lnterventional radiology followed by endoscopic drainage for pancreatic fluid collections associated with high bleeding risk:Two case reports
2022-09-01NingXuLongSongLiWenYiYueDanQiZhaoJingYuanXiangBoZhangPengJuWangYaXuanChengEnQiangLinghuNingLiChai
Ning Xu,Long-Song Li,Wen-Yi Yue,Dan-Qi Zhao,Jing-Yuan Xiang,Bo Zhang,Peng-Ju Wang,Ya-Xuan Cheng,En-Qiang Linghu,Ning-Li Chai
Ning Xu,Long-Song Li,Dan-Qi Zhao,Jing-Yuan Xiang,Bo Zhang,Peng-Ju Wang,Ya-Xuan Cheng,En-Qiang Linghu,Ning-Li Chai,Senior Department of Gastroenterology,The First Medical Center of PLA General Hospital,Beijing 100853,China
Wen-Yi Yue,Department of Radiology,Chinese PLA General Medical School,Beijing 100853,China
Abstract BACKGROUND Endoscopic ultrasound (EUS)-guided transluminal drainage is an advanced technique used to treat pancreatic fluid collections (PFCs).However,gastric varices and intervening vessels may be associated with a high risk of bleeding and are,therefore,listed as relative contraindications.Herein,we report two patients who underwent interventional embolization before EUS-guided drainage.CASE SUMMARY Two 32-year-old males developed symptomatic PFCs after acute pancreatitis and came to our hospital for further treatment.One patient suffered from intermittent abdominal pain and vomiting,and computed tomography (CT) imaging showed an encapsulated cyst 7.93 cm × 6.13 cm in size.The other patient complained of a mass inside the abdomen,which gradually became enlarged.Gastric varices around the ideal puncture site were detected by EUS when we evaluated the possibility of endoscopic drainage in both patients.Interventional embolization was recommended as the first procedure to decrease the risk of bleeding.After that,EUS-guided transluminal drainage was successfully conducted,without vascular rupture.No postoperative complications occurred during hospitalization,and no recurrence was detected at the last follow-up CT scan performed at 1 mo.CONCLUSION Interventional embolization is a safe,preoperative procedure that is performed before EUS-guided drainage in PFC patients with gastric varices or at high risk of bleeding.
Key Words: Interventional embolization;Endoscopic drainage;Endoscopic ultrasound;Pancreatic fluid collections;Gastric varices;Case report
lNTRODUCTlON
Pancreatic fluid collections (PFCs),including walled-off necrosis (WON) and pancreatic pseudocysts (PPCs),are local complications of acute or chronic pancreatitis according to the updated Atlanta classification[1].European Society of Gastrointestinal Endoscopy (ESEG) recommends endoscopic or percutaneous drainage as a first-line therapy for symptomatic PFCs[2].A previous study found that endoscopic transmural drainage is more effective than surgery because of its minimal invasiveness[3].However,the gastric varices and the abundant vessels surrounding PFCs might be ruptured while establishing the tunnel between the stomach and cyst,thus resulting in uncontrollable bleeding that is unresponsive to endoscopic clips or electrocoagulation[4].In the two patients described here,lumenmetal apposing stents were successfully placed to drain PFCs under endoscopic ultrasound (EUS) guidance during preoperative embolization of potential bleeding vessels.Herein,we share our successful experience in the form of two case reports to help endoscopists prevent bleeding during the endoscopic drainage procedure.
CASE PRESENTATlON
Chief complaints
Case 1:A 32-year-old male was admitted to our department with the symptoms of abdominal pain and vomiting.
Case 2:A 32-year-old male with abdominal distension was referred to our hospital for therapeutic management.
History of present illness
Case 1:The patient experienced continuous abdominal pain and vomiting and was sent to the emergency department of our hospital.The symptoms gradually disappeared after fasting and acid suppression.Abdominal ultrasound indicated the presence of cystic lesions in the body of the pancreas.Then,he was transferred to our inpatient area.
Case 2:In December 2020,the patient who was diagnosed with PPC from an outside hospital was admitted to the Department of Hepatobiliary Surgery to undergo open surgery.However,he was unsuitable for the surgical operation because of renal insufficiency.He came to our department for further treatment of PPC until renal function returned to normal in September 2021.
History of past illness
Case 1:Three years ago,he was admitted to a local hospital to receive treatment for severe acute pancreatitis.
Case 2: The patient suffered from acute pancreatitis for the first time five years prior to hospitalization,and recovered after symptomatic treatment.Intermittent pancreatitis occurred frequently between 2017 and 2020.The patient was hospitalized in the intensive care unit,at least once,for severe abdominal pain combined with continuous vomiting and fever.
Personal and family history
Cases 1 and 2: The personal and family histories were unremarkable.
Physical examination
Case 1:Abdominal distension was visible even when the patient lay flat.
Case 2:An obvious mass was palpable in the left upper abdomen,but the size of the mass might not have been evaluated accurately.
Laboratory examinations
Case 1:No pancreatitis-related abnormalities were found by blood biochemical examination.
Case 2:A slight increase in the carbohydrate antigen 125 level was detected by blood biochemical examination,as well as a sharp increase in the carbohydrate antigen 19-9 level.Amylase (501 U/L) and lipase levels (559 U/L) were much higher than normal (normal ranges: 0-150 U/L and 13-60 U/L).
Imaging examinations
Case 1:Contrast-enhanced abdominal computed tomography (CECT) showed a cystic lesion in the body of the pancreas,with a size of 7.93 cm × 6.13 cm (Figure 1A).A cystic lesion of the same size and the presence of blood vessels around the cyst were observed on linear EUS (Figure 2A).
Case 2:A cyst with a maximum diameter of 14 cm was detected by CECT (Figure 1B).Linear EUS showed signs of several vessels around the fundus of the stomach,which may have been a potential puncture site (Figure 2B).
FlNAL DlAGNOSlS
Case 1
Based on the patient’s history of illness and the direct endoscopic visualization of the cystic cavity contents,his diagnosis ultimately concluded as being WON.
Case 2
According to the characterization of the cystic cavity contents,he was diagnosed with PPC.
TREATMENT
Case 1
Coil embolization was performed before the endoscopic drainage (Figure 3A and B).Then the patient was prepared to undergo EUS-guided cystogastrostomy and a lumen-metal apposing stent (LAMS: 16 mm × 26 mm,Micro-Tech Co.,Ltd.,Nanjing,Jiangsu Province,China) placement.
Case 2
Under fluoroscopy guidance,endovascular embolization was conducted first (Figure 3C and D).Four days later,EUS-guided cystogastrostomy and placement of a LAMS were successively performed.
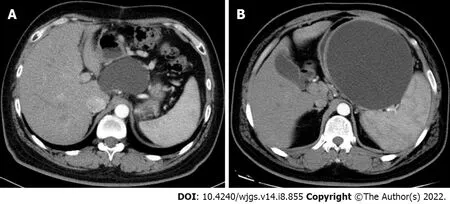
Figure 1 Preoperative images of contrast-enhanced computed tomography.
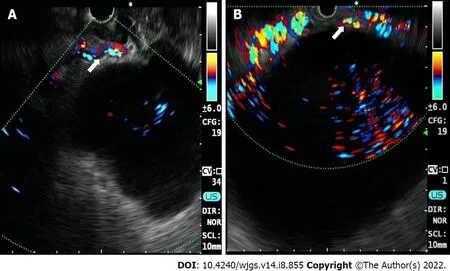
Figure 2 Multiple vasculature (white arrow) detected by Doppler endoscopic ultrasound.

Figure 3 Typical imaging of interventional radiology.
OUTCOME AND FOLLOW-UP
Case 1
Subsequent monitoring showed that the patient’s temperature was maintained within the normal range.However,he experienced unexplained nausea and vomiting during hospitalization after the LAMS was placed.Four days after stent placement,postoperative endoscopic observation showed that the contents were almost fully discharged to the stomach cavity.Thus,after irrigation of the cystic cavity with sterile water only,the stent was retrieved,and thereby eliminated all discomforting symptoms.One month after endoscopic drainage,CECT of the abdomen revealed that WON in the patient has resolved.
Case 2
The patient’s vital signs were stable during hospitalization.Postoperative endoscopy was used to perform direct endoscopic necrosectomy.Sterile water was used to rinse the small amount of liquid content that remained in the cystic cavity followed by withdrawal of the stent.CECT obtained one month after the procedure showed shrinkage of the PPC.No abdominal symptoms or postoperative complications were observed.
DlSCUSSlON
PFCs are local complications of acute pancreatitis that frequently occur more than 4 wk after the onset of pancreatitis[5].Some PFCs patients might suffer from symptoms of abdominal pain,vomiting,and other digestive-related discomfort,but the majority of patients are asymptomatic and their symptoms resolve spontaneously[6].For symptomatic PFCs,especially those that seriously affect normal life,drainage of the collections is vital for effective treatment[7,8].Although there are other drainage methods,endoscopic drainage is minimally invasive and has improved safety and efficacy when compared to open surgery or percutaneous drainage,so endoscopic drainage is recommended as the first-line treatment.
Endoscopic drainage is a well-established therapy for PFCs;however,bleeding complications still haunt endoscopists[9,10].In the past,PFCs associated with gastric varices or abundant surrounding vessels were referred to the surgical department for further treatment[11].Previous studies have reported attempts to treat PFC-associated diseases with high bleeding risks,such as arterial pseudoaneurysms,with a combination of minimally invasive endoscopic and radiological interventions[12,13].However,this combined treatment is rare because of its association with the gastric varices or the surrounding vessels,thus limiting is applicability due to the demand for expertise in interventional radiology and therapeutic endoscopy.
Endovascular embolization,an advanced technique,is the preferred treatment of choice for esophageal or gastric varices and has been widely used to stop and prevent bleeding[14,15].However,clinicians have limited experience in the clinical management of PFCs that present with gastric varices.Moreover,ideal management depends on the patient’s hemodynamic stability[16].The development of interventional radiological techniques has led to better outcomes of hemostasis with angioembolization.One report indicated that angioembolization alone is an effective treatment for a pseudocyst associated with pseudoaneurysms[17].
In the presence of gastric varices or pseudoaneurysms,EUS-guided endoscopic drainage is contraindicated because of the increased risk of vessel rupture[18].In our study,we show that endoscopic drainage combined with coil embolization is an effective treatment for varices.These two patients underwent EUS-guided puncture and a small incision was made in the wall of the stomach and PFC cysts after interventional radiology.No intraoperative complications,such as bleeding or infection,occurred.We did not encounter any complications while removing the necrotic solid debris or the metal stent.However,we did not determine the cause of intermittent nausea and vomiting that occurred in one patient.All symptoms disappeared after the stent was removed.
One limitation is associated with this combined treatment method.For patients with PFCs less than 6 cm,a LAMS cannot be used to establish a tunnel between the two lumens[19].Therefore,EUS-guided endoscopic drainage combined with interventional radiology would not be feasible.
CONCLUSlON
The application of endovascular embolization before EUS-guided endoscopic drainage prevents vessel rupture.This combined treatment has the potential to be a solution for PFC patients with high bleeding risks and warrants further investigation to substantiate its use.
ACKNOWLEDGEMENTS
The authors thank Dr.Yuan K for providing the imaging data.
FOOTNOTES
Author contributions:Xu N and Li LS contributed equally to this manuscript;Chai NL and Xu N contributed to manuscript drafting;Xu N and Yue WY wrote the manuscript;Li LS,Zhao DQ,Xiang JY,Zhang B,Wang PJ and Cheng YX were responsible for the revision of the manuscript for significant content;Chai NL and Linghu EQ were the patient’s endoscopists and reviewed the literature;all authors issued final approval for the version to be submitted.
Supported byNational Natural Science Foundation of China,No.82070682;and Beijing Municipal Science and Technology Commission,China,No.Z181100001718177.
lnformed consent statement:Informed written consent was obtained from the patient for publication of this report and any accompanying images.
Conflict-of-interest statement:There are no conflicts of interest to declare.
CARE Checklist (2016) statement:The authors have read the CARE Checklist (2016),and the manuscript was
prepared and revised according to the CARE Checklist (2016).
Open-Access:This article is an open-access article that was selected by an in-house editor and fully peer-reviewed by external reviewers.It is distributed in accordance with the Creative Commons Attribution NonCommercial (CC BYNC 4.0) license,which permits others to distribute,remix,adapt,build upon this work non-commercially,and license their derivative works on different terms,provided the original work is properly cited and the use is noncommercial.See: https://creativecommons.org/Licenses/by-nc/4.0/
Country/Territory of origin:China
ORClD number:Ning Xu 0000-0002-7770-8731;Long-Song Li 0000-0002-4000-7501;Jing-Yuan Xiang 0000-0002-1755-7978;Bo Zhang 0000-0002-4333-0750;En-Qiang Linghu 0000-0003-4506-7877;Ning-Li Chai 0000-0002-6791-5817.
S-Editor:Yan JP
L-Editor:A
P-Editor:Yan JP
杂志排行
World Journal of Gastrointestinal Surgery的其它文章
- Percutaneous direct endoscopic pancreatic necrosectomy
- Factors associated with hypertension remission after gastrectomy for gastric cancer patients
- 3D laparoscopic-assisted vs open gastrectomy for carcinoma in the remnant stomach:A retrospective cohort study
- Pre-colonoscopy special guidance and education on intestinal cleaning and examination in older adult patients with constipation
- Model established based on blood markers predicts overall survival in patients after radical resection of types II and III adenocarcinoma of the esophagogastric junction
- Over-the-scope-grasper: A new tool for pancreatic necrosectomy and beyond - first multicenter experience
