categorized into six groups according to their lung function parameters(normal/low) and GS status (low/moderate/high).
Blood Sample Collection and Laboratory Tests
A 12-h fasting blood sample was collected to measure FBG,TC,TG,LDL-C,and HDL-C at baseline investigation.Blood samples were centrifuged and transferred into a -70°C refrigerator or -180°C liquid nitrogen tanks for storage for testing within one month.FBG was measured by an accredited lab using glucose oxidase or hexokinase methods within 12 h.TG,TC HDL-C and LDL-C were measured using an autoanalyzer (Abbott Laboratories) in Jiangsu Province Center for Disease Control and Prevention,which was certificated by The National Laboratory Certification of China.
Lung Function Measurement
Lung function was measured with a portable spirometer (MicroGP;Micro Medical,Chatham,IL,USA),without spirographs.According to the criteria of American Thoracic Society,[14]the data from participants with two or more acceptable spirometry performances were selected,and the highest FEV1 and FVC values were analyzed.To avoid the influence of age,sex,height and weight on the measured values of lung function,the results were expressed as the ratio of the measured values to the predicted values (i.e.,FEV1%=FEV1/predicted FEV1).The regression formula of the predicted value of lung function in East China[15]was used to calculate the predicted value of lung function for each participant.Low FEV1 was defined as FEV1% <80% and low FVC was defined as FVC% <80%.[16]
Grip Strength Measurement
GS was measured three times for each hand using a Jamar dynamometer (Sammons Preston,Bolingbrook,IL,USA).The arm was positioned at the side of the body and the dynamometer was held with the elbow flexed to 90°.The participant was asked to squeeze the device as hard as possible for 3 s.The measurement was repeated twice more at an interval of at least 30 s.GS was calculated by taking the mean of the maximal values of non-dominant and dominant GS.GS is related to sex and age,we thus categorized sex-and age-specific GS into low(<25thpercentile),moderate (25th-75thpercentile),and high (>75thpercentile) strength subgroups.[17]
Definition
Blood pressure (mmHg) was read using an automated sphygmomanometer (Omron HEM-757;Omron,Kyoto,Japan).Hypertension was defined as having a diagnosis of hypertension,receiving antihypertension treatment,or having an average measured systolic blood pressure (SBP) of at least 140 mmHg and/or diastolic blood pressure (DBP) of at least 90 mmHg.Dyslipidemia was defined as receiving anti-dyslipidemia treatment,TC ≥ 6.22 mmol/L,and/or TG ≥ 2.26 mmol/L,and/or LDL-C≥ 4.14 mmol/L,and/or HDL-C ≤ 1.04 mmol/L.PA was evaluated using the International Physical Activity Questionnaire,in which four main types of PA(including occupation,housework,transportation,and recreation) were recorded in minutes per week.The total PA was computed as the sum of these 4 PA types in metabolic equivalent (MET) × min per week,and was classified as low (<600 MET ×min/week),moderate (600-3000 MET × min/week),and high (>3000 MET × min/week).Using a standard questionnaire,information on tobacco and alcohol status was collected,and participants were categorized into never,former (defined as those who had quit more than a year),or current smoker.[18]Alcohol use was defined as having alcohol more than once per month in the past year.[19]Sociodemographic information,such as age,occupation and education was self-reported at baseline.Body mass index (BMI) was calculated as weight divided by height squared.
Ethics Approval and Consent to Participate
Informed consent was written and obtained from all participants.The study protocol was approved by the ethical review committee of the Jiangsu Province Center for Disease Control and Prevention.Individual person’s data has not been contained in any form (including individual details,images or videos) in this manuscript.The procedures were in accordance with the standards of the ethics committee of Jiangsu Provincial Center for Disease Control and Prevention and with the Declaration of Helsinki (1975,revised 2013).
Statistical Analysis
Frequencies and percentages for categorical variables and means with standard deviations for continuous variables were used to describe the baseline characteristics of participants.Analysis of variance and χ2test were used to compare differences between groups.Cox proportional hazard model was used to analyze the effect of independent GS,independent lung function,and a combination of the above two on major CVD.Linear trends in GS were tested using the median value within each GS level.The results were reported as hazard ratios (HRs) together with 95% confidence interval (CI).The proportional hazards assumption was checked by visual inspection of log-log plots.To investigate whether levels of GS modified the associations between lung function and major CVD,multiplicative interaction between lung function and age-and sex-specific categories of GS were assessed in the Cox model.For all analyses,we ran three incremental models.Model 1 was adjusted for age (35-44,45-54,55-70 years) and sex;Model 2 was adjusted for model 1 plus BMI,alcohol use,tobacco use,occupation,PA,and education;Model 3 was adjusted for model 2 plus hypertension,diabetes mellitus,and dyslipidemia.All analyses were conducted using SPSS 25.0.A 2-sidedP-value of less than 0.05 was considered significant.
RESULTS
Baseline Characteristics of the Population Based on Lung Function and GS levels
Among the 7200 participants recruited representatively from Jiangsu Province,5967 eligible participants were included in our analysis,of which 2612(43.8%) were classified as low FVC and 2671 (44.8%)were classified as low FEV1.During the follow-up of 10 years,182 participants developed major CVD.The baseline characteristics of the participants based on FVC status and the level of GS were shown in Table 1.3338 (55.9%) were women.More people aged 35 to 44 in the normal FVC groups than in the low FVC groups.The mean BMI of the normal FVCgroup was lower than that of the low FVC group,and the high GS group had the highest BMI,followed by the moderate and low GS group.The proportion of high PA,secondary education level in the normal FVC group was higher than in the low FVC group,and the proportion of high PA level in the low GS group was the lowest.The prevalence of hypertension and diabetes mellitus in the normal FVC group were lower than that in the low FVC group.The baseline characteristics of BMI,prevalence of hypertension and diabetes mellitus in the participants based on FEV1 status and GS level were consistent with those based on FVC status and GS level (Supplementary Table 1).
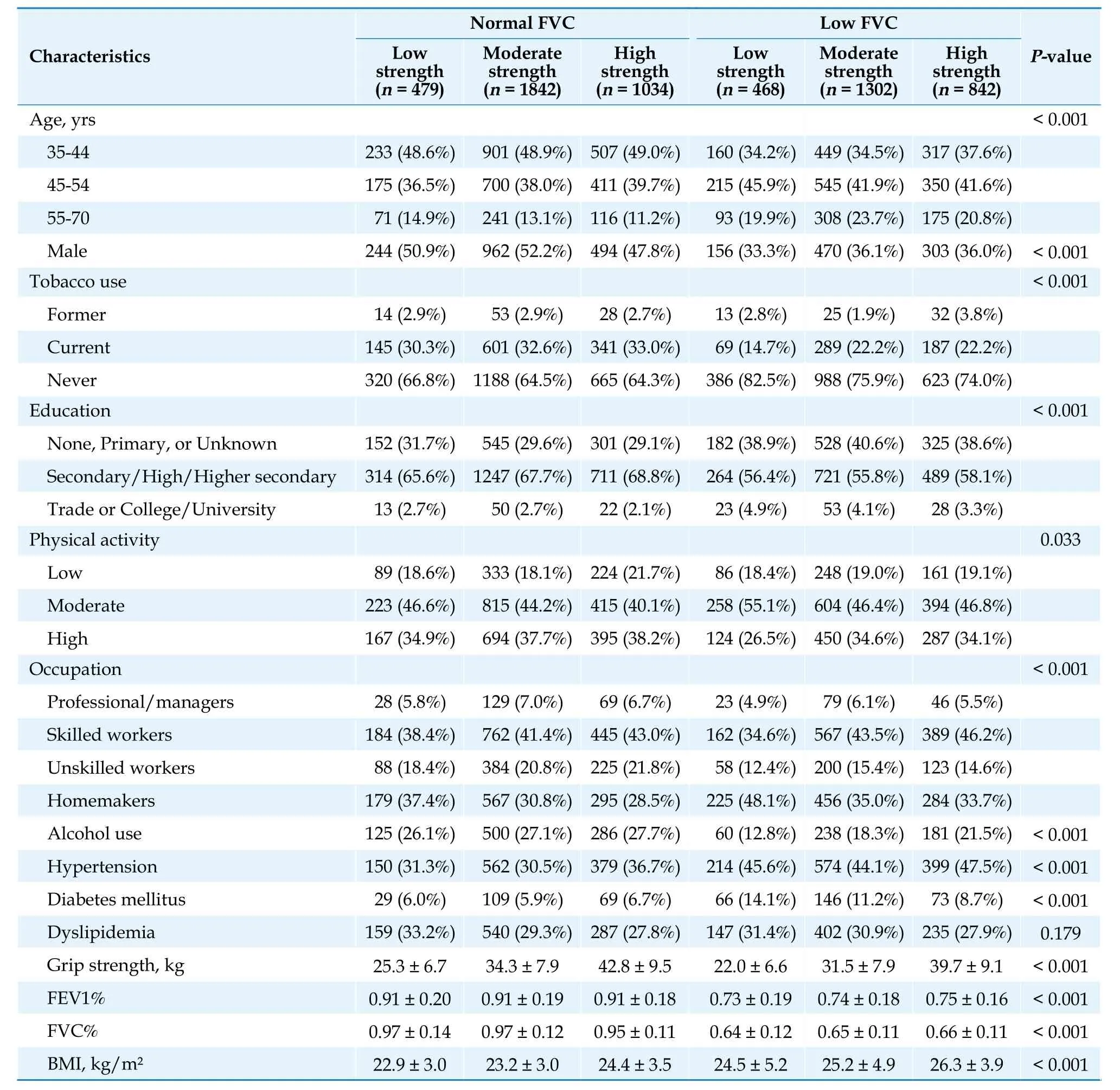
Table 1 Participant’s baseline characteristics by GS and FVC status.
Association of Lung Function and GS with Major CVD
The risk of major CVD was only significantly higher in participants with low FVC (Table 2).Compared with normal FVC participants,the HR was 1.45 (P<0.05) for major CVD incidence adjusted for covariates.In addition,participants with high GS had a significantly lower risk of major CVD.Compared with low GS,the HR was 0.54 (P<0.01) for major CVD incidence in high GS.When participants with obstructive impairment (defined as FEV1/FVC ratio <0.70) were removed (Table 3),the associations of lung function,GS,and major CVD were consistent with Table 2.
The Event Rate of Major CVD According to GS and the Lung Function Status During Follow-up
As the results of FEV1 had no significant association with the major CVD in the Cox proportional hazards models analyzed (Table 2),we classified the major CVD by the level of GS and FVC status,the results are summarized in Table 4.In the low FVC status,as the GS level decreased,the event rate of major CVD significantly increased (P<0.01).In the normal FVC status,the event rate of major CVD among three GS level were not a significant difference.The highest event rates of major CVD events(6.20%) occurred in the group with low FVC and low GS.
HRs of Major CVD According to GS and Lung Function Status
The HRs for major CVD incidence by GS and FVC status are summarized in Table 5.The interaction between FVC and GS for major CVD incidence(P=0.006) was statistically significant in Model 3.In stratified analysis,only in low FVC status,thehigh GS had a significantly association with major CVD incidence (P<0.01).When the participants with obstructive impairment (defined as FEV1/FVC ratio <0.70) were removed (Table 6),the results were consistent with Table 5.Major CVD incidence risk across combined categories of GS and FVC status is shown in Figure 1.Compared with normal FVC participants with high GS,low GS had the highest risk of major CVD incidence (HR=2.50;95% CI: 1.43-4.36;P<0.01) among low FVC participants in Model 3,followed by moderate GS for the risk of major CVD incidence (HR=1.67;95% CI:1.02-2.74;P<0.05).However,the risk of major CVD events in high GS had no significant difference among low FVC participants compared with normal FVC participants with high GS.
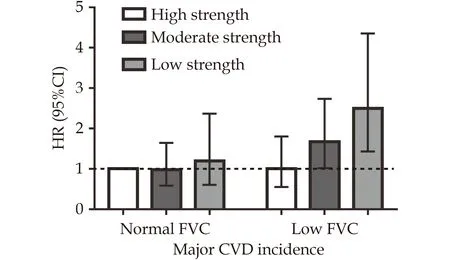
Figure 1 Association of major CVD incidence by FVC status and GS strata.The model was adjusted for age,sex,BMI,alcohol use,tobacco use,occupation,PA,education,hypertension,diabetes mellitus,and dyslipidemia.Participants with normal FVC and high GS were used as the reference group.BMI: body mass index;CVD: cardiovascular disease;FVC: forced vital capacity;GS: grip strength;PA: physical activity.

Table 2 Cox proportional hazards models analyzed of major CVD events by FVC,FEV1 and GS.

Table 3 Cox proportional hazards models analyzed of major CVD events by FVC,FEV1,and GS in participants without obstructive impairment.

Table 4 Major CVD events by GS and FVC status.
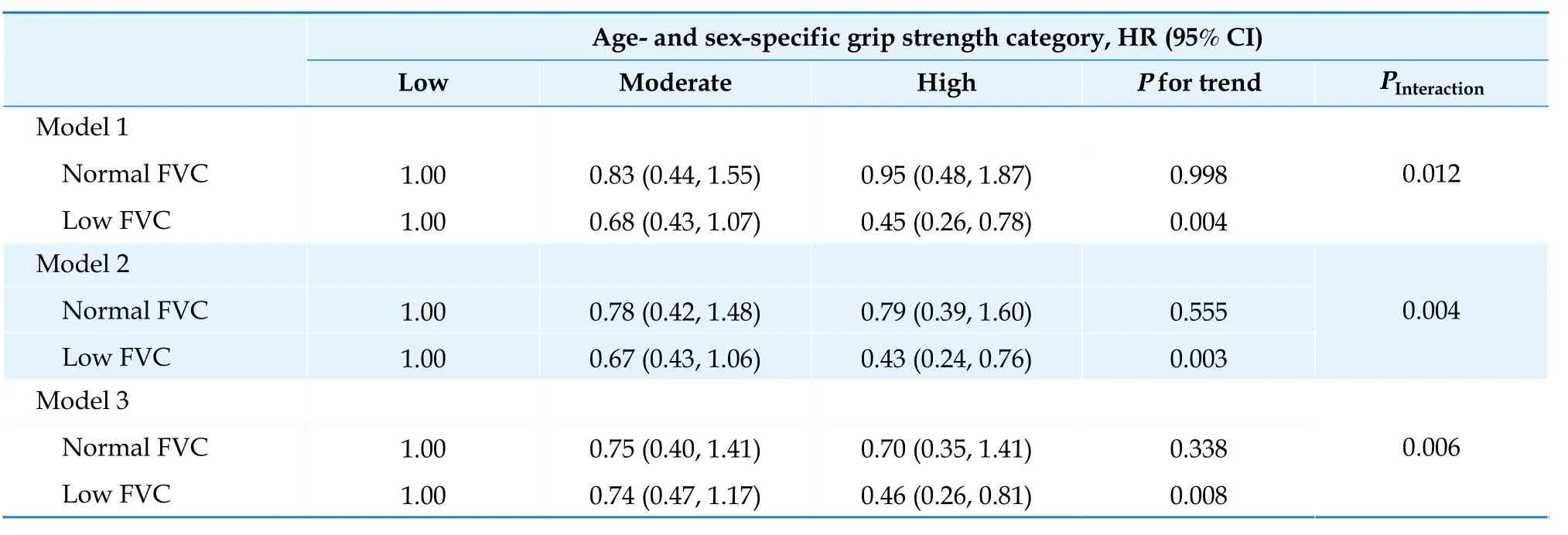
Table 5 Cox proportional hazards models for major CVD incidence in participants with low FVC by GS category.

Table 6 Cox proportional hazards models for major CVD incidence in participants with low FVC by GS category excluding individuals with obstructive impairment.
DISCUSSION
In this prospective study,we demonstrated the effect of independent FVC,independent GS and the combination of two on major CVD incidence.FVC and GS levels were inversely associated with major CVD incidence.Compared with normal FVC participants with high GS,low FVC patients with low GS in our study had the highest risk of major CVD incidence.
The relationship between low FVC and the risk of major CVD was in line with previous studies,while FEV1 and the risk of major CVD was inconsistent with previous studies.[9-11]In this study,the association between FEV1 and major CVD was not found.Moreover,this study was consistent with these findings.[12,20]Bikov,et al.[12]demonstrated that FEV1 was not associated with CVD.Another study showed that the risk of CVD was similar between COPD patients with and without accelerated FEV1 decline.[20]The rapid decline in FEV1 occurs in the early stages of the lung disease and FVC declines faster in later disease stages.Previous studies have shown that arterial stiffness increases in subjects with more severe and advanced COPD than in those with mild to moderate COPD.[21,22]In addition,some studies have shown that lower FVC is associated with atherosclerosis,[23,24]which is a recognized underlying cause of CVD.The mechanism of re-duced lung function and arterial stiffness is not fully understood,but their relationship may be linked by a cardiovascular risk factor and systemic inflammation.[25]According to a study that included 21 countries with reference values for GS among healthy adults,[17]we categorized participants in this study into low,moderate,and high GS groups using sex-and age-specific GS cutoffs.GS is a simple,reliable proxy for muscle strength.Compared with low GS participants,high GS participants reduced the risk of major CVD by 46%,but moderate GS did not have a significantly reduced risk of major CVD.These findings were consistent with previous studies,suggesting that low muscle strength was a risk factor for health-related events and can predict the morbidity of CVD.[26,27]Skeletal muscle is the primary protein store and site of glucose disposal[28]and it can provide gluconeogenic precursors that are important for survival as such disease progresses.[29]Studies have shown that structured resistance training is associated with reduced risks of CVD.[30,31]It can promote muscle function and improve CVD risk factors.Our study suggested that improving overall muscle mass of people with low GS may play an important role in the prevention and management of CVD.
To the best of our knowledge,this is the first prospective cohort study to explore the combined effects of GS and lung function on the risk of major CVD incidence in Chinese.In this study,lung function status and GS status were measured at baseline,while major CVD occurred during follow-up,which was in accordance with the temporal association.The current study demonstrated that the association between FVC and GS for risk of major CVD has a significant interaction.FVC is a parameter of lung volume examination primarily affected by respiratory muscles and FEV1 is a parameter of lung volume examination and expiratory flow examination,which is affected not only by respiratory muscles but also by airway patency.[32]One study showed a significant increase in FVC after exercise in people with sarcopenia;however,FEV1 was not significantly increased.[33]Another study demonstrated a similar result.[34]In our study,the risk of major CVD incidence is 2.5-fold higher in low FVC patients with low GS compared to those with high GS with normal FVC.The combined effect of low GS and low FVC was significantly greater than their single effect on major CVD.Skeletal muscle decline is often accompanied by respiratory muscle decline,resulting in decreased lung function and respiratory complications,including atelectasis and ineffective cough.[35,36]These respiratory complications can lead to CVD.[37]In addition,muscle function decline may promotes inflammation,[38]which is a factor contributing to reduce lung function,[23,38]and increase cardiovascular events.[37]These findings are very important for patients with low lung function in secondary prevention,particularly those with low GS.Increasing GS by physical exercise training may benefit low lung function patients who have a prognosis of adverse health outcomes.However,additional well-designed randomized controlled trials are warranted to confirm our findings.
One strength of our study was a prospective study with large sample size.Our study also used high-quality data obtained using a systematic and standardized approach.In addition,our data included a number of potential covariates to illustrate well the relationship between lung function,GS,and major CVD.Nevertheless,there are several limitations to our study.We only had baseline data on GS and lung function information;we did not know whether GS and lung function changed during the follow-up.Our data were from the Jiangsu population,which did not represent the Chinese population well.
In conclusion,low GS and low FVC are associated with a higher risk of major CVD incidence.In the combined analyses,the risk of CVD incidence was highest for people with low FVC and low GS.This finding provides a new reference for preventing and controlling major CVD in low FVC populations.
ACKNOWLEDGMENTS
We thank Prof.Zengwu Wang and Prof.Xin Wang (Division of Prevention and Community Health,National Center for Cardiovascular Disease,Fuwai Hospital),and Prof.Qizhan Liu (School of Public Health,Nanjing Medical University) for their constructive suggestions and the technical support.We thank all the colleagues involved in this survey from the study site.
COMPETING INTERESTS
None.
FUNDING
This work was supported by the Natural Science Foundations of China (81973005);the Natural Science Foundation of Jiangsu Province (BK20151593).
杂志排行
Journal of Geriatric Cardiology的其它文章
- In-hospital outcomes and readmission in older adults treated with percutaneous coronary intervention for stable ischemic heart disease
- A short P-wave duration is associated with incident heart failure in the elderly: a 15 years follow-up cohort study
- Association between heart failure severity and mobility in geriatric patients: an in-clinic study with wearable sensors
- Iatrogenic atrial septal defects after transseptal puncture for percutaneous left atrial appendage occlusion and their hemodynamic effects
- Early identification of STEMI patients with emergency chest pain using lipidomics combined with machine learning
- Complement use of Chinese herbal medicine after percutaneous coronary intervention: a prospective observational study
